A subset of CD8 T cells in normal mice, expressing high levels of activation markers such as CD44, shares many properties with antigen-specific memory CD8 T cells. Homeostasis of CD44high CD8 T cells depends upon cytokines such as interleukin-15 (IL-15); however, the downstream signaling pathways regulating IL-15–dependent homeostatic proliferation are poorly defined. Surprisingly, we show here that haploinsufficiency of the protooncogene c-myc leads to a highly selective decrease in CD44high CD8 T cells in mice. Although steady-state proliferation and survival of CD44high CD8 T cells appeared not to be dependent on c-Myc, homeostatic proliferation of c-myc+/– CD44high CD8 T cells in lymphopenic hosts was strongly reduced, and the residual homeostatic proliferation of these cells appeared to occur independently of IL-15. Moreover, c-myc+/– CD44high CD8 T cells responded very poorly to purified IL-15 in vitro. Backcrossing of c-myc+/– mice to IL-15–/– mice revealed that the number of CD44high CD8 T cells decreased in an additive fashion in mice heterozygous for c-myc and IL-15. Finally homeostatic proliferation of antigen-specific memory CD44high CD8 T cells was also impaired in c-myc+/– mice. Collectively, our data identify c-Myc as a novel downstream component of the IL-15–dependent pathway controlling homeostatic proliferation of memory CD44high CD8 T cells.
Introduction
T-cell memory is essential for efficient protection against a variety of pathogens.1 In mice, antigen-specific memory T cells can be distinguished from naive T cells by their expression of high levels of several surface markers.2-4 For example, in the CD8 lineage, memory CD8 T cells are frequently identified by their elevated expression of CD44 and CD122. Memory CD8 T cells respond more rapidly and efficiently to re-encounter with pathogens. Enhanced responses of memory T cells involve many factors, including their increased frequency as well as their state of differentiation.
Normal unimmunized mice contain a subset of CD8 T cells that express the same activation markers as antigen-specific memory CD8 T cells. These so-called “memory-phenotype” or CD44high CD8 T cells increase with age5 and are widely believed to arise from repeated infections by environmental antigens, although this subject remains controversial.6 Regardless of their precise origin, CD44high CD8 T cells in normal mice have very similar requirements for their maintenance in vivo as antigen-specific memory CD8 T cells. In this regard, several lines of evidence implicate cytokines, particularly interleukin-15 (IL-15), as being very important for memory CD8 T cell homeostasis. First, IL-15 is a potent growth factor for CD44high CD8 T cells both in vitro and in vivo.7-9 Second, the number of CD44high CD8 T cells is significantly decreased and their homeostatic proliferation (measured upon adoptive transfer to lymphopenic recipients) is impaired in either IL-15–/– or IL-15R–/– mice.10-13 Third, CD44high CD8 T cells expand massively in IL-15 transgenic mice.14 Finally, injection of agents that induce type I interferon (IFN) (such as polyinosinicpolycytidylic acid [polyI:C]) selectively increase the number of CD44high CD8 T cells in vivo via an IL-15–dependent mechanism.7,8,15 In addition to IL-15, IL-7 has also been shown to play a role in the homeostasis of CD44high CD8 T cells, particularly in situations where IL-15 is limiting or absent.16-18 Despite this wealth of information, however, downstream signaling pathways and transcriptional mediators of cytokine-dependent homeostatic proliferation in CD44high CD8 T cells are not well defined.
c-myc is a proto-oncogene that regulates many cellular functions including proliferation, cellular growth, stem/progenitor as well as terminal differentiation, immortalization, and apoptosis.19-28 Although c-Myc function has been widely studied in cell lines such as fibroblasts, relatively little is known about the role of c-Myc in primary cells such as lymphocytes. This discrepancy is largely due to the fact that c-Myc is essential during development, such that disruption of the c-myc gene leads to early embryonic lethality at embryonic day (E) 10.5.29,30 Moreover, overexpression of c-Myc via transgenesis leads to rapid induction of tumors (particularly lymphomas),31-33 thereby complicating the analysis of lymphocyte function. Although conditional alleles of c-myc have recently been reported, inactivation of c-myc in hematopoietic cells rapidly leads to the disappearance of most myeloid and lymphoid lineages.34
To circumvent these problems, we have investigated T-cell development and function in mutant mice with a single functional c-myc allele (c-myc+/–). Although these mice show a decreased growth rate and reduced organ size,30 c-myc haploinsufficiency did not impact in any selective way on thymus development or on the frequency of major lymphocyte (T, B, or natural killer [NK]) subsets in peripheral organs. Surprisingly, however, c-myc+/– mice were selectively deficient in CD44high CD8 T cells. This deficiency corresponded to a reduced homeostatic proliferation of c-myc+/– CD44high CD8 T cells in lymphopenic hosts and a decreased capacity of these cells to respond to IL-15 in vivo and in vitro. Collectively, our data identify c-Myc as a novel downstream regulator of IL-15–dependent homeostatic proliferation of memory CD44high CD8 T cells.
Materials and methods
Mice
C57BL/6 and C57BL/6.PL (Thy1.1+) mice were purchased from Harlan (Horst, the Netherlands) and the Jackson Laboratory (Bar Harbor, ME) respectively. Mice heterozygous for the c-mycΔORF allele, in which the entire open-reading frame was deleted (c-myc+/–) have been previously described.30 c-myc+/– mice were backcrossed to C57BL/6 for 8 generations. For all in vivo experiments, mice backcrossed 5 times or more were used. In most experiments, these mice were used at older than 6 months of age because of the higher proportion of CD44high CD8 T cells present in aged versus young mice.5 Similar results were obtained, however, when using cells from younger mice (2-3 months). IL-15–/– mice (C57BL/6 background) were kindly provided by Immunex and for some experiments were bred in our facility to c-myc+/– mice. All mice were bred and housed under specific pathogen-free conditions. Animal studies were approved by the Cantonal Veterinary Office (Lausanne, Switzerland).
Antibodies and flow cytometry
FITC-conjugated monoclonal antibodies (mAbs) against CD62L (Mel-14), CD4 (GK1.5), CD8α (53.6.7), TCRαβ (H57), TCRγδ (GL3), CD3ϵ (17A2), B220 (RA3-6B2), Gr1 (Ly6G), and Alexa-647–conjugated mAbs against CD8α (53.6.7) and CD127 were purified and conjugated in our laboratory following standard protocols. CD90.2-PE and CD90.2-PE-Cy5, CD8α (53.6.7)–PE-Cy7, CD44-PE-Cy5, CD4-PE-Cy7, and CD4-APC-Cy7, CD25-PE-Cy7, CD90.1-biotin, streptavidin-PE-Cy7 and streptavidin-APC-Cy7 were purchased from eBiosciences (San Diego, CA). CD122 (IL-2Rβ)–PE, TCRγδ (GL3)–PE, CD161 (NK1.1)–PerCp-Cy5.5, annexin V–Cy5, CD19-APC-Cy7, CD132-biotin, as well as FITC-conjugated mAbs against BrdU (5′-bromo-2′-deoxyuridine) and B-cell lymphoma 2 (Bcl-2) were purchased from BD Biosciences (San Jose, CA). CD25-PE was purchased from Caltag (Burlingame, AL). Biotinylated IL-15Rα mAb was purchased from R&D Systems (Minneapolis, MN). Gp33-41-Db tetramers35 were produced in our institute. All stainings were performed in 2.4G2 supernatant to block unspecific binding to Fcγ receptors. Four-, 5-, or 6-color fluorescence-activated cell-sorting (FACS) analysis was performed using a FACSCalibur and a FACSCanto Flow Cytometer (Becton Dickinson, San Jose, CA) respectively, and data were analyzed using CellQuest or FACSDiva software (Becton Dickinson). Four-color FACS sorting was performed using a FACSAria Flow Cytometer (Becton Dickinson).
BrdU and Bcl-2 intracellular staining
BrdU uptake analysis was performed as described.36 Intracellular Bcl-2 staining was also performed according to the manufacturer's protocol using a Bcl-2 staining kit (BD Biosciences). FITC-conjugated isotype control mAb was used as control (BD Biosciences).
Cell-cycle analysis
Cell-cycle analysis was performed together with a 4-color surface staining. Briefly, after surface staining, fixation, and permeabilization, cells were stained with Hoechst 33342 (Molecular Probes, Eugene, OR) at 20 μg/mL for 5 minutes and analyzed on a LSR Flow Cytometer (Becton Dickinson).
Annexin V staining
A single-cell suspension of total splenocytes was incubated 1 hour at 37°C and cells were then surface stained. Annexin V staining was performed according to the manufacter's instructions (BD Biosciences), and samples were analyzed within the next hour by flow cytometry.
Adoptive transfer and CFSE staining
Anti-NK.1.1 antibody (PK136; 100 μg) was injected intraperitoneally into recipient hosts 48 hours before adoptive transfer and mice were exposed to a sublethal dose (600 Gy) of whole-body irradiation 24 hours before transfer. Prior to CFSE (5′ (and 6)-carboxy-fluorescein succinimidyl ester diacetate) staining of donor cell suspensions, cells were washed twice with cold phosphate-buffered saline (PBS) and were then incubated at 10 × 106 cells/mL in PBS with 2 μM CFSE (Molecular Probes) at 37°C for 10 minutes. Cells were then washed twice with cold Dulbecco modified Eagle medium (DMEM)/10% fetal calf serum (FCS). Donor CFSE–labeled splenocytes from distinct mice were mixed in a 1:1 ratio and 20 to 30 × 106 cells/mouse were injected intravenously. At the indicated times after adoptive transfer, lymph node (LN) and spleen cells were removed and stained with appropriate mAbs for flow cytometry analysis. For adoptive transfer of CD44low and CD44high CD8 T cells, a mixture of spleen cells from wild-type (wt) and c-myc+/– mice was sorted and CFSE labeled, and 2 × 106 cells per mouse transferred as described. Adoptive transfer of immune splenocytes was performed similarly 50 days after lymphocytic choriomeningitis virus (LCMV) infection (200 plaque-forming units (pfu)/mouse, strain LCMV-WE).
In vitro cell culture
In some experiments, total splenocytes were cultured in DMEM (supplemented with 10 mM HEPES, penicillin-steptomycin-neomycin [PSN], 50 μM 2-β-mercaptoethanol [Life Technologies, Bethesda, MD] and 10% FCS [Sigma, Buchs, Switzerland]) at a concentration of 3 × 106 cells/mL. CFSE-labeled cells were stimulated for 4 days with recombinant human IL-15 (R&D Systems) at the indicated concentrations. A fresh cytokine mix was added every day. For analysis of CD44low and CD44high CD8 T-cell proliferation in vitro, 200 000 sorted CD44low and CD44high CD8 T cells were CFSE labeled and cultured in 96-well plates at 1 × 106 cells/mL in the presence of IL-15 as described. For NK cell experiments, NK cell enrichment was performed by negative selection using Dynabeads (Dynal Biotech ASA, Oslo, Norway). CFSE-labeled NK cells were then cultured for 5 days in the presence of IL-15 at the indicated concentrations.
RNA extraction and real-time PCR
Total RNA from 200 000 sorted cells was prepared and reverse transcribed using standard procedures. Real-time polymerase chain reaction (PCR) was performed on a Light Cycler (Roche, Rotkreuz, Switzerland) according to the manufacter's instructions. The expression levels of c-myc were normalized by the expression of the housekeeping gene TATA-binding protein (TBP). Primers and conditions of the real-time PCR are available upon request.
Results
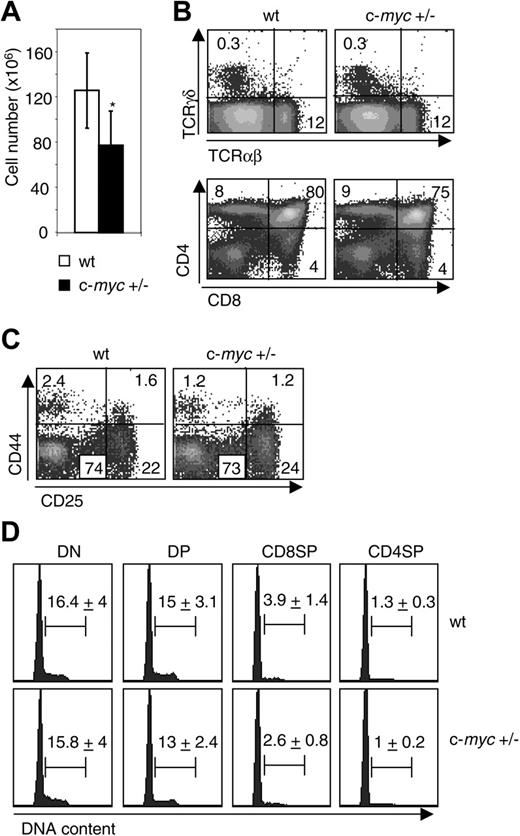
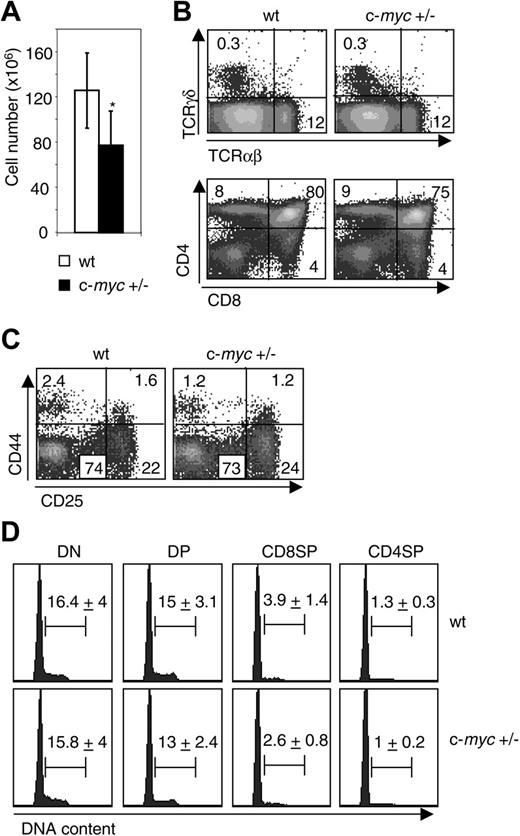
Reduced levels of c-Myc do not perturb thymocyte development
In order to understand the role of the c-Myc protein in the development of hematopoietic cells, we first analyzed the distribution of thymocyte populations in mice heterozygous for the c-mycΔORF allele, in which the entire open-reading frame was deleted (hereafter referred to as c-myc+/–), and wt controls. Although thymus cellularity is reduced in c-myc+/– mice compared with littermate controls (Figure 1A),30 similar proportions of the αβ and γδ T-cell lineages were observed (Figure 1B). The development of double-negative (DN) CD4–CD8– into double-positive (DP) CD4+CD8+, and single-positive CD4+CD8– (CD4SP) and CD4–CD8+ (CD8SP) cells was normal in c-myc+/– mice and cycling rates of these populations were not perturbed when c-Myc levels were reduced (Figure 1B,D). In addition, the percentages of CD24low CD4SP and CD8SP thymocytes, corresponding to the most mature populations that are ready to be exported from the thymus to the periphery,37 were not affected in c-myc+/– mice (data not shown). A more detailed analysis of DN subsets, according to the expression of CD44 and CD25 molecules as previously described,38 showed no differences in their development (Figure 1C). Taken together, these data revealed that reduced levels of c-Myc did not affect thymocyte development, differentiation, or maturation.
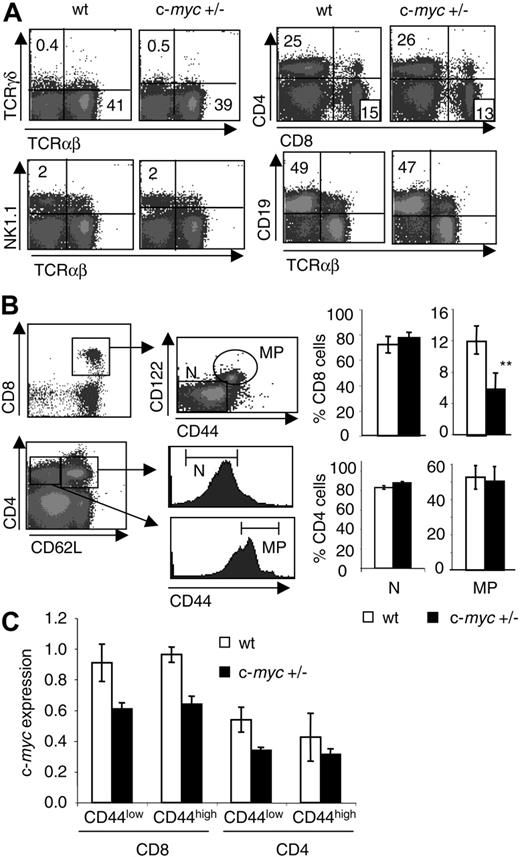
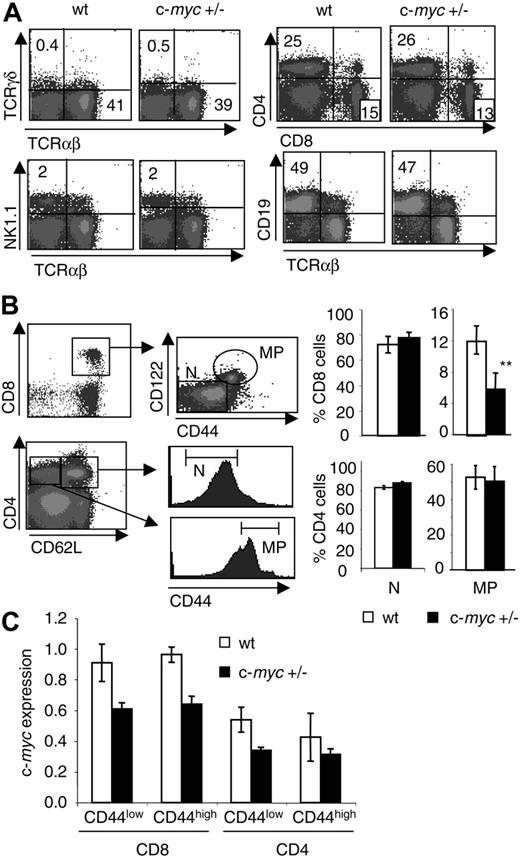
Selective decrease of CD44high CD8 T cells in the periphery of c-myc+/– mice
We further analyzed the distribution of the major lymphocyte populations in the periphery of c-myc+/– mice and observed that T cells (TCRαβ+ and TCRγδ+), mature CD4 and CD8 T-cell subsets (CD4+CD8– and CD4–CD8+), B cells (CD19+), and NK cells (NK1.1+TCRαβ–) were equally distributed in c-myc+/– mice and littermate controls in the spleen, LN, and peripheral blood lymphocytes (PBLs) (Figure 2A and data not shown). However, c-myc+/– mice had a selective decrease in the CD8 T-cell subset defined by high expression of the activation markers CD44 and CD122, the so-called “memory-phenotype” CD8 T-cell population (hereafter referred to as CD44high). Interestingly, other T-cell subsets such as naive (hereafter referred to as CD44low) CD8 T cells, as well as CD44low and CD44high CD4 T cells, were not affected by reduced levels of c-Myc (Figure 2B). This reduction in CD44high CD8 T cells varied between 2- to 3-fold and was observed in both young and adult c-myc+/– mice (data not shown). As expected, c-myc mRNA levels were reduced approximatively 1.4- to 1.6-fold in both CD8 and CD4 T cell subsets from c-myc+/– mice compared with wt controls; however, no significant differences were observed between CD44high and CD44low CD8 T cells in either case (Figure 2C), excluding a generalized cell-cycle defect of CD44high CD8 T cells due to lower expression of c-Myc.
Normal thymocyte development in c-myc+/– mice. (A) Thymus cellularity (mean ± SD; n = 5) is shown for wt and c-myc+/– mice. *P < .05. (B) Thymocytes from wt and c-myc+/– littermates were analyzed for expression of TCRαβ, TCRγδ, CD4, and CD8. The numbers shown represent the percentage of cells within each quadrant. (C) Subpopulations of DN thymocytes in wt and c-myc+/– littermates were analyzed for expression of CD44 and CD25 gated on lin– cells (defined as negative for markers expressed by mature cells such as TCRαβ, TCRγδ, CD3, CD4, CD8, B220, NK1.1, CD11b, and Gr1). (D) Cell-cycle analysis of DN, DP, CD8SP, and CD4SP thymocytes from wt and c-myc+/– littermates was performed by Hoechst staining and FACS analysis. The numbers shown represent the mean percentage ± SD of cells in S-G2-M phases. The results shown are representative of 2 experiments and 5 mice per group (4 months old) were analyzed in each experiment.
Normal thymocyte development in c-myc+/– mice. (A) Thymus cellularity (mean ± SD; n = 5) is shown for wt and c-myc+/– mice. *P < .05. (B) Thymocytes from wt and c-myc+/– littermates were analyzed for expression of TCRαβ, TCRγδ, CD4, and CD8. The numbers shown represent the percentage of cells within each quadrant. (C) Subpopulations of DN thymocytes in wt and c-myc+/– littermates were analyzed for expression of CD44 and CD25 gated on lin– cells (defined as negative for markers expressed by mature cells such as TCRαβ, TCRγδ, CD3, CD4, CD8, B220, NK1.1, CD11b, and Gr1). (D) Cell-cycle analysis of DN, DP, CD8SP, and CD4SP thymocytes from wt and c-myc+/– littermates was performed by Hoechst staining and FACS analysis. The numbers shown represent the mean percentage ± SD of cells in S-G2-M phases. The results shown are representative of 2 experiments and 5 mice per group (4 months old) were analyzed in each experiment.
Selective decrease in the proportion of CD44high CD8 T cells, but not other lymphoid populations, in c-myc+/– mice. (A) Splenocytes from wt and c-myc+/– littermates were analyzed for expression of TCRαβ, TCRγδ, CD19, NK1.1, CD4, and CD8. The numbers shown represent the percentage of cells within each quadrant. The results shown are representative of 3 experiments and 5 mice per group were analyzed in each experiment. (B) Naive (N) and memory-phenotype (MP) CD8 and CD4 T cells were defined by expression of CD8, CD62L, CD122, and CD44 (top panels) or CD4, CD62L, and CD44 (bottom panels). Bar graphs indicate the mean percentages ± SD of N and MP cells within CD8 or CD4 populations from wt and c-myc+/– littermates. The results shown are representative of more than 5 experiments. **P < .01. (C) c-myc mRNA levels were determined by real-time PCR in sorted naive CD44low and memory-phenotype CD44high CD8 and CD4 T cells from wt and c-myc+/– littermates. Values for c-myc were normalized to TBP values and presented in arbitrary units. Mean ± SD of triplicate samples is indicated.
Selective decrease in the proportion of CD44high CD8 T cells, but not other lymphoid populations, in c-myc+/– mice. (A) Splenocytes from wt and c-myc+/– littermates were analyzed for expression of TCRαβ, TCRγδ, CD19, NK1.1, CD4, and CD8. The numbers shown represent the percentage of cells within each quadrant. The results shown are representative of 3 experiments and 5 mice per group were analyzed in each experiment. (B) Naive (N) and memory-phenotype (MP) CD8 and CD4 T cells were defined by expression of CD8, CD62L, CD122, and CD44 (top panels) or CD4, CD62L, and CD44 (bottom panels). Bar graphs indicate the mean percentages ± SD of N and MP cells within CD8 or CD4 populations from wt and c-myc+/– littermates. The results shown are representative of more than 5 experiments. **P < .01. (C) c-myc mRNA levels were determined by real-time PCR in sorted naive CD44low and memory-phenotype CD44high CD8 and CD4 T cells from wt and c-myc+/– littermates. Values for c-myc were normalized to TBP values and presented in arbitrary units. Mean ± SD of triplicate samples is indicated.
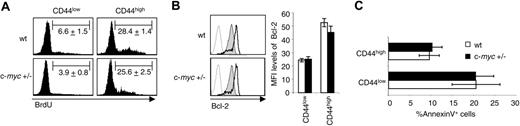
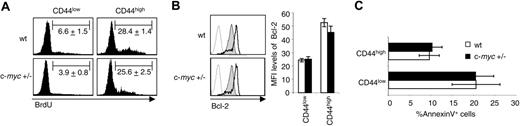
Steady-state proliferation and survival of CD44high CD8 T cells are not affected in c-myc+/– mice. (A) Wt and c-myc+/– littermates were injected intraperitoneally with BrdU, and BrdU was added in drinking water for 15 days. BrdU incorporation was measured for CD44low and CD44high CD8 T cells in the spleen. Numbers indicate the mean percentages ± SD of BrdU+ cells. The results shown are representative of 3 experiments. (B) Intracellular Bcl-2 expression in CD44low (filled histograms) and CD44high (empty histograms) CD8 T cells from wt and c-myc+/– littermates. Isotype control is shown in dotted lines. Bar graphs show the mean fluorescence intensity (MFI) ± SD of Bcl-2 expression in CD44low and CD44high CD8 T cells from wt (white) and c-myc+/– (black) mice. The results shown are representative of 3 experiments, and 3 to 5 mice per group were analyzed in each experiment. (C) After 1 hour of incubation at 37°C, the mean percentage ± SD of Annexin V+ CD44low and CD44high CD8 T cells from wt and c-myc+/– littermates was determined by flow cytometry.
Steady-state proliferation and survival of CD44high CD8 T cells are not affected in c-myc+/– mice. (A) Wt and c-myc+/– littermates were injected intraperitoneally with BrdU, and BrdU was added in drinking water for 15 days. BrdU incorporation was measured for CD44low and CD44high CD8 T cells in the spleen. Numbers indicate the mean percentages ± SD of BrdU+ cells. The results shown are representative of 3 experiments. (B) Intracellular Bcl-2 expression in CD44low (filled histograms) and CD44high (empty histograms) CD8 T cells from wt and c-myc+/– littermates. Isotype control is shown in dotted lines. Bar graphs show the mean fluorescence intensity (MFI) ± SD of Bcl-2 expression in CD44low and CD44high CD8 T cells from wt (white) and c-myc+/– (black) mice. The results shown are representative of 3 experiments, and 3 to 5 mice per group were analyzed in each experiment. (C) After 1 hour of incubation at 37°C, the mean percentage ± SD of Annexin V+ CD44low and CD44high CD8 T cells from wt and c-myc+/– littermates was determined by flow cytometry.
Steady-state proliferation and survival of CD44high CD8 T cells are not affected in c-myc+/– mice
CD44high CD8 T cells have increased steady-state proliferation and expression of survival factors (such as Bcl-2) compared with CD44low CD8 T cells (Figure 3A-B).39,40 Therefore, reduced numbers of CD44high CD8 T cells in c-myc+/– mice could be explained by a defect in steady-state proliferation or an increase in susceptibility to apoptosis of this population. Steady-state proliferation was determined by BrdU incorporation in CD44low and CD44high CD8 T cells and showed a similar turnover rate in c-myc+/– mice and controls (Figure 3A). Intracellular expression of the antiapoptotic Bcl-2 molecule in CD44low and CD44high CD8 T cells was not influenced by reduced expression of c-Myc (Figure 3B), suggesting that reduced levels of c-Myc do not interfere with survival of these cells. In addition, susceptibility to apoptosis measured by Annexin V staining after a 1-hour incubation at 37°C41,42 was similar for CD44low and CD44high CD8 T cells independently of c-Myc expression (Figure 3C). Survival of CD4 and CD8 T cells in vitro for 4 days without any growth factors also revealed no differences (data not shown). Taken together, these results indicate that reduced levels of c-Myc do not affect the number of CD44high CD8 T cells by impairing their steady-state turnover or their survival.
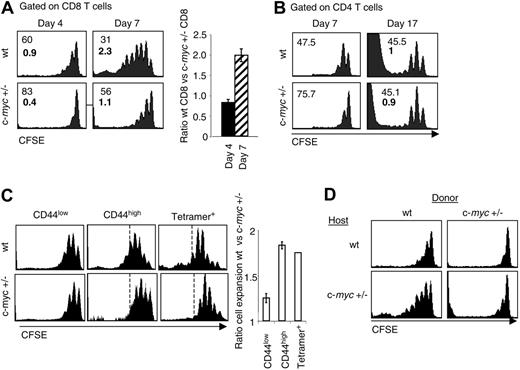
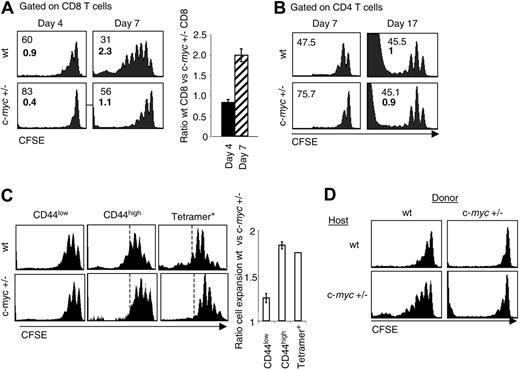
Impaired homeostatic proliferation of c-myc+/– CD8 T cells after adoptive transfer into sublethally irradiated recipients. Total splenocytes from wt (Thy1.1+) and c-myc+/– (Thy1.2+) littermates were CFSE labeled and adoptively cotransferred into sublethally irradiated wt (A-B) or c-myc+/– (D) recipients (Thy1.1+Thy1.2+). Spleen and LN cells were removed after 4, 7, and 17 days, pooled, and stained for CD4, CD8, Thy1.1, and Thy1.2. Histograms show representative CFSE profiles from donor CD8 (A,D) and CD4 (B) T-cell populations gated on the appropriate Thy1 marker. Upper numbers in histograms indicate the percentage of cells in the undivided peak; lower bold numbers indicate population doublings. Numbers were calculated according to Wells and colleagues.43 Bar graph represents the ratio of the percentage of wt versus c-myc+/– CD8 T cells. The results shown are representative of 2 experiments, and 1 to 3 mice per group were analyzed at each time point. (C) CD44low and CD44high CD8 T cells were sorted from wt (Thy1.2+) and c-myc+/– (Thy1.1+Thy1.2+) mice, CFSE labeled, and adoptively cotransferred into sublethally irradiated B6.PL (Thy1.1+) recipients. Splenocytes from wt and c-myc+/– littermates infected with LCMV 50 days before were CFSE labeled and adoptively transferred into sublethally irradiated wt recipients. Histograms show representative CFSE profiles from donor CD44low, CD44high, and tetramer+ CD8 T-cell populations gated on the appropriate Thy1 marker 6 or 7 days after transfer. Bar graph represents the ratio of the cell expansion of wt versus c-myc+/– cells.
Impaired homeostatic proliferation of c-myc+/– CD8 T cells after adoptive transfer into sublethally irradiated recipients. Total splenocytes from wt (Thy1.1+) and c-myc+/– (Thy1.2+) littermates were CFSE labeled and adoptively cotransferred into sublethally irradiated wt (A-B) or c-myc+/– (D) recipients (Thy1.1+Thy1.2+). Spleen and LN cells were removed after 4, 7, and 17 days, pooled, and stained for CD4, CD8, Thy1.1, and Thy1.2. Histograms show representative CFSE profiles from donor CD8 (A,D) and CD4 (B) T-cell populations gated on the appropriate Thy1 marker. Upper numbers in histograms indicate the percentage of cells in the undivided peak; lower bold numbers indicate population doublings. Numbers were calculated according to Wells and colleagues.43 Bar graph represents the ratio of the percentage of wt versus c-myc+/– CD8 T cells. The results shown are representative of 2 experiments, and 1 to 3 mice per group were analyzed at each time point. (C) CD44low and CD44high CD8 T cells were sorted from wt (Thy1.2+) and c-myc+/– (Thy1.1+Thy1.2+) mice, CFSE labeled, and adoptively cotransferred into sublethally irradiated B6.PL (Thy1.1+) recipients. Splenocytes from wt and c-myc+/– littermates infected with LCMV 50 days before were CFSE labeled and adoptively transferred into sublethally irradiated wt recipients. Histograms show representative CFSE profiles from donor CD44low, CD44high, and tetramer+ CD8 T-cell populations gated on the appropriate Thy1 marker 6 or 7 days after transfer. Bar graph represents the ratio of the cell expansion of wt versus c-myc+/– cells.
Impaired homeostatic proliferation of c-myc+/– CD44high CD8 T cells in vivo
Since homeostatic mechanisms control the size of lymphocyte pools and the number of T cells, we investigated whether c-Myc could affect homeostasis of CD8 T cells. To this end, we adoptively co-transferred CFSE-labeled splenocytes from wt and c-myc+/– mice into sublethally irradiated wt recipients. Interestingly, c-myc+/– CD8 T cells had a severe defect in homeostatic expansion in lymphopenic conditions, since 60% of these cells remained resting after 7 days, whereas only 30% of wt CD8 T cells failed to divide (Figure 4A). A quantitative estimation of cell division43 indicates that wt CD8 T cells expanded 2-fold more than c-myc+/– CD8 T cells (Figure 4A and Table 1). Similar results were obtained when wt and c-myc+/– spleen cells were transferred separately to lymphopenic recipients (data not shown), indicating that c-myc+/– CD8 T cells expanded less than wt CD8 T cells, even in the absence of competition. In contrast, reduced levels of c-Myc did not affect homeostatic expansion of CD4 T cells (Figure 4B and Table 1). Up-regulation of activation markers, such as CD44, upon homeostatic proliferation was similar on wt and c-myc+/– CD8 T cells (data not shown). Taken together, these data indicate that wt levels of c-Myc are required for optimal homeostatic proliferation of CD8 T cells, but not CD4 T cells, upon transfer into a lymphopenic host.
Since CD44high CD8 T cells are selectively deficient in c-myc+/– mice, we directly tested whether the impaired homeostatic proliferation of the total c-myc+/– CD8 population could be accounted for by the CD44high subset. To this end, CD44high and CD44low CD8 T cells from wt and c-myc+/– mice were purified by cell sorting and injected into sublethally irradiated wt recipients. As shown in Figure 4C, CD44high CD8 T cells from c-myc+/– mice proliferated less as compared to wt controls, and quantitative analysis revealed a 2-fold reduction in cell expansion. In contrast, CD44low CD8 T cells from wt or c-myc+/– mice proliferated to a similar extent. These data demonstrate a selective defect in homeostatic proliferation by CD44high CD8 T cells from c-myc+/– mice.
Impaired homeostatic proliferation of antigen-specific memory CD8 T cells from c-myc+/– mice
Although CD44high CD8 T cells from normal mice share many properties with bona fide antigen-specific memory CD8 T cells, the relationship between these 2 populations remains controversial.6 We therefore assessed the role of c-Myc in the well-characterized H-2Db-restricted CD8 T-cell response to the glycoprotein (gp) 33 to 41 epitope of LCMV using gp33-Db tetramers to monitor LCMV-specific CD8 T cells.35 Although the induction and maintenance of tetramer+ cells was not significantly affected in c-myc+/– mice (data not shown), homeostatic proliferation of LCMV-specific memory CD8 T cells in lymphopenic recipients was impaired to a similar extent as for CD44high CD8 T cells in normal mice (Figure 4C). Thus, bona fide antigen-specific memory CD8 T cells, like CD44high CD8 T cells in normal mice, depend upon c-Myc for optimal homeostatic proliferation.
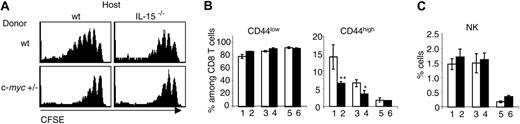
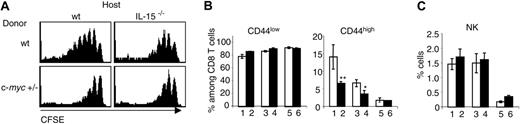
Reduced levels of c-Myc strongly impair IL-15 responsiveness of CD44high CD8 T cells in vivo. (A) Total splenocytes from wt (Thy1.1+) and c-myc+/– (Thy1.1+Thy1.2+) mice were CFSE labeled and adoptively cotransferred into sublethally irradiated IL-15–/– mice and wt controls (Thy1.2+). Histograms show CFSE profiles from donor wt and c-myc+/– CD8 T cells 7 days after adoptive transfer. (B-C) Bar graphs show the mean percentages ± SD of CD44low and CD44high CD8 T cells (B) and NK cells (C) in the spleen from the progeny of c-myc+/– IL-15+/– crossed with IL-15+/– mice. Bar 1 shows wt; bar 2, c-myc+/–; bar 3, IL-15+/–; bar 4, c-myc+/–IL-15+/–; bar 5, IL15–/–; and bar 6, c-myc+/–IL15–/–.*P < .05 group 3 versus 4; **P < .01 group 1 versus 2.
Reduced levels of c-Myc strongly impair IL-15 responsiveness of CD44high CD8 T cells in vivo. (A) Total splenocytes from wt (Thy1.1+) and c-myc+/– (Thy1.1+Thy1.2+) mice were CFSE labeled and adoptively cotransferred into sublethally irradiated IL-15–/– mice and wt controls (Thy1.2+). Histograms show CFSE profiles from donor wt and c-myc+/– CD8 T cells 7 days after adoptive transfer. (B-C) Bar graphs show the mean percentages ± SD of CD44low and CD44high CD8 T cells (B) and NK cells (C) in the spleen from the progeny of c-myc+/– IL-15+/– crossed with IL-15+/– mice. Bar 1 shows wt; bar 2, c-myc+/–; bar 3, IL-15+/–; bar 4, c-myc+/–IL-15+/–; bar 5, IL15–/–; and bar 6, c-myc+/–IL15–/–.*P < .05 group 3 versus 4; **P < .01 group 1 versus 2.
c-Myc levels influence IL-15–dependent homeostatic proliferation of CD8 T cells in lymphopenic recipients
Since IL-15 is essential for maintenance of CD44high CD8 T cells, we were interested to investigate whether reduced numbers of these cells in c-myc+/– mice was due to a defect in IL-15 responsiveness. To this end, we performed an adoptive transfer of wt and c-myc+/– splenocytes into sublethally irradiated IL-15–/– mice and controls. In the absence of IL-15, a residual homeostatic proliferation of wt and c-myc+/– CD8 T cells was observed, consistent with the possibility that IL-15–independent homeostatic proliferation may be driven by IL-7.16,17 Interestingly, homeostatic proliferation of c-myc+/– CD8 T cells was almost identical in IL-15–/– mice and controls, strongly suggesting that IL-15–induced, but not IL-15–independent, homeostatic proliferation of CD8 T cells requires normal levels of c-Myc expression (Figure 5A).
Intrinsic defect of c-myc+/– CD8 T cells undergoing homeostatic proliferation
Recent reports have described the importance of IL-15 trans-presentation in vivo and in vitro in the maintenance and proliferation of memory CD8 T cells.44-46 By performing an adoptive transfer of wt and c-myc+/– splenocytes into sublethally irradiated c-myc+/– recipients, we could exclude a possible defect in IL-15 presentation or production by c-myc+/– radiation-resistant cells. Thus, donor wt CD8 T cells underwent efficient homeostatic proliferation in c-myc+/– hosts (Figure 4D). Indeed, wt (and even c-myc+/–) CD8 T cells proliferated better in c-myc+/– hosts compared with wt recipients, presumably because of the reduced competition from c-myc+/– host CD8 T cells that survived the sublethal irradiation. Therefore, this result suggests strongly that impaired homeostatic proliferation of c-myc+/– CD8 T cells upon transfer into sublethally irradiated hosts (Figure 4A) is due to an intrinsic defect of CD8 T cells expressing reduced levels of c-Myc.
Effect of combined heterozygosity of c-Myc and IL-15 on CD44high CD8 T cells
c-myc+/– IL-15+/– mice were generated and crossed with IL-15+/– mice to analyze the effect of reducing both c-Myc and IL-15 levels in vivo on CD8 T cell subsets. We observed that the effect of heterozygosity of c-myc and IL-15 on the number of CD44high CD8 T cells was additive (compare groups number 2 and 4, Figure 5B). Interestingly, the residual population of CD44high CD8 T cells found in IL-15–/– mice was not further decreased when c-Myc levels were reduced (compare groups number 5 and 6, Figure 5B). CD44low CD8 T cells were not influenced by reduced levels of c-Myc in mice with limiting concentrations of IL-15. Bcl-2 expression in CD44high CD8 T cells, which is up-regulated by IL-15,47 was decreased in mice with reduced levels of IL-15; however, this effect was not amplified when c-Myc was reduced (data not shown). Taken together, these results suggest that IL-15 controls the number of CD44high CD8 T cells by acting on their survival via Bcl-2 regulation and on their proliferation by a mechanism implicating c-Myc.
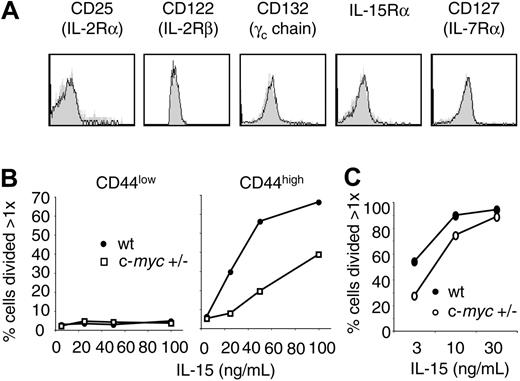
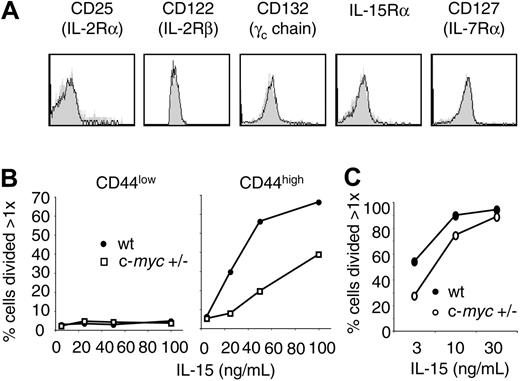
Impaired proliferation of c-myc+/– CD44high CD8 T cells to IL-15 in vitro
Efficient cytokine responsiveness relies on cytokine presentation and production, as well as on expression of the appropriate chains of the receptor inducing signaling events. Levels of expression of the IL-15Rα, β, and γ chains were similar on wt and c-myc+/– CD44high CD8 T cells (Figure 6A). As a consequence, it appears that c-Myc expression is required in CD44high CD8 T cells for efficient responsiveness to IL-15. To verify this hypothesis, CFSE-labeled sorted CD44low and CD44high CD8 T cells were cultured in vitro in the presence of purified IL-15. As expected, IL-15 responsiveness of c-myc+/– CD44high CD8 T cells was impaired in vitro (Figure 6B), while CD44low CD8 T cells did not respond to IL-15. Taken together, these results directly confirm a role for c-Myc in regulating IL-15–dependent proliferation of CD44high CD8 T cells.
Reduced IL-15–dependent proliferation of CD44high CD8 T cells and NK cells in vitro. (A) Histograms show expression of cytokine receptor chains on CD44high CD62Lhigh CD8 T cells from wt (empty histograms) and c-myc+/– mice (filled histograms). (B) Sorted CD44low and CD44high CD8 T cells from wt and c-myc+/– mice were CFSE labeled and cultured in the presence of various concentrations of IL-15 for 4 days. (C) NK-enriched splenocytes from wt and c-myc+/– mice were CFSE labeled and cultured in the presence of various concentrations of IL-15 for 5 days. Graphs in panels B and C show the percentage of cells that have undergone more than 1 division.
Reduced IL-15–dependent proliferation of CD44high CD8 T cells and NK cells in vitro. (A) Histograms show expression of cytokine receptor chains on CD44high CD62Lhigh CD8 T cells from wt (empty histograms) and c-myc+/– mice (filled histograms). (B) Sorted CD44low and CD44high CD8 T cells from wt and c-myc+/– mice were CFSE labeled and cultured in the presence of various concentrations of IL-15 for 4 days. (C) NK-enriched splenocytes from wt and c-myc+/– mice were CFSE labeled and cultured in the presence of various concentrations of IL-15 for 5 days. Graphs in panels B and C show the percentage of cells that have undergone more than 1 division.
Role of c-Myc in IL-15 responsiveness of NK cells
Since NK cells are also dependent on IL-15 for their development and maintenance,10,48 we were interested to investigate whether reduced levels of c-Myc also affect NK cell responsiveness to IL-15 in vitro and in vivo. c-myc+/– NK cells showed a slight defect in proliferation in response to IL-15 in vitro, although this defect could be restored at higher concentrations of IL-15 (Figure 6C). Interestingly, heterozygosity of IL-15 and/or c-Myc in vivo had no effect on NK cell numbers, although as reported previously IL-15–/– mice had very few NK cells (Figure 5C).10 Thus, it appears that NK cells are quantitatively less dependent on IL-15 and c-Myc than CD44high CD8 T cells both for proliferation in vitro and for homeostatic maintenance in vivo.
Discussion
Since proliferation, differentiation, and apoptosis play such crucial roles in lymphopoiesis, the aim of this study was to investigate lymphocyte development in c-myc+/– mice. To this end, we analyzed in detail the distribution of lymphocyte subsets in the thymus and periphery of these mice. While reduction of c-Myc by 2-fold did not affect the development and maturation of thymocytes, we found that c-Myc selectively regulates a subset of mature CD8 T cells. Hence, in c-myc+/– mice, a 2- to 3-fold reduction was observed in “memory-phenotype” CD44high CD8 T cells, whereas the CD44low CD8 T-cell compartment and other T-cell subsets were not affected.
Several independent lines of evidence support the hypothesis that c-Myc acts downstream of the IL-15 signaling pathway to promote proliferation of CD44high CD8 T cells. First, homeostatic proliferation of c-myc+/– CD44high CD8 T cells in sublethally irradiated hosts was impaired compared with wt controls. Since IL-15 is the key cytokine promoting homeostatic proliferation of CD8 memory T cells in normal mice,10-13 these data indicate that c-Myc may play a role in controlling IL-15–dependent homeostatic proliferation of the CD44high CD8 T-cell subset. This hypothesis was further confirmed by comparing the homeostatic proliferation of wt and c-myc+/– CD8 T cells in IL-15–/– mice. Whereas (as expected) wt CD8 T cells underwent significantly less homeostatic proliferation in the absence of IL-15, the residual homeostatic proliferation of c-myc+/– CD8 T cells was not further reduced in IL-15–deficient hosts. These data strongly suggest that c-Myc selectively controls IL-15–dependent homeostatic proliferation of CD44high CD8 T cells, whereas residual IL-15–independent homeostatic proliferation of those cells (presumably mediated by IL-7) is not affected by the reduced levels of c-Myc.
Backcrossing c-myc+/– IL-15+/– mice with IL-15+/– mice allowed us to further analyze the effect of c-Myc in vivo when concentrations of IL-15 are limiting. Interestingly, we found that the number of CD44high CD8 T cells is decreased in an additive fashion in mice heterozygous for both c-myc and IL-15. We also showed that in mice expressing reduced amounts of IL-15, the expression of the antiapoptotic molecule Bcl-2 in CD44high CD8 T cells is decreased. This is in accordance with other studies showing that increased survival of memory CD8 T cells correlates with an increased expression of Bcl-2 induced by IL-15.9,47 However, in c-myc+/– mice, reduced levels of c-Myc did not affect Bcl-2 expression in CD44high CD8 T cells, irrespective of the amount of IL-15. Thus it appears that survival of CD44high CD8 T cells is not directly affected by c-Myc. This would in turn support the hypothesis that c-Myc is a key regulator of IL-15 signaling for proliferation rather than survival.
We further tested the proliferation of purified c-myc+/– CD44high CD8 T cells in response to IL-15 in vitro and observed that it was strongly impaired compared with wt CD44high CD8 T cells. Even at the highest dose of IL-15 tested (100 ng/mL), proliferation of c-myc+/– CD44high CD8 T cells could not be fully restored. This result directly supports the hypothesis that IL-15 induces proliferation of CD44high CD8 T cells via c-Myc. In agreement with other studies performed in vitro, CD44low CD8 T cells did not proliferate in response to IL-15.9
IL-15 is also an important cytokine for NK cell development, activation, and proliferation, as well as homeostasis.10,49-51 If c-Myc is a universal regulator of IL-15 signaling, proliferation of NK cells from c-myc+/– mice to IL-15 should also be affected. We tested this hypothesis in vitro, and our results showed that NK cells from c-myc+/– mice have only a slightly decreased proliferation in response to IL-15. Furthermore, in contrast to c-myc+/– CD44high CD8 T cells, proliferation of c-myc+/– NK cells could be restored with high doses of IL-15. This result suggests that NK cells are less dependent upon IL-15 than CD44high CD8 T cells, in the sense that reduced levels of c-Myc are sufficient to drive IL-15–induced proliferation of NK cells, but not CD44high CD8 T cells, in vitro. This hypothesis was confirmed in vivo, since mice heterozygous for both c-myc and IL-15 had the same number of NK cells as wt mice, whereas numbers of CD44high CD8 T cells were dramatically reduced.
What is the mechanism by which c-Myc regulates IL-15–dependent proliferation of CD44high CD8 T cells? Recent studies indicate that IL-15 can be presented in trans (by macrophages or epithelial cells) to neighboring NK cells or memory CD8 T cells, thereby promoting their proliferation.44 However, wt levels of c-Myc are not required in macrophages or in other cells than T cells for efficient IL-15 presentation, since wt CD8 T cells can efficiently undergo homeostatic expansion when transferred into sublethally irradiated c-myc+/– recipients. Moreover, it is unlikely that c-myc+/– CD8 T cells would inefficiently bind IL-15 since the 3 chains composing the functional IL-15 receptor are expressed at the same levels in c-myc+/– CD44high CD8 T cells as in wt CD44high CD8 T cells.
Since production, presentation, and binding of IL-15 do not seem to be influenced by reduced levels of c-Myc, the role of c-Myc is likely to be downstream of engagement of the IL-15R. The binding of γc cytokine receptors activates the Janus kinase/signal transducer and activator of transcription (JAK/STAT) pathway, which is mainly regulated by suppressors of cytokine signaling (SOCS). Several lines of evidence have demonstrated that members of the SOCS family play crucial roles in γc cytokine signaling, and mice deficient in SOCS molecules have severe immunologic defects.52,53 Importantly, a recent study showed that SOCS-1 can regulate IL-15R signaling in CD44high CD8 T cells.54 In that study, SOCS-1–deficient mice were characterized by massive accumulation of CD44high CD8 T cells that showed increased proliferation in response to IL-15 in vitro and to polyI:C in vivo. Moreover, SOCS-1–deficient CD8 T cells could still up-regulate Bcl-2, suggesting that SOCS-1 regulates IL-15–induced proliferation but not IL-15–induced survival. In consequence, SOCS-1 would be an attractive candidate as a novel target of c-Myc, and in particular c-Myc could negatively regulate SOCS-1 upon IL-15 signaling. According to this scenario, reduced levels of c-Myc in CD44high CD8 T cells from c-myc+/– mice would not be sufficient to inhibit SOCS-1, which would lead to increased inhibition of IL-15 signaling and impaired proliferation in response to IL-15.
Since antigen-specific memory CD8 T cells differ from naive CD8 T cells in terms of their turnover rate, their capacity to proliferate homeostatically in the absence of antigen and their ability to rapidly produce cytolytic molecules, it is not surprising that the gene expression profile is very different in these 2 populations. In particular, many molecules involved in cell-cycle progression, such as cyclin-dependent kinase 4 (CDK4), CDK6, cyclin D2, and cyclin D3, are overexpressed in memory CD8 T cells compared with naive CD8 T cells, whereas cell-cycle inhibitors, such as p27Kip1 and p21Cip1, are expressed at lower levels.55-57 This gene expression profile in memory CD8 T cells would account for rapid division upon re-encounter with antigen, since memory cells would require a lower threshold of stimulation to enter cell cycle. In this context, it is interesting that many of the known target genes of c-Myc encode proteins involved in the cell cycle. Thus, expression of both CDK4 and CDK6 are positively induced by c-Myc, whereas expression of p27Kip1 and p21Cip1 are repressed.58-61 Hence, we can speculate that reduction of c-Myc in CD44high CD8 T cells could decrease CDK4 and CDK6 levels while increasing p27Kip1 and p21Cip1, thus impairing the capacity of these cells to homeostatically proliferate in response to IL-15. This hypothesis is particularly attractive since it would explain why reduced c-Myc levels would selectively affect cell-cycle progression in CD44high CD8 T cells as opposed to other lymphocyte subsets.
Prepublished online as Blood First Edition Paper, January 31, 2006; DOI 10.1182/blood-2005-09-3851.
Supported in part by Oncosuisse/Swiss Cancer League.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We are particularly grateful to Markus Nabholz, who participated in the early phase of this work. We are grateful to Immunex for providing IL-15–/– mice. We also thank Dr Frédéric Grosjean for FACS sorting, Dr Philippe Guillaume for the production of gp33-41-Db tetramers, and Dr Isabel Ferrero for help with real-time PCR.