Abstract
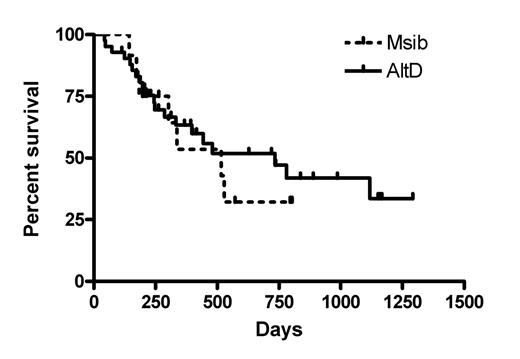
We added Sirolimus to an established conditioning regimen in an attempt to optimize engraftment and anti-tumor effects while minimizing GVHD. 55 patients patients with advanced hematological malignancies (median age 60) received cyclophosphamide (1gm/m2 days −7 and −6) and fludarabine (25mg/m2 days −7 through −3) prior to peripheral blood cell (51 patients) or marrow (4 patients) transplant. All received sirolimus with tacrolimus, both adjusted to 5–15ng/ml, and methotrexate (5mg/m2 days 1,3, 6) immunoprophyllaxis. Tacrolimus was tapered from days 30–45 in matched siblings (Msib -12 patients) and days 40–100 in (most) alternative donor recipients (AltD- unrelated donor or 5/6 matched related cells - 43 patients) without acute GVHD. Median follow-up is 313 days in AltD patients and 337 days for Msib patients. All Msib cells engrafted, whereas 3/43 AltD recipients showed primary graft failure or secondary graft failure (1/43). Msib recipients engrafted more rapidly than those with AltD transplants (p<0.01). For AltD recipients, the CD34 dose had a positive significant effect on donor engraftment - chimerism (p<0.05 for all points up to D100). Median overall and disease free survival was 287 and 230 days respectively for AltD patients and 303 and 167 days for Msib recipients. Amongst AltD patients, 17/43 survive progression free at D114-1167 (median D416), while in MSib patients only 1/12 survives progression free (p=0.0023 ). Two additional patients are disease free after donor lymphocytes (DLI) or withdrawal of immunosuppression in each group. No patient in the Msib group had transplant related mortality (TRM), but in the AltD group there were nine TRMs, including 7 from GVHD (NS). Multivariate analysis showed CD34 dose and donor types had no significant effect on development of progressive disease (PD). However, in general the odds ratio of any PD decreased exponentially as the level of chimerism increased. For example, at D100 the odds of developing PD decreased by 0.699 times when the level of chimerism increased by 0.1. Multinomial logit analysis showed that compared to GVHD death, the odds ratios for PD death decreased exponentially as the level of chimerism increased. In this series of patients with advanced hematological malignancy, Alternative donor cells provided a higher probability of control of disease, albeit with a trend to higher TRM. Higher CD34 cell doses were associated with improved donor engraftment (chimerism) in AltD recipients. For AltD recipients, risk of PD was reduced by increasing donor chimerism, but increasing chimerism is associated with increased risk of death from GVHD. Efforts to improve control of malignancy via more rapid engraftment of donor cells must be tempered with concern regarding potentially severe GVHD.
Author notes
Corresponding author