Abstract
NKG2D is an activating cell-surface receptor expressed on natural killer (NK) cells and some T-cell subsets. Its ligands are primarily expressed on tumor cells. The aim of this study was to determine whether chimeric NK-receptor—bearing T cells would directly kill tumor cells and lead to induction of host immunity against tumors. Chimeric NK receptors were produced by linking NKG2D or DNAX activating protein of 10 kDa (Dap10) to the cytoplasmic portion of the CD3ζ chain. Our results showed that chimeric (ch) NKG2D-bearing T cells responded to NKG2D-ligand–bearing tumor cells (RMA/Rae-1β, EG7) but not to wild-type tumor cells (RMA). This response was dependent upon ligand expression on the target cells but not on expression of major histocompatibility complex (MHC) molecules, and the response could be blocked by anti-NKG2D antibodies. These T cells produced large amounts of T-helper 1 (Th1) cytokines and proinflammatory chemokines and killed ligand–expressing tumor cells. Adoptive transfer of chNKG2D-bearing T cells inhibited RMA/Rae-1β tumor growth in vivo. Moreover, mice that had remained tumor-free were resistant to subsequent challenge with the wild-type RMA tumor cells, suggesting the generation of immunity against other tumor antigens. Taken together, our findings indicate that modification of T cells with chimeric NKG2D receptors represents a promising approach for immunotherapy against cancer.
Introduction
T cells, especially cytotoxic T cells (CTLs), play important roles in antitumor immunity.1 Adoptive transfer of tumor-specific T cells into patients provides a promising means to treat cancer.2 However, the traditional approaches for obtaining large numbers of tumorspecific T cells are time consuming, laborious, and sometimes difficult because the average frequency of antigen-specific T cells in the periphery is extremely low.3-5 In addition, isolation and expansion of T cells that retain their antigen specificity and function can also be a challenging task.2 Genetic modification of primary T cells with tumor-specific immunoreceptors, such as full-length T-cell receptors (flTCRs) or chimeric TCR (chTCR) molecules provides a novel way for redirecting T cells against tumor cells.6-9 This strategy avoids the limitation of low frequency of antigen-specific T cells, allowing for facilitated expansion of tumor-specific T cells to therapeutic doses. Although some success has been reported using flTCR- or chTCR-transduced T cells, several factors, such as incorrect pairing between endogenous and exogenous TCR molecules, variable signaling capacity, and potential immunogenecity of chTCR molecules, may limit the therapeutic efficiency of these approaches.2,10,11 Therefore, investigation of novel immunoreceptors besides flTCR or chTCR molecules remains an important goal.
Natural killer (NK) cells attack tumor and virally infected cells in the absence of major histocompatibility complex (MHC) restriction, using a combination of signals from activating and inhibitory receptors.12 One of these activating receptors is NKG2D, which is expressed on all NK cells, NKT cells, γδ T cells, and some CD8+ αβ T cells.12,13 Ligands for mouse NKG2D are Retinoic acid early inducible protein 1 (Rae-1), Murine UL-16–binding proteinlike transcript (Mult-1), and minor histocompatibility antigen H60 (H60), and ligands for human NKG2D include MHC class I chain–related A (MICA), MICB, and several UL-16–binding proteins (ULBPs).13,14 It has been found that NKG2D ligands are primarily expressed on tumor cells but not on most normal tissues.13,14 Thus, the NKG2D receptor–NKG2D ligand system provides a relatively specific system for immune cells to recognize tumor cells. Recent data show that Rae-1– and H60-expressing tumor cells can induce robust antitumor effects in an NK cell–mediated and CD8+ T-cell–mediated fashion.15 However, NKG2D expression on T cells does not induce direct activation of T cells after NKG2D crosslinking, but NKG2D enhances T-cell signaling initiated by TCR crosslinking.16 This is probably due to the distinct signaling pathway of NKG2D in different cell types. T cells express the adaptor protein Dap10 but lack expression of Dap12, whereas NK cells express both adaptor proteins.16,17 Dap12 contains an immunoreceptor tyrosine-based activation motif (ITAM) capable of providing primary signals for cell activation.18 In contrast, Dap10 only contains a Tyr-X-X-Met (YXXM) motif that transduces costimulatory signals via phosphatidylinositol 3 (PI3) kinase.14
In an effort to develop a new mechanism for T cells to attack tumor cells and induce host antitumor immunity, we genetically modified primary T cells with chimeric NKG2D receptor containing the CD3ζ chain-signaling domain. Our hypothesis was that the chimeric NKG2D-modified T cells would react to NKG2D ligand–positive tumor cells and become fully activated, resulting in elimination of the tumor and induction of host antitumor immunity.
Materials and methods
Mice
C57BL/6 mice were purchased from the National Cancer Institute (Frederick, MD), and all animal work was conducted at the Dartmouth Medical School Animal Facility in accordance with institutional guidelines.
Cell lines
The cell lines Bosc23, PT67, GP+E86, EG7 (H-2b), and YAC-1 were obtained from the American Type Culture Collection (ATCC; Rockville, MD). RMA cells (H-2b) originated from a Rauscher virus–induced C57BL/6 T-cell lymphoma.19 RMA-S is an subline of RMA which lacks MHC class I surface expression.20 All packaging cells were grown in Dulbecco modified Eagle medium (DMEM) with a high glucose concentration (4.5 g/L) supplemented with 10% heat-inactivated fetal bovine serum (FBS; Hyclone, Logan, UT), 20 U/mL penicillin, 20 μg/mL streptomycin, 1 mM pyruvate, 10 mM HEPES (N-2-hydroxyethylpiperazine-N′-2-ethanesulfonic acid), 0.1 mM nonessential amino acids, and 50 μM 2-mercaptoethanol. RMA, EG7, RMA-S, and YAC-1 cells were cultured in RPMI plus the same supplements described.
Retroviral vector construction
The full-length murine NKG2D cDNA was purchased from Open Biosystems (Huntsville, AL). Murine CD3ζ chain, Dap10, and Dap12 cDNAs were cloned by reverse transcriptase–polymerase chain reaction (RT-PCR) using RNA from concanavalin A (ConA)– or interleukin (IL)–2 (1000 U/mL)–activated spleen cells as templates. Mouse NKG2D ligands Rae1β and H60 were cloned from YAC-1 cells by RT-PCR. All PCR reactions were performed using high-fidelity enzyme Pfu or PfuUltra (Stratagene, La Jolla, CA). The oligos are shown in Table 1. chNKG2D was created by fusing the murine CD3ζ chain cytoplasmic (CYP) region coding sequence (CD3ζ-CYP) to the full-length gene of murine NKG2D. Briefly, the SalI-EcoRI fragment of CD3ζCYP (with the initiation codon ATG at the 5′ end, primers no. 9 and 10) the EcoRI-XhoI fragment of NKG2D (without ATG, primers no. 2 and 3) were ligated into the SalI/XhoI-cut pFB-neo retroviral vector (Stratagene). Similarly, chDap10 was generated by fusing the SalI-EcoRI fragment of full-length Dap10 (primers no. 4 and 6) to the EcoRI-XhoI fragment of CD3ζCYP (primers no. 11 and 12). Wild-type NKG2D (primers no. 2 and 3), Dap10 (primers no. 4 and 5), and Dap12 (primers no. 7 and 8) fragments were inserted between the EcoRI and XhoI sites in pFB-neo. In some cases, a modified vector pFB-IRES-GFP was used to allow coexpression of green fluorescent protein (GFP) with genes of interest. pFB-IRES-GFP was constructed by replacing the 3.9–kilobase (kb) AvrII/ScaI fragment of pFB-neo with the 3.6 kb AvrII/ScaI fragment of a plasmid GFP-RV.21 Rae-1β (primers no. 13 and 14) and H60 (primers no. 15 and 16) cDNAs were cloned into pFB-neo.
Retrovirus production and transduction
Eighteen hours before transfection, Bosc23 cells were plated in 25-cm2 flasks at a density of 4 × 106 cells per flask in 6 mL of DMEM-10. Transfection of retroviral constructs into Bosc23 cells was performed using Lipofectamine 2000 (Invitrogen, Carlsbad, CA) according to the manufacturer's instruction. Viral supernatants were collected 48 and 72 hours after transfection and filtered (0.45 μm) before use. For generation of large-scale, high-titer ecotropic vectors, the ecotropic viruses produced above were used to transduce the dualtropic packaging cell PT67 in the presence of polybrene (8 μg/mL). After 3 rounds of transduction, PT67 cells were selected in G418 (1 mg/mL) for 7 days. Dualtropic vectors were then used to transduce the ecotropic cell line GP+E86. Through this process, the virus titer from pooled GP+E86 cells generally was over 1 × 106 colony-forming units (CFU)/mL. Concentration of retroviruses by polyethylene glycol (PEG) was performed according to a method described previously.11,22 Viral stocks with high titer (1-2 × 107 CFU/ml) were used for transduction of T cells. Primary T cells from spleens of C57BL/6 (B6) mice were infected 18 to 24 hours after ConA (1 μg/mL) stimulation based on our previous protocol.23 Two days after infection, transduced primary T cells (0.5-1 × 106/mL) were selected in RPMI-10 media containing G418 (0.5 mg/mL) plus 25 U/mL recombinant human (rHu) IL-2 for an additional 3 days. Viable cells were isolated using Histopaque-1083 (Sigma, St Louis, MO) and expanded for 2 days without G418 before functional analyses. NKG2D ligand–expressing RMA (RMA/Rae-1 and RMA/H60) or RMA-S (RMA-S/Rae-1) cells were established by retroviral transduction with dualtropic vectors from PT67.
Cytokine production by gene-modified T cells
Gene-modified primary T cells (105) were cocultured with an equal number of RMA, RMA/Rae-1β, RMA/H60, or YAC-1 cells in 96-well plates in complete media. After 24 hours, cell-free supernatants were collected. Interferon (IFN)–γ was assayed by enzyme-linked immunosorbent assay (ELISA) using Duoset ELISA kits (R&D Systems, Minneapolis, MN). In some cases, T cells were cultured with equal numbers of irradiated (100 Gy) tumor cells for 3 days. Detection of other cytokines in culture was performed using Bio-Plex kits (BioRad, Hercules, CA) based on the manufacturer's protocol. Analysis was performed by the Immune Monitoring Laboratory of the Norris Cotton Cancer Center (Lebanon, NH).
Flow cytometry
For fluorescence-activated cell-sorting (FACS) analysis of NKG2D ligand expression, tumor cells were stained with mouse NKG2D–immunoglobulin (Ig) fusion protein (R&D Systems) according to manufacturer's instruction. Cell-surface phenotyping of transduced primary T cells was determined by direct staining with allophycocyanin–anti-CD3ϵ (clone 145-2C11; Pharmingen, San Diego, CA), phycoerythrin (PE)–anti-NKG2D (clone 16-10A1; eBioscience, San Diego, CA) and fluoroscein isothiocyanate (FITC)–anti-CD4 (Clone RM4-5; Caltag, Burlingame, CA) monoclonal antibodies (mAbs). Cell fluorescence was monitored using a FACSCalibur cytometer (Becton Dickinson, San Jose, CA). Sorting of NKG2D ligand–expressing cells was performed on a FACStar cell sorter (Becton Dickinson).
Cytotoxicity assay
Three or 4 days after G418 selection (0.5 mg/mL), retroviral vector–transduced primary T cells were cultured in complete RPMI media containing 25 U/mL human IL-2 for an additional 2 to 3 days. Viable lymphocytes were recovered by centrifugation over Histopaque-1083 (Sigma) and used as effector cells. Lysis of target cells (RMA, RMA/Rae-1β, RMA/H60, EG7, RMA-S, RMA-S/Rae-1β, and YAC-1) was determined by a 4-hour chromium 51 (51Cr) release assay as previously described.23 To block NKG2D receptors, anti-NKG2D (clone: CX5, 20 μg/mL) was included in those assays. The percentage of specific lysis was calculated as follows: % specific lysis = (specific 51Cr release–spontaneous 51Cr release)/(maximal 51Cr release–spontaneous 51Cr release) × 100.
Treatment of mice with genetically modified T cells
For the determination of direct effects of chNKG2D-bearing T cells (106) on the growth of RMA or RMA/Rae-1β tumors, chNKG2D- or vector-transduced T cells were mixed with tumor cells (105) and then injected subcutaneously into the shaved right flank of recipient mice. Tumors were then measured using a caliper, and tumor areas were calculated. Animals were regarded as tumor free when no tumor was found 4 weeks after inoculation. For the rechallenge experiments, mice were inoculated with 104 RMA cells on the shaved left flank. In other experiments, transduced T cells were injected intravenously the day before subcutaneous inoculation of tumor cells. Mice were monitored for tumor size every 2 days and were killed when tumor burden became excessive.
Statistical analysis
Differences between groups were analyzed using the Student t test. P values less than .05 were considered significant.
Results
Construction of chimeric NKG2D receptors
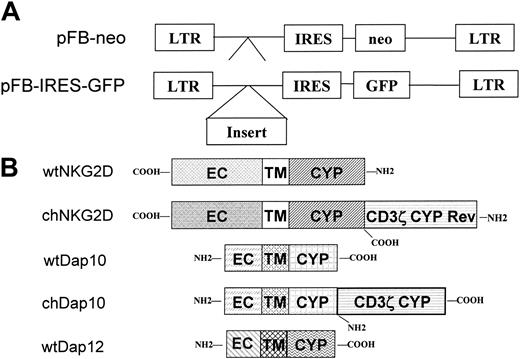
As a first step toward the generation of T cells with an ability to kill NKG2D-ligand–bearing tumor cells, cDNA sequences encoding the mouse NKG2D receptor and CD3ζ chain were assembled to make the chNKG2D receptor. NKG2D is a type II protein, in which the N-terminus is located intracellularly,14 whereas the CD3ζ chain is a type I protein with the C-terminus in the cytoplasm.24 In an effort to generate a chimeric NKG2D-CD3ζ fusion protein, an initiation codon ATG was placed ahead of the cDNA encoding the cytoplasmic region of the CD3ζ chain (without a stop codon TAA) followed by a wild-type NKG2D gene. Upon expression, the orientation of the CD3ζ portion is reversed inside the cells. The extracellular and transmembrane domains are derived from NKG2D. A second chimeric gene called chDap10, which encoded the Dap10 gene followed by a fragment coding for the CD3ζ cytoplasmic domain, was also constructed. The structures of the chimeric and wild-type receptors used are diagrammed in Figure 1.
Chimeric NKG2D is expressed at the cell surface in a Dap10- or Dap12-dependent manner
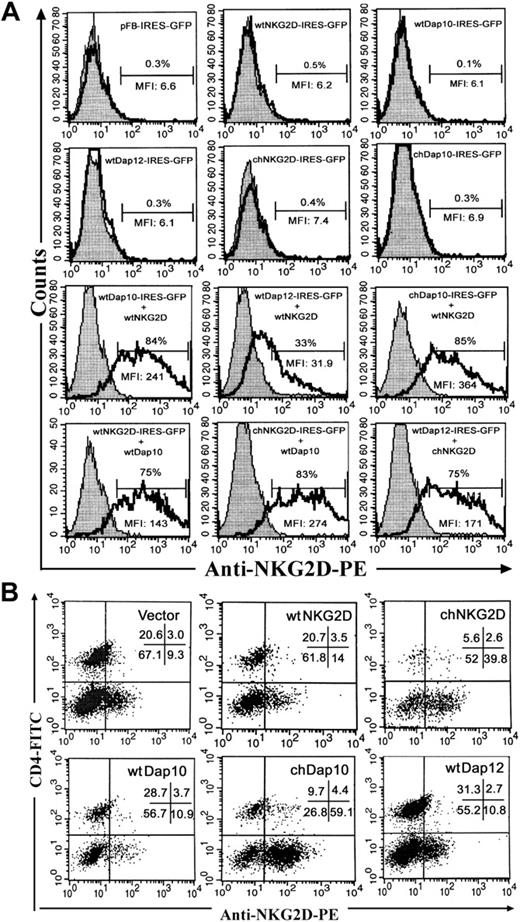
To determine whether chimeric NKG2D or chDap10 receptors could be expressed in a similar manner as wild-type NKG2D or Dap10, we cotransfected a NKG2D gene with an adaptor protein gene (Dap10/Dap12) into Bosc23 cells and determined NKG2D expression by flow cytometry. To analyze those cells that were transfected, a bicistronic vector with GFP gene controlled by internal ribosome entry site (IRES) was used. NKG2D surface expression was normalized by gating on the GFP+ cell population. Like many NK receptors, such as CD94/NKG2C, Ly49D, and Ly49H, NKG2D needs to be associated with adaptor proteins (ie, Dap10 and/or Dap12) for surface expression.14,25 Packaging cell Bosc23 did not express either NKG2D or Dap10/Dap12, and transfection with only 1 of the 2 components did not give rise to surface expression of NKG2D (Figure 2A). However, cotransfection of a NKG2D gene along with an adaptor protein gene led to significant membrane expression of NKG2D. Compared with Dap12, Dap10 transfection resulted in higher NKG2D surface expression. Surface expression of NKG2D after association with chDap10 adaptor was higher than that with wtDAP10. Higher surface expression of NKG2D was also observed after transfection with chNKG2D than with wild-type (wt) NKG2D genes, especially when pairing with the Dap12 gene (> 5-fold increase in mean fluorescence intensity [MFI]).
Structure of retroviral constructs. (A) The empty vectors pFB-neo and pFB-IRES-GFP were used in experiments as controls for retrovirus infection. The gene inserts were placed behind the 5′ long terminal repeat (LTR) and upstream of the internal ribosomal entry site (IRES), whereas the marker gene (either neo or GFP) was controlled by the IRES. Schematic diagram of wild-type (wt) and chimeric (ch) proteins are shown in panel B. The extracellular (EC), transmembrane (TM), and cytoplasmic regions (CYP) are indicated. In the chNKG2D, the CD3ζ chain was fused to the N-terminus of the NKG2D molecule in a reverse (Rev) orientation (COOH-terminus > NH2-terminus). In chDap10, the CD3ζ chain was placed downstream of the COOH-terminus of the Dap10 molecule in a normal orientation.
Structure of retroviral constructs. (A) The empty vectors pFB-neo and pFB-IRES-GFP were used in experiments as controls for retrovirus infection. The gene inserts were placed behind the 5′ long terminal repeat (LTR) and upstream of the internal ribosomal entry site (IRES), whereas the marker gene (either neo or GFP) was controlled by the IRES. Schematic diagram of wild-type (wt) and chimeric (ch) proteins are shown in panel B. The extracellular (EC), transmembrane (TM), and cytoplasmic regions (CYP) are indicated. In the chNKG2D, the CD3ζ chain was fused to the N-terminus of the NKG2D molecule in a reverse (Rev) orientation (COOH-terminus > NH2-terminus). In chDap10, the CD3ζ chain was placed downstream of the COOH-terminus of the Dap10 molecule in a normal orientation.
chNKG2D and chDap10 molecules express as efficiently as their wild-type counterparts on cell surface. (A) NKG2D expression on Bosc23 cells was evaluated 24 hours after transfection by combination of plasmids containing NKG2D and adaptor genes. Surface expression of NKG2D was determined on the gated GFP+ population using the PE-conjugated anti-NKG2D Ab (unshaded region). Isotype controls are shown in shaded region. The percentage of NKG2D+ cells is indicated. (B) NKG2D expression on B6 T cells 7 days after transduction. NKG2D expression was measured using anti-NKG2D mAbs in combination with anti-CD4 and anti-CD3 mAbs. More than 97% cells are CD3+ T cells (data not shown). CD4– T cells are CD8+ T cells. The dot plots shown were all gated on CD3+ cells. The percentage of cells in each quadrant is indicated. The data are a representative of 6 similar experiments.
chNKG2D and chDap10 molecules express as efficiently as their wild-type counterparts on cell surface. (A) NKG2D expression on Bosc23 cells was evaluated 24 hours after transfection by combination of plasmids containing NKG2D and adaptor genes. Surface expression of NKG2D was determined on the gated GFP+ population using the PE-conjugated anti-NKG2D Ab (unshaded region). Isotype controls are shown in shaded region. The percentage of NKG2D+ cells is indicated. (B) NKG2D expression on B6 T cells 7 days after transduction. NKG2D expression was measured using anti-NKG2D mAbs in combination with anti-CD4 and anti-CD3 mAbs. More than 97% cells are CD3+ T cells (data not shown). CD4– T cells are CD8+ T cells. The dot plots shown were all gated on CD3+ cells. The percentage of cells in each quadrant is indicated. The data are a representative of 6 similar experiments.
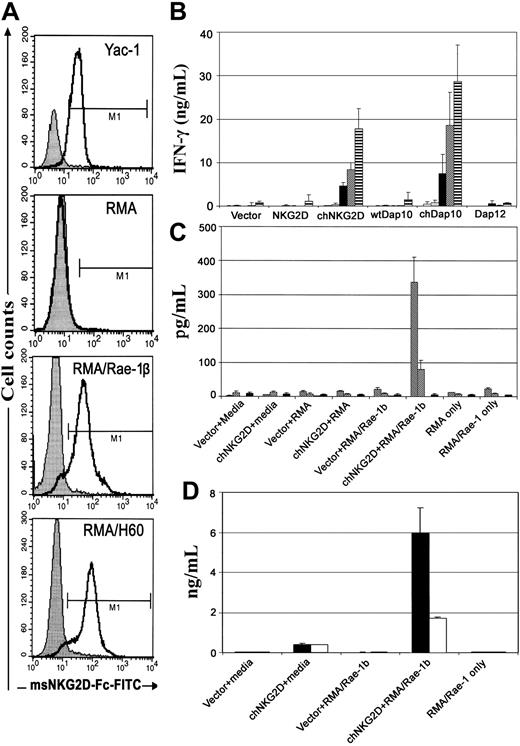
chNKG2D- or chDap10-modified T cells produce large amounts of Th1 cytokines and proinflammatory chemokines after coincubation with NKG2D ligand–expressing tumor cells. The NKG2D ligand expression on various target cells is shown in panel A. Cells were stained with mouse NKG2D Ig (open curve) or control Ig (shaded curve). Bar labeled M1 designates positive events. For detection of IFN-γ (B), T cells (105) were cocultured with 105 target tumor cells RMA (▦), RMA/Rae-1β (▪), RMA/H60 (▨), and YAC-1 (▤) or media alone (□) for 24 hours. Concentrations of IFN-γ in supernatants were determined by ELISA. For detection of other cytokines (C) and chemokines (D), irradiated (100 Gy) tumor cells instead were mixed with T cells for 3 days. Bio-plex assays were performed to measure the levels of GM-CSF (▧), IL-3 (▩), IL-5 (▦), IL-10 (▪) (shown in C), CCL3 (▪), and CCL5 (□) (D).
chNKG2D- or chDap10-modified T cells produce large amounts of Th1 cytokines and proinflammatory chemokines after coincubation with NKG2D ligand–expressing tumor cells. The NKG2D ligand expression on various target cells is shown in panel A. Cells were stained with mouse NKG2D Ig (open curve) or control Ig (shaded curve). Bar labeled M1 designates positive events. For detection of IFN-γ (B), T cells (105) were cocultured with 105 target tumor cells RMA (▦), RMA/Rae-1β (▪), RMA/H60 (▨), and YAC-1 (▤) or media alone (□) for 24 hours. Concentrations of IFN-γ in supernatants were determined by ELISA. For detection of other cytokines (C) and chemokines (D), irradiated (100 Gy) tumor cells instead were mixed with T cells for 3 days. Bio-plex assays were performed to measure the levels of GM-CSF (▧), IL-3 (▩), IL-5 (▦), IL-10 (▪) (shown in C), CCL3 (▪), and CCL5 (□) (D).
Concentrated high-titer retroviral vectors (ecotropic) were used to infect C57BL/6 spleen cells, and NKG2D surface expression was determined by flow cytometry 7 days after retroviral transduction. Genetic modification of T cells with wt Dap10, Dap12, and NKG2D did not significantly increase the surface expression of NKG2D (10%-20%) compared with vector alone (Figure 2B). In contrast, significantly higher NKG2D expression was observed in T cells modified with either chNKG2D (42%) or chDap10 (64%). In chDap10-transduced T cells, the surface-expressed NKG2D molecules are only due to endogenous molecules, whereas both endogenous and exogenous NKG2D molecules are likely to be responsible for surface expression in chNKG2D-modified T cells. Taken together, these data indicate that chNKG2D and chDap10 molecules are expressed in a similar manner as the wild-type molecules and that they increase NKG2D expression on T cells.
Chimeric NK receptor–expressing T cells produce proinflammatory cytokines upon culture with NKG2D-ligand–bearing tumor cells
To assess whether the chDAP10- or chNKG2D-transduced T cells were capable of recognizing NKG2D ligands, NKG2D ligand–positive tumor cells (RMA/Rae-1β, RMA/H60, and YAC-1) were used as targets for chNKG2D-bearing T cells (Figure 3A). chDAP10-or chNKG2D-transduced T cells produced huge amounts of IFN-γ (20-30 ng/mL) after coculture with RMA/Rae-1β, RMA/H60, or YAC-1 cells, but not with RMA cells (no ligands), indicating that these chNKG2D-modifed T cells could functionally recognize NKG2D-ligand–bearing tumor cells. In addition, upon NKG2D ligation, chDAP10- or chNKG2D-modified T cells also released significant amounts of proinflammatory chemokines (CC chemokine ligand 3 [CCL3] and CCL5) as well as Th1 cytokines, granulocyte-macrophage colony-stimulating factor (GM-CSF), and IL-3 (Figure 3B-C), but not Th2 cytokines IL-5 and IL-10 (Figure 3C). In contrast, wild-type Dap10, Dap12, or NKG2D modified T cells did not show any significant response to the stimulation by RMA/Rae-1β, RMA/H60, or YAC-1 cells. These data demonstrate that the chimeric molecules led to the direct activation of T cells.
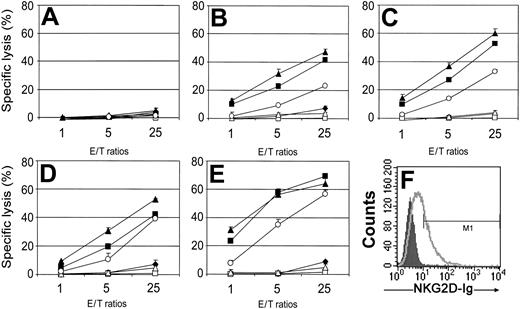
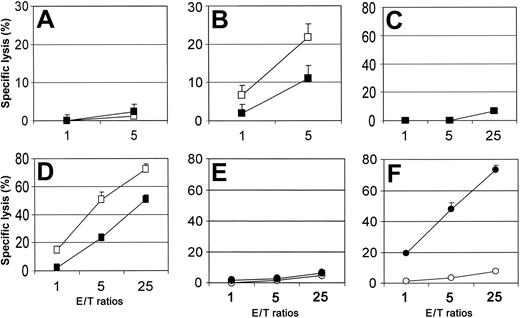
chNKG2D-bearing T cells kill target cells
The cytotoxic activity of chNKG2D-modified splenic T cells against tumor cells was also determined. As shown in Figure 4, chDap10- or chNKG2D-transduced T cells were able to lyse NKG2D ligand–expressing target cells (RMA/Rae-1β, RMA/H60, EG7, and YAC-1) in vitro (Figure 4B-E). The specificity of the interaction was apparent from the absence of lysis of YAC-1, EG7, RMA/Rae-1β, and RMA/H60 cells by vector-only transduced T cells, and the lack of lysis of RMA cells by chDap10- or chNKG2D-modified T cells (Figure 4A). Similar to cytokine production, no significant specific lysis of tumor cells was observed by wild-type Dap10– or wild-type NKG2D–modified T cells. T cells transduced with wild-type Dap12 were able to kill target cells that expressed ligands for NKG2D. This was expected because activated murine CD8+ T cells express NKG2D (associated with Dap10), so expression of Dap12 would allow the endogenous NKG2D to associate with Dap12 and provide a primary activation signal. It is noteworthy that T cells transduced with Dap12 were 3- to 5-fold less efficient than T cells transduced with chimeric NK receptors at killing tumor cells. The killing of YAC-1 and EG7 tumor cells demonstrates that the chimeric NK receptors provided the T cells a means to kill tumor cells that express endogenous NKG2D ligands (Figure 4F).
Specific lysis of target cells by gene-modified primary T cells. Effector T cells modified with vector only (♦), wtNKG2D (□), chNKG2D (▪), wtDAP10 (▵), chDap10 (▴), or wtDap12 (○) were cocultured with target cells RMA (A), RMA/Rae-1β (B), RMA/H60 (C), YAC-1 (D), or EG7 (E) cells, respectively, at ratios from 1:1 to 25:1 in 4-hour 51Cr release assays. The data are presented as means ± SD and are representative of 3 to 5 independent experiments. (F) The expression of NKG2D ligands on EG7 cells is shown. Cells were stained with mouse NKG2D Ig (open curve) or control Ig (shaded curve).
Specific lysis of target cells by gene-modified primary T cells. Effector T cells modified with vector only (♦), wtNKG2D (□), chNKG2D (▪), wtDAP10 (▵), chDap10 (▴), or wtDap12 (○) were cocultured with target cells RMA (A), RMA/Rae-1β (B), RMA/H60 (C), YAC-1 (D), or EG7 (E) cells, respectively, at ratios from 1:1 to 25:1 in 4-hour 51Cr release assays. The data are presented as means ± SD and are representative of 3 to 5 independent experiments. (F) The expression of NKG2D ligands on EG7 cells is shown. Cells were stained with mouse NKG2D Ig (open curve) or control Ig (shaded curve).
Killing by chNKG2D-transduced T cells is blocked by anti-NKG2D and is not dependent upon target cell expression of MHC molecules
Our data have demonstrated the need for NKG2D ligand expression on the target cells. To investigate the role of the NKG2D receptor, we tested whether blocking antibodies to NKG2D would diminish the cytotoxic activity. As shown in Figure 5, chNKG2D-transduced T cells kill RMA/Rae-1β (Figure 5B) and EG7 (Figure 5D) tumor cells, and this activity was reduced when anti-NKG2D antibodies were included in the assay. Vector-only–transduced T cells were unable to kill the target cells and the activity was not changed with the addition of anti-NKG2D antibodies (Figure 5A,C). Although these data support the idea that the NKG2D receptor is responsible for the activity in these assays, it is possible that the chimeric receptors in some way alter the T cells to kill via their T-cell–receptor. To address this, we chose to examine the ability of chNKG2D-transduced T cells to kill RMA-S/Rae-1β tumor cells. RMA-S cells are deficient in TAP genes and express very low levels of MHC class I molecules on cell surface and no MHC class II molecules.26 As shown in Figure 5E and F, chNKG2D-bearing T cells killed RMA-S/Rae-1β tumor cells but not RMA-S cells. Vector-transduced T cells did not kill either RMA-S cell line. Thus, these data support the idea that chNKG2D functions via direct NKG2D recognition of its ligand on target cells.
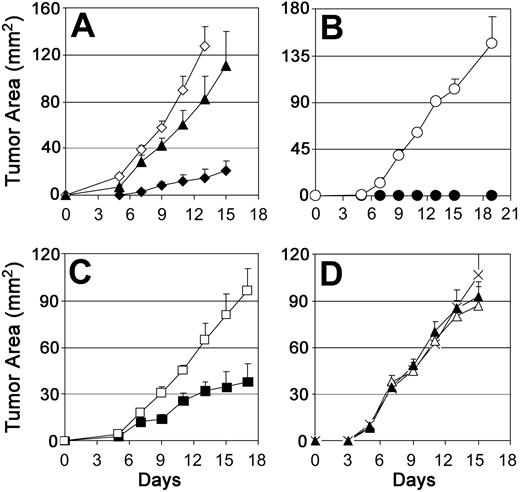
chNKG2D-transduced T cells suppress growth of NKG2D ligand–positive tumor cells in vivo
Having shown that chNKG2D-modified T cells could react against NKG2D ligand–positive tumor cells in vitro, we wanted to determine the therapeutic potential of chNKG2D-modified T lymphocytes in vivo. chNKG2D-bearing T cells (106) were coinjected with RMA/Rae-1β tumor cells (105) subcutaneously to C57BL/6 mice. T cells transduced with the chNKG2D construct significantly inhibited the growth of RMA/Rae-1 tumors (Figure 6A), whereas vector-only transduced T cells had no effect on tumor growth. Approximately 36% (4/11) of chNKG2D-bearing T-cell–treated mice were tumor free after 30 days. chNKG2D-bearing T cells did not show any significant inhibition effects on the growth of wild-type RMA cells (Figure 6D), suggesting that inhibition of RMA/Rae-1β tumor growth by chNKG2D T cells was mediated by chNKG2D–Rae-1β engagement. In a second and more stringent model, transduced T cells (107) were adoptively transferred intravenously into B6 mice 1 day before subcutaneous tumor inoculation in the right flank. These chNKG2D-bearing T cells significantly suppressed the growth of RMA/Rae-1β tumors (subcutaneous) compared with control vector–modified T cells (Figure 6C). As for the toxicity of treatment with chNKG2D-modified T cells, the animals treated with chNKG2D-bearing T cells did not show any overt evidence of inflammatory damage (ie, ruffled hair, hunchback, or diarrhea, etc), suggesting there was no overt toxicity (data not shown).
Lytic activity of chNKG2D-bearing T cells is dependent upon NKG2D recognition but not target cell MHC expression. Effector T cells modified with vector only (A,C) or chNKG2D (B,D) were cocultured with target cells RMA/Rae-1β (A-B) or EG7 (C-D) in the presence of anti-NKG2D antibodies (▪) or control antibodies (□), and percentage of specific lysis determined after a 4-hour 51Cr release assay. Effector T cells modified with vector only (○) or chNKG2D (•) were cocultured with RMA-S (E), or RMA-S/Rae-1β (F) cells, respectively, in 4-hour 51Cr release assays. The data are presented as means ± SD and are representative of 2 or 3 independent experiments.
Lytic activity of chNKG2D-bearing T cells is dependent upon NKG2D recognition but not target cell MHC expression. Effector T cells modified with vector only (A,C) or chNKG2D (B,D) were cocultured with target cells RMA/Rae-1β (A-B) or EG7 (C-D) in the presence of anti-NKG2D antibodies (▪) or control antibodies (□), and percentage of specific lysis determined after a 4-hour 51Cr release assay. Effector T cells modified with vector only (○) or chNKG2D (•) were cocultured with RMA-S (E), or RMA-S/Rae-1β (F) cells, respectively, in 4-hour 51Cr release assays. The data are presented as means ± SD and are representative of 2 or 3 independent experiments.
Effects of coadministration of chNKG2D-modified T cells with RMA/Rae-1β tumor cells on in vivo tumor growth and generation of host antitumor immunity. (A) chNKG2D (♦)– or vector-only (⋄)–transduced T cells were mixed with RMA/Rae-1β tumor cells at a ratio of 10:1 and injected subcutaneously into the right flank of recipient mice. RMA/Rae-1β cells alone (▴) were also injected as control. The error bars represent SEM. chNKG2D-bearing T cells significantly (P < .05 at days 5-15) suppressed the RMA/Rae-1β tumor growth compared with vector-transduced T cells or tumor alone. (B) Tumor-free mice (•) in the chNKG2D-treated group (A) and age-matched naive mice (○) were challenged with wild-type RMA cells (104) injected subcutaneously into the left flank. A summary of 3 independent experiments is shown. (C) The day before RMA/Rae-1β tumor implantation (day-1), 107 chNKG2D (▪)– or vector-only (□)–transduced T cells were adoptively transferred to mice intravenously. At day 0, tumor cells (105) were implanted subcutaneously at the right flank. The tumor areas are represented as means ± SEM. P < .05 at days 9 to 17. (D) chNKG2D (▴)– or vector-only(▵)–transduced T cells were mixed with wild-type RMA tumor cells at a ratio of 10:1 and injected subcutaneously into B6 mice. RMA cells alone (×) were also injected as control. The error bars represent SEM. There was no significant suppression of RMA tumor growth (P > .05) by chNKG2D-transduced T cells compared with vector-transduced T cells or tumor alone.
Effects of coadministration of chNKG2D-modified T cells with RMA/Rae-1β tumor cells on in vivo tumor growth and generation of host antitumor immunity. (A) chNKG2D (♦)– or vector-only (⋄)–transduced T cells were mixed with RMA/Rae-1β tumor cells at a ratio of 10:1 and injected subcutaneously into the right flank of recipient mice. RMA/Rae-1β cells alone (▴) were also injected as control. The error bars represent SEM. chNKG2D-bearing T cells significantly (P < .05 at days 5-15) suppressed the RMA/Rae-1β tumor growth compared with vector-transduced T cells or tumor alone. (B) Tumor-free mice (•) in the chNKG2D-treated group (A) and age-matched naive mice (○) were challenged with wild-type RMA cells (104) injected subcutaneously into the left flank. A summary of 3 independent experiments is shown. (C) The day before RMA/Rae-1β tumor implantation (day-1), 107 chNKG2D (▪)– or vector-only (□)–transduced T cells were adoptively transferred to mice intravenously. At day 0, tumor cells (105) were implanted subcutaneously at the right flank. The tumor areas are represented as means ± SEM. P < .05 at days 9 to 17. (D) chNKG2D (▴)– or vector-only(▵)–transduced T cells were mixed with wild-type RMA tumor cells at a ratio of 10:1 and injected subcutaneously into B6 mice. RMA cells alone (×) were also injected as control. The error bars represent SEM. There was no significant suppression of RMA tumor growth (P > .05) by chNKG2D-transduced T cells compared with vector-transduced T cells or tumor alone.
Therapy with chNKG2D-bearing T cells results in immunity to tumor cells that do not express ligands for NKG2D
Because the immune system can select for tumor variants, the most effective immunotherapies for cancer are likely going to be those that induce immunity against multiple tumor antigens. We tested whether treatment with chNKG2D-bearing T cells could induce host immunity against wild-type tumor cells. Mice that were treated with chNKG2D-bearing T cells and RMA/Rae-1β tumor cells and that were tumor free after 30 days (Figure 6A) were challenged with RMA tumor cells. These tumor-free mice were resistant to a subsequent challenge of wild-type RMA cells (104), whereas all control-naive mice had aggressive tumors (tumor area: ∼100 mm2) after 2 weeks (Figure 6B). This observation suggested that adoptive transfer of chNKG2D-bearing T cells allowed hosts to generate T-cell memory.
Discussion
In many cases, potent cytotoxic T lymphocytes are needed for effective tumor eradication.4 Genetic modification of T cells has become a promising way of “building better T cells” to attack tumors.2,4 This study demonstrates that T cells engineered with a chimeric NK cell receptor (incorporating CD3ζ chain signaling domain) can induce antitumor immunity and T-cell memory. Strategies using chimeric immune receptors (such as single-chain fragments of TCRs or antibody variable regions) have shown some success in various animal models.1,2,4,8-10 However, to bestow specificity against tumors, a specific chimeric gene must be constructed for each given antigen. Our strategy of using NK receptors avoids this requirement. chNKG2D-bearing T cells are capable of recognizing target cells as long as these cells express NKG2D ligands. In addition, chNKG2D is less likely immunogenic than single-chain antibody or single-chain TCR chimeras because the extracellular and transmembrane domains of chNKG2D are identical to wild-type NKG2D.
Interestingly, although the orientation of CD3ζ chain in chNKG2D is reversed, it still maintained functional capacity, suggesting that the interaction between the ITAMs of the CD3ζ chain and zeta-associated protein 70/spleen tyrosine kinase (Zap70/Syk) protein kinases may be orientation independent. In T cells, NKG2D associates with Dap10 and can signal via PI3 kinase to provide costimulation. The chimeric receptors presented in this paper have the potential to signal via CD3ζ (signal 1) and via Dap10–PI3 kinase (signal 2). It may be that these T cells were so active because the receptor can induce both signaling pathways. Future experiments will be undertaken to clarify this point. Furthermore, our data suggest that chNKG2D receptors allow for more efficient surface expression than wtNKG2D, especially when in association with Dap12 based on the mean fluorescent intensity of NKG2D expression on Bosc23 cells. This finding may be due to the increased stability of the fusion protein or its increased association capacity with adaptor proteins. Our result also showed that Dap10 was more efficient than Dap12 in allowing NKG2D surface expression. This observation was consistent with previous findings.27 Dap12 contains an ITAM, and transfer of wild-type Dap12 into primary T cells allowed the T cells to become activated to kill target cells that expressed ligands for NKG2D. However the Dap12-mediated lysis appeared less efficient than the chimeric receptor–bearing T cells. Inefficient pairing of NKG2D with Dap12 compared with Dap10 may be responsible for this less-efficient signaling. Although it may be possible to use Dap12 directly in an immunotherapy strategy, Dap12 is known to associate with other cell-surface receptors, so the ligand specificity of Dap12-bearing T cells in vivo would be complex. 28-30
T cells can use a variety of different effector mechanisms to inhibit tumor growth in vivo.4,31 Based on the in vitro cytotoxicity observed with chNKG2D-bearing T cells, it is very likely that the antitumor activity is achieved by the cytotoxic activity of the cells. However, other mechanisms are possible, including the release of cytokines and chemokines that activate and attract other immune cell populations, leading to reduction or delay of tumor growth.4,32,33 It may well be that attraction and activation of macrophages may be an important mechanism for chNKG2D-bearing T cells to eliminate tumor cells and promote antitumor immunity. It is well known that exocytosis of granules, such as perforin and granzymes, is a major pathway of T-cell–mediated cell killing.31 Fas ligand or tumor necrosis factor–related apoptosis-inducing ligand (TRAIL)–mediated pathways also play a role, especially in CD4+ T-cell–mediated killing.34,35 The exact pathway that chNKG2D-bearing T cells employed in the direct killing of target cells remains to be determined.
The critical roles of Th1 cytokines (eg, IFN-γ, GM-CSF) in antitumor immunity have also been well documented.32,36,37 These cytokines are considered important in activation of macrophages and for enhancement of antigen presentation.37 In addition to Th1 cytokines, local expression of high-levels of “inflammatory chemokines” such as CCL3 (macrophage inflammatory protein-1α [MIP-1α]) and CCL5 (RANTES [regulated on activation, normal T-expressed and secreted]) have been associated with tumor regression.38 Activated CD8+ T cells can secrete CCL3 and CCL5 with IFN-γ, and these cytokines function synergistically on macrophages, helping to drive a Th1 response.39 Our results showed that chNKG2D-modified T cells produced IFN-γ, GM-CSF, IL-3, CCL3, and CCL5 after coculture with NKG2D ligand–positive tumor cells. Thus, it is likely that the production of cytokines helped the host to generate antitumor immunity.
In addition to induction of direct antitumor immunity, adoptive immunotherapy with chNKG2D-bearing T cells may induce generation of T-cell memory. Since chNKG2D-bearing T cells did not show any significant cytotoxic effects on RMA cells during in vitro assays or primary in vivo RMA tumor challenge, it is unlikely that these chNKG2D-bearing T cells played a direct role in rejection of the RMA tumor cells upon subsequent challenge. Accordingly, generation of host T-cell memory due to the interplay between chNKG2D-bearing T cells and RMA/Rae-1β cells is presumably responsible for the subsequent wild-type RMA tumor rejection. However, we cannot rule out an expansion of RMA-specific subset of T cells within the transferred chNKG2D-bearing T cells that mediate rejection of wild-type RMA cells. Direct killing of RMA/Rae-1β tumor cells by chNKG2D-bearing T cells in situ is speculated to cause significant release of various tumor antigens. Concurrent production of large amounts of Th1 cytokines and chemokines by chNKG2D-bearing T cells locally may also provide a good milieu for recruitment of professional antigen presentation cells (APCs) and antigen presentation. Elicitation and expansion of polyclonal tumor-specific T-cell populations are expected to occur after encounter with tumor antigen-presented APCs leading to generation of antitumor T-cell memory.35 However, the exact role of chNKG2D-bearing T cells in generation of antitumor memory remains unclear.
On one level, our data complement data that demonstrate that treatment of mice with RMA/Rae-1 tumor cells led to no tumor growth and resistance to a challenge with RMA tumor cells.15 In our study, mice were given 105 RMA/Rae-1β cells and all mice developed tumors, but in another study mice did not develop tumors when they were given 106 RMA/Rae-1β tumor cells.15 One important difference between these studies was the level of Rae-1β expression on tumor cells, and in our study the RMA/Rae-1β cells expressed less Rae-1β than the cells used by Diefenbach et al.15 The host response depends on the level of Rae-1β expression, such that higher levels of expression lead to greater host immune responses. In fact, Diefenbach et al reported that RMA cells with reduced levels of Rae-1β expression resulted in tumor growth and death of wild-type mice.15 Our data demonstrate that chNKG2D-bearing T cells are effective against tumor cells with low levels of ligand expression and those that express endogenous NKG2D ligands.
Human NKG2D ligands (eg, MICA, MICB, and ULBPs) are not only expressed on tumor cells but also on some normal tissues, such as differentiated gut epithelium.14 Their expressions are induced by heat shock, oxidative stress, virus infection, and transformation.40 Although ULBP transcripts were detected in a wide range of tissues, the surface expression of ULBPs on normal tissues is low or has not been documented.14 In some cases, human tumor cells may evade NK cell surveillance by producing soluble forms of NKG2D ligands,41,42 although it is unknown if the levels of soluble ligands would alter the function of chNKG2D-bearing T cells. It has been shown that the susceptibility of target cells to NKG2D-mediated NK killing is correlated with NKG2D ligand density on the cell surface.43 Therefore, whether adoptively transferred chNKG2D-bearing T cells can attack normal tissues and result in autoimmune diseases may be dependent on the NKG2D ligand density on target cells. It is possible that chNKG2D-modified T cells will be able to target tumors bearing high levels of NKG2D ligands with reasonable specificity and correspondingly low toxicity. However, it may be considerate to engineer a “suicide gene” into the vector along with the chNKG2D gene, which will enable the elimination of transferred T cells to prevent potential autoimmunity or T cell transformation. Suitable “suicide gene” candidates include a thymidine kinase (TK) gene from human herpes virus (HSV) and a Fas-based “artificial suicide gene.”44,45 This suicidal strategy has been demonstrated to allow control of gene-modified T cells through the administration of gancyclovir and AP1903, respectively.
The studies presented here represent an important “proof-of-principle” for the eventual development of chimeric NK receptor-based antitumor therapies. However, to improve the overall therapeutic efficacy of chNKG2D-bearing T cells against tumors, many parameters, including the doses, times, and coadministration of cytokines, need to be optimized. Although in our model a single intravenous injection of 107 chNKG2D-bearing T cells in the absence of exogenous IL-2 has been shown to suppress tumor growth, multiple T-cell transfers may be helpful to achieve clinical efficacy. Administration of cytokines, such as IL-2, IL-7, or IL-15, may also enhance the therapeutic effects mediated by the infused chNKG2D-bearing T cells because these cytokines have been shown to promote survival of the adoptive transferred T cells and memory T cells.32,46
Many human cancers, such as colon cancer, leukemia, lymphoma, myeloma, cervical cancer, ovarian cancer, prostate cancer, and melanoma have been found to express NKG2D ligands.41,47,48 Thus, the strategy described here has a promising potential to treat many human cancers. The ability of chNKG2D-bearing T cells to induce long-term memory may be beneficial to cancer patients with minimal residual disease. Collectively, our findings suggest that genetic modification of T cells with a chimeric NKG2D receptor represents a promising alternative to current methods for the development of effective adoptive immunotherapy against cancer.
Prepublished online as Blood First Edition Paper, May 12, 2005; DOI 10.1182/blood-2004-11-4365.
Supported by National Institutes of Health grant CA101748.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
The authors thank Gary A. Ward (Englert Cell Analysis Laboratory, Norris Cotton Cancer Center) for cell sorting.