Abstract
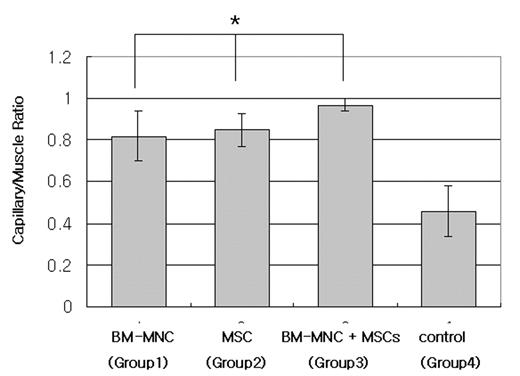
We examined whether the injection of bone marrow mononuclear cells (BM-MNCs) or mesenchymal stem cells (MSCs) might augment angiogenesis and collateral vessel formation in a mouse model of hind limb ischemia. C57BL/6 BM-MNCs were isolated by centrifugation through a Histopaque density gradient and MSCs were obtained from C57BL/6 bone marrow and cultured in low-glucose DMEM media. Unilateral hind limb ischemia was surgically induced in C57BL/6 mice (control; n=4), and autologous BM-MNCs (Group 1; n=4, 1.8±0.2 x107/animal) or MSCs (Group 2; n=4, 1.0±0.14 x106/animal) or BM-MNCs and MSCs (Group 3; n=4, 2.3±0.1 x107 and 1.1±0.21 x106/animal) were transplanted into the ischemic tissue. Six weeks after transplantation, the group 1, group 2 and group 3 had a higher capillary/muscle ratio (0.82±0.12 vs 0.85±0.08 vs 0.97 ±0.03) than control (0.46±0.12, p<0.05) (Fig. 1). This result suggested that direct local transplantation of autologous BM-MNCs or MSCs seems to be a useful strategy for therapeutic neovascularization in ischemic tissues.
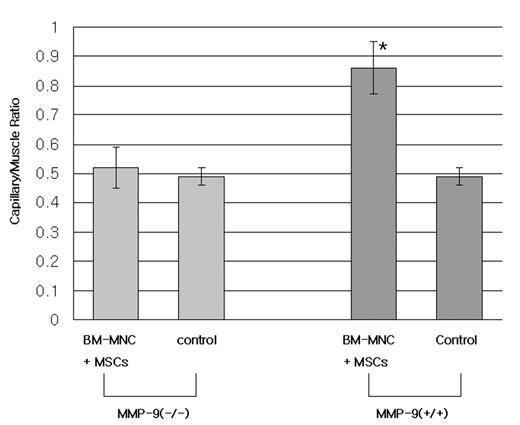
Next, we evaluated whether bone marrow derived stem cells were participated in the process of local injected stem cells forming new vessels. In general, mobilizing stem cells from bone marrow to local site, MMP-9 has been known as an important molecule. So we used the MMP-9 deficient KO mice and wild type, 129SvEv mice were used in the experiments. Autologous BM-MNCs and MSCs were transplanted into the ischemic limb in MMP-9 (−/−) (n=4) after unilateral hind limb ischemia was surgically induced and then the same experiments was done in MMP-9 (+/+) mice (n=4). The number of the injected BM-MNCs and MSCs was 2.2±0.05 x107 and 0.87±0.17 x106/animal in MMP-9 (−/−). And the number of the injected BM-MNCs and MSCs was 2.1±0.17 x107 and 0.98±0.09 x106/animal in MMP-9 (+/+). No difference was seen in the BM-MNCs and MSCs were injected or not (0.52±0.07 vs 0.49±0.03,) in MMP-9 (−/−). But, in the case that BM-MNCs and MSCs were injected, the higher capillary/muscle ratio was seen in MMP-9 (+/+) compared to control (0.86 ±0.09 vs 0.49±0.03, P<0.05) (Fig 2). This data indicated that the mobilization of bone marrow derived stem cells would have an important role in the neovasculrization although the stem cells were injected directly into the muscle of ischemic limb.
Author notes
Corresponding author