Comment on Cesarman-Maus et al, page 4375
Anti–annexin A2 antibodies in patients with antiphospholipid syndrome accentuate endothelial cells and impair annexin A2–stimulated plasminogen activation.
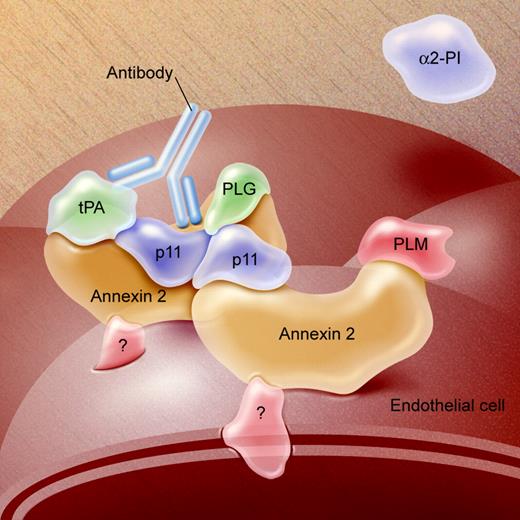
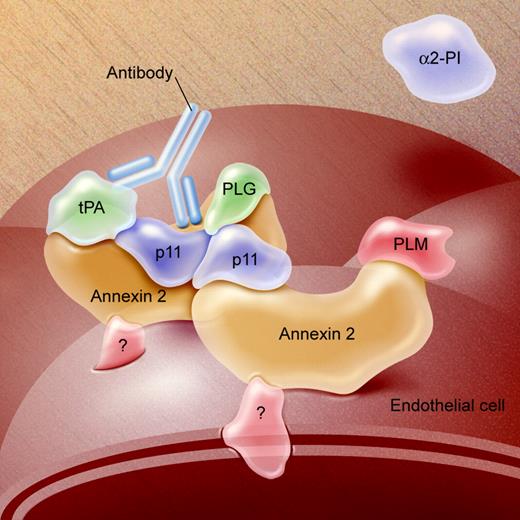
Autoantibody-mediated endothelial activation may play an important role in the pathogenesis of antiphospholipid antibody–associated thrombosis. In this issue of Blood, Cesarman-Maus and colleagues describe the presence of IgG or IgM anti–annexin A2 antibodies in 22.6% of patients with thrombosis due to antiphospholipid syndrome (APS), a prevalence significantly higher than that found in healthy controls, patients with systemic lupus but no history of thrombosis, and patients with thrombosis but no underlying autoimmune disease. Affinity-purified anti–annexin A2 antibodies activated endothelial cells, as determined by their ability to enhance tissue factor expression, and inhibited the ability of annexin A2 to promote tissue-type plasminogen activator (tPA)–mediated plasminogen activation, either in the fluid phase or on the endothelial surface (see figure). The latter effect suggests that although these antibodies recognized isolated annexin A2, they inhibited the activity of the annexin A2–S100A10 heterotetramer.1
These findings are important for several reasons. First, they are among the first to convincingly demonstrate the presence of antibodies that recognize a well-defined endothelial cell surface protein in patients with APS. Moreover, these antibodies induced functional effects that might contribute to a thrombophilic state. Second, in several patients, anti–annexin A2 antibodies occurred independently of lupus anticoagulants, anticardiolipin, or anti–β2-glycoprotein I (β2GPI) antibodies. Hence, screening for these antibodies in patients with a history, but not serologic studies, compatible with APS may be reasonable, though this consideration must be tempered by the retrospective nature of this study. Finally, these findings extend the recent work of Zhang and McCrae,2 in which anti-β2GPI antibodies were found to activate endothelial cells by cross-linking β2GPI bound to endothelial annexin A2, and support the hypothesis that annexin A2 cross-linking, either directly or indirectly, mediates endothelial activation.FIG1
Model of the annexin A2–S100A10 (p11) heterotetramer, depicting binding of tPA and plasminogen (p19) leading to generation of plasmin (PLM). The anti–annexin A2 antibody (Antibody) might inhibit binding of tPA or PLG or block their interaction with each other. Illustration by A. Y. Chen; adapted from Figure 2B of Cesarman-Maus and Hajjar.5
Model of the annexin A2–S100A10 (p11) heterotetramer, depicting binding of tPA and plasminogen (p19) leading to generation of plasmin (PLM). The anti–annexin A2 antibody (Antibody) might inhibit binding of tPA or PLG or block their interaction with each other. Illustration by A. Y. Chen; adapted from Figure 2B of Cesarman-Maus and Hajjar.5
This fascinating study raises several additional questions. First, whether anti–annexin A2 antibodies contribute to poor pregnancy outcomes remains uncertain, due to the inclusion of only small numbers of pregnant patients. Second, whether these antibodies affect other annexin A2–dependent processes, such as monocyte migration or angiogenesis, remains unknown.3 Third, the molecular relationship, if any, between these antibodies and those of other primary specificities involved in APS is uncertain. Finally, the mechanism by which cross-linking of endothelial cell annexin A2 induces cellular signaling responses remains enigmatic. Annexin A2 associates with cell surfaces through Ca2+ and phospholipiddependent interactions, but does not span the cell membrane, suggesting that interactions of annexin A2 with other cell surface proteins may contribute to the initiation of transmembrane signaling. Raschi et al4 have reported that a MyD88-dependent pathway culminating in NF-κB activation mediates endothelial activation caused by anti-β2GPI antibodies, implicating involvement of endothelial cell Toll-like receptors (TLRs), though the role for TLRs has not yet been demonstrated.
Based on these results, annexin A2 must now be considered alongside annexin V as a potentially key component in the pathogenesis of APS. Other receptor-based mechanisms involving apolipoprotein E receptor 2 may also mediate platelet adhesion to dimeric β2GPI. Additional studies addressing the importance of these mechanisms in animal models are eagerly awaited. ▪