Comment on Taussig et al, page 4086
In the current issue of Blood, Taussig and colleagues demonstrate that cell surface markers previously thought restricted to mature myeloid cells are expressed on both normal hematopoietic stem cells and leukemia stem cells.
The hypothesis that a rare population of cells that possesses “stem-like” characteristics exists within tumors was proposed more than 4 decades ago. However, identifying, characterizing, and isolating cancer stem cells remain fundamental goals of cancer research. Achieving these goals will provide insight into cancer pathophysiology and permit the development of more effective anticancer therapies. Therefore, information regarding both shared and unique properties of cancer stem cells in relationship to other cancer cells and normal tissues is highly relevant.
Because bone marrow is readily available and easily manipulated, stem cell research is most advanced in the field of hematopoiesis. There are in vitro and in vivo assays capable of identifying stem, progenitor, and mature populations of cells. The application of these techniques to malignancy, such as xenotransplantation of human bone marrow to severe combined immunodeficient (SCID) mice, has provided information regarding the existence of SCID leukemia-initiating cells (SL-ICs). SL-ICs are capable of inducing an acute myeloid leukemia (AML)–like disease in conditioned mice.1 These cells are low in frequency, immunophenotypically primitive, and possess self-renewal capabilities, confirming their similarity to normal hematopoietic stem cells (HSCs).2 However, their relationship to leukemia stem cells (LSCs) capable of human leukemogenesis requires further investigation. Furthermore, functional characterization techniques such as transplantation are limited, and identifying a pattern of cell surface markers unique to LSCs would facilitate therapeutic manipulation. Efforts to identify such an immunophenotypic signature have not resulted in a pattern fully capable of distinguishing leukemic from normal stem cells.3
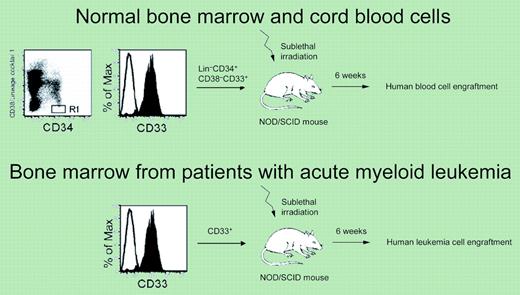
The cell surface markers CD13 and CD33 are considered restricted to mature myeloid cells. Expression of the latter marker on myeloblasts serves as the basis for the antileukemic therapy, gemtuzumab ozogamycin (GO, Mylotarg; Wyeth-Ayerst, Pearl River, NY), a humanized monoclonal antibody directed against CD33 that is covalently attached to the anthracycline, calicheamicin. In an effort to determine whether myeloid markers such as CD13 and CD33 are expressed on normal hematopoietic stem and leukemia stem cells, Taussig and colleagues isolated primitive hematopoietic cells from normal human bone marrow, cord blood, and bone marrow from patients with acute myeloid leukemia (AML) using flow cytometry. Stem cell function was confirmed by injecting cells into conditioned, immunocompromised mice and assessing for the presence of human hematopoietic cells after a period of 6 weeks.
The authors showed that when CD34+ CD38-Lin- cells from normal human bone marrow and cord blood were separated according to CD33 expression, stem cell activity was surprisingly enriched in the CD33+ fraction (see figure). In order to determine whether CD33 is expressed on SL-ICs, bone marrow from patients with AML was sorted according to CD33 expression and injected into conditioned SCID mice. Again, stem cell activity was enriched in the CD33+ fraction (see figure).
In order to determine the functional consequence of blocking CD33, both normal cord blood and AML bone marrow were incubated with a blocking antibody to CD33 prior to transplantation. Compared with unblocked samples, blocking CD33 resulted in diminished engraftment of both normal cord blood and AML bone marrow cells.
Given that CD33 is expressed on normal HSCs, these findings explain the clinical observation that treatment of AML patients with GO not only induces a reduction in myeloblasts, but frequently results in additional cytopenias. Furthermore, because GO is effective in only a portion of patients with AML, these findings suggest that multiple therapies may be required to effectively eradicate LSCs.4
Functional stem cell activity is demonstrated in the CD33+ population of cells from normal bone marrow and cord blood (top) and bone marrow from patients with acute myeloid leukemia (bottom). Figure was adapted from Taussig and Pearce; see the complete figure in the article beginning on page 4086.
Functional stem cell activity is demonstrated in the CD33+ population of cells from normal bone marrow and cord blood (top) and bone marrow from patients with acute myeloid leukemia (bottom). Figure was adapted from Taussig and Pearce; see the complete figure in the article beginning on page 4086.
The emerging field of cancer stem cells provides a challenge to cancer therapeutics: selective and effective manipulation of cancer stem cells. Identification of cell surface molecules and biochemical pathways5 unique to cancer stem cells will facilitate the development of cancer stem cell–directed therapies. Clinical studies such as the GAIN Trial of GO by the Southwest Oncology Group (SWOG) and of bortezomib (Velcade; Millennium Pharmaceuticals, Cambridge, MA) by the Cancer and Leukemia Group B (CALGB) in AML will test whether therapies capable of targeting the cancer stem cell result in clinical benefit. ▪