Abstract
The deficiency of methylthioadenosine phosphorylase (MTAP) in T-cell acute lymphoblastic leukemia (T-ALL) and other cancers, while constitutively expressed in normal cells, allows for selective therapy using L-alanosine, an inhibitor of de novo AMP synthesis. We demonstrate that MTAP- T-ALL cells obtained at relapse are as sensitive to L-alanosine toxicity as diagnosis samples. The therapeutic index of L-alanosine can be increased by the use of a MTAP substrate, which protects MTAP+ normal cells. Since MTAP substrates MTA and 5′deoxyadenosine are prone to toxicities associated with adenosine, we synthesized and evaluated a potentially nontoxic MTAP substrate, 9-β-D-erythrofuranosyladenine (EFA). The cytotoxicity of EFA to hematopoietic progenitors erythroid burst-forming units (BFU-Es) and granulocyte-macrophage colony-forming units (CFU-GMs) was at least 26- to 41-fold less than that of MTA. In addition, EFA selectively rescued MTAP+ MOLT-4 cells from L-alanosine toxicity at 25 μM with negligible toxicity even at 100 μM. As for MTA, significant, albeit incomplete, rescue was achieved at 12.5 μM, but higher concentrations were toxic. EFA at 20 μM or less rescued primary MTAP+ T-ALL cells and normal lymphocytes from L-alanosine toxicity. Collectively, these data indicate that EFA is an effective agent for salvaging MTAP+ cells from L-alanosine toxicity and is superior to MTA due to lower cytotoxicity.
Introduction
Acute lymphoblastic leukemia (ALL) is the most common type of cancer in children. T-cell ALL (T-ALL) comprises 15% to 20% of ALL and frequently presents with high-risk features, requiring more intensive therapy than B-precursor ALL. Approximately 25% of T-ALL patients will relapse and die despite aggressive therapy. The development of selective therapies by exploitation of the molecular alterations in T-ALL cells but not in normal cells can improve the outlook for this disease as well as that of other malignancies possessing similar molecular characteristics. In this context, deficiency of a constitutively expressed enzyme, methylthioadenosine phosphorylase (MTAP), in T-ALL and other cancers offers an opportunity for selective anticancer therapy.
MTAP is an important salvage enzyme for both adenine and methionine. Specifically, 5′-deoxy-5′methylthioadenosine (MTA), generated during the synthesis of polyamines, is rapidly cleaved by the ubiquitous enzyme MTAP into adenine and 5-methylthioribose-1-phosphate (MTR-1-P).1 Adenine is efficiently salvaged to form AMP by adenine phosphoribosyltransferase, and MTR-1-P is converted to methionine by a complex set of oxidations via the intermediate 2-keto-4-methylthiobutyrate.2 The MTAP gene, located on chromosome 9p21, is often codeleted with CDKN2A and CDKN2B in tumor cells.3-9 Previously, we reported that the MTAP gene is deleted in over 30% of T-ALL patients at both diagnosis and relapse and is always associated with the deletion of CDKN2A.10 Lack of MTAP activity or inactivation of the MTAP gene has been demonstrated in other primary tumors including glioma,11 non-small-cell lung cancer,12,13 acute nonlymphoid leukemia,14,15 melanoma,14 and mesothelioma.16 MTAP-deficient malignant cells do not fall into any particular phenotypic category as established by us and others previously.14,15,17 The deficiency of MTAP in tumor cells offers a unique opportunity to develop a tumor-selective therapy, since MTAP activity is present in all normal cells including erythrocytes3,18 and bone marrow stem/progenitor cells19 within a relatively narrow range.14,15,17 Tumor cells devoid of MTAP activity are unable to salvage adenine from MTA and, therefore, are more dependent on the de novo synthesis of AMP. As a consequence, MTAP-deficient tumor cells are more sensitive than normal (MTAP+) cells to agents that block de novo AMP synthesis.20 Furthermore, normal cells abundant in MTAP can be rescued from the toxicity of inhibitors of de novo AMP synthesis by the provision of exogenous MTAP substrates that provide a source of adenine.
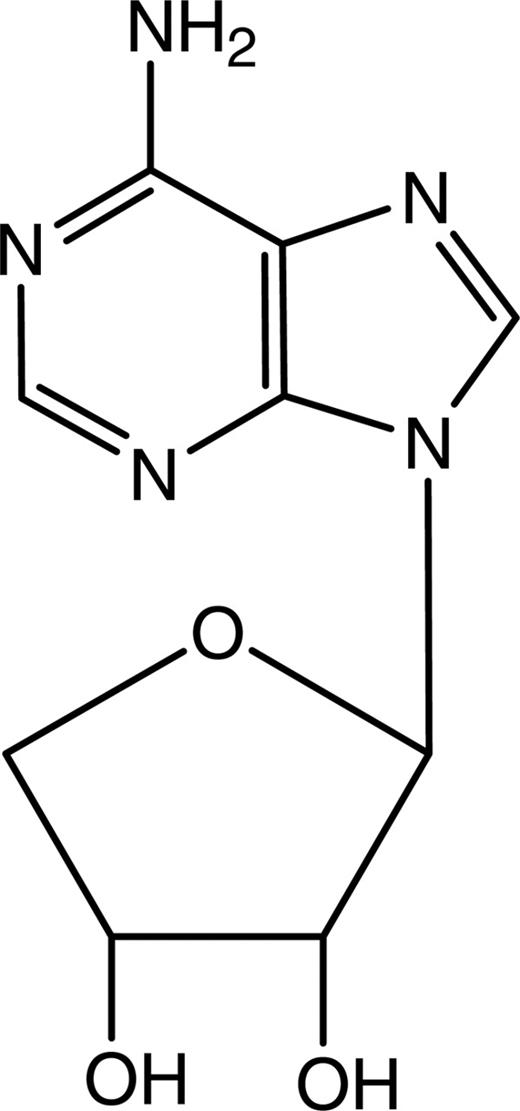
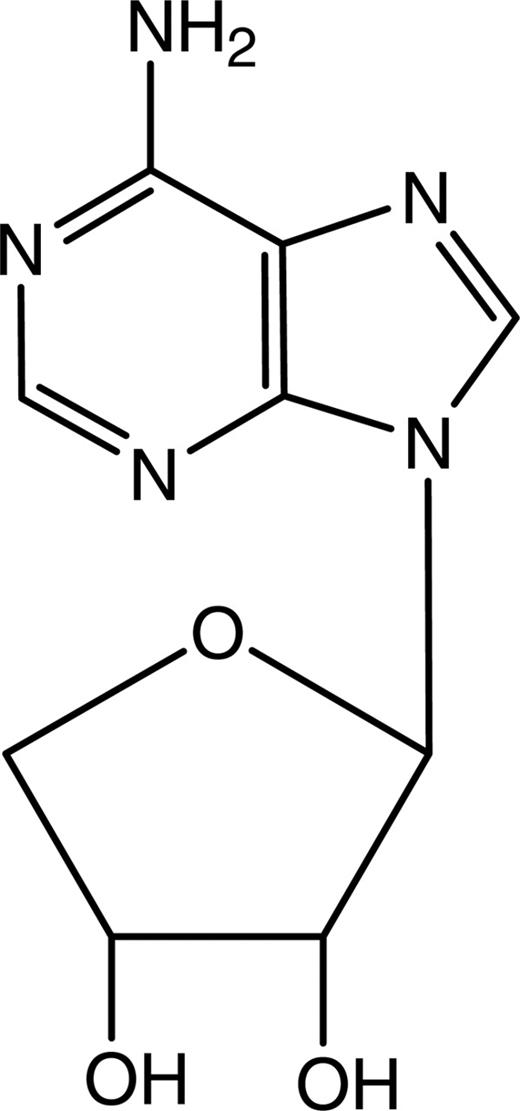
L-alanosine is a potent inhibitor of de novo AMP synthesis.21-24 The metabolite of L-alanosine, L-alanosinyl-5-amino-4-imidazole carboxylic acid ribonucleotide (L-alanosinyl-AICOR), is a strong inhibitor of adenylosuccinate synthase, which converts IMP to AMP. Thus, L-alanosine is an ideal candidate for MTAP-targeted therapy. In previous studies, we demonstrated that MTAP- T-ALL cells were more sensitive to the toxicity of L-alanosine than MTAP+ cells. In addition, we established that normal lymphocytes and MTAP+ primary T-ALL cells could be rescued from L-alanosine toxicity by MTA, the endogenous MTAP substrate,10 or by 5′-deoxyadenosine,20 whereas MTAP- primary T-ALL cells were not rescued. However, both MTA and 5′-deoxyadenosine have associated toxicities in normal cells in vitro as well as effects in vivo including coronary vasodilation.19,25-30 For this reason, the present study aims to synthesize and evaluate a potentially nontoxic MTAP substrate, 9-β-D-erythrofuranosyladenine (EFA),31 as a salvage agent for MTAP+ cells (Figure 1) to enhance the therapeutic index of L-alanosine.
Materials and methods
Preparation of EFA
EFA was synthesized in 4 main steps. These included the preparation of 1,2,3-tri-O-acetyl-D-erythrofuranose from D-erythrose followed by condensation with 2,6-dichloropurine to form 2,6-dichloro-9-(2,3-di-O-acetyl-β-D-erythrofuranosyl)-purine. 2-chloro-9-β-D-erythrofuranosyladenine was then prepared by treatment of 2,6-dichloro-9-(2,3-di-O-acetyl-β-D-erythrofuranosyl)-purine with ammonia in methanol. Finally, replacement of the 2-chloro group of 2-chloro-9-β-D-erythrofuranosyladenine with hydrogen yielded EFA. The 4 main steps in the synthesis of EFA are detailed here. 1,2,3-tri-O-acetyl-D-erythrofuranose was prepared from D-erythrose purchased from Lancaster Synthesis (Windham, NH). D-erythrose (3.0 g, 25 mmol) was dissolved with warming in dry pyridine (20 mL). Acetic anhydride (10 mL) was added drop wise to the stirred solution, keeping the temperature below 20°C. The light amber solution was stirred at room temperature overnight and then poured into 150 mL of ice/water with stirring and extracted with dichloromethane (3 × 100 mL). The combined extract was washed with diluted sulfuric acid (1 N, 1 × 100 mL) then saturated aqueous sodium bicarbonate (1 × 100 mL) and dried over magnesium sulfate and evaporated to yield a pale amber syrup (yield 5.1 g; 83%). This material is of suitable purity (thin-layer chromatography [TLC]) for the glycosylation reaction.
2,6-dichloro-9-(2,3-di-O-acetyl-β-D-erythrofuranosyl)-purine was prepared as follows: 2,6-dichloropurine (3.9 g, 21 mmol; Aldrich Chemical, Milwaukee, WI) was trimethylsilylated using hexamethyldisilazane (HMDS; 25 mL) and refluxing for 90 minutes. The excess HMDS was removed in vacuo and the erythrose triacetate (5.1 g, 21 mmol) dissolved in dry acetonitrile (100 mL) was added to the residue. When everything dissolved, the acid catalyst trimethylsilyl trifluoromethane sulfonate (5.6 mL, 1.5 equivalents [equiv]) was added in one lot. The reaction mixture was stirred overnight at room temperature and evaporated in vacuo. The residue was dissolved in ethyl acetate (300 mL), washed with saturated aqueous sodium bicarbonate (1 × 200 mL), dried over magnesium sulfate, and then evaporated to yield a yellow paste. This crude product was purified by flash silica gel chromatography using dichloromethane-acetone 9:1 (vol/vol). The pale yellow syrupy product slowly solidified to provide 1.22 g of pure product.
2-chloro-9-β-D-erythrofuranosyladenine was prepared by dissolving 0.88 g (2.35 mmol) of the dichloro nucleoside in dry methanol (10 mL) and cooling to 0°C. This was followed by bubbling ammonia gas into the solution for 15 minutes to saturate. The mixture was sealed in a small steel reaction vessel and heated at 80°C for 3 hours and allowed to remain at room temperature overnight. The vessel was cooled in ice, opened, and the methanolic ammonia was evaporated. The residue was flash chromatographed to remove some dichloro deblocked product using dichloromethane-methanol 9:1 (vol/vol) to yield 108 mg of pure title compound (melting point [mp] > 165°C decomposition [dec]).
Replacement of the 2-chloro group was accomplished as follows. Ninety milligrams (0.33 mmol) of the chloro nucleoside was dissolved in 50% aqueous ethanol (10 mL) with warming, and palladium on carbon (25 mg, 10%) was added. Potassium carbonate (45 mg) was added and the mixture was shaken in a hydrogenator at 20 psi hydrogen atmosphere. After 4 hours, TLC indicated the reaction was only about 25% complete. Therefore, additional palladium was added (10 mg) and the reaction continued at room temperature overnight, after which TLC showed the reaction to be complete. The mixture was filtered through celite and absorbed onto silica and flash chromatographed on silica gel using dichloromethane-methanol 85:15 (vol/vol) to provide 45 mg of EFA (Figure 1) as a white solid (mp > 220°C dec). The UV and NMR data are listed here: UV pH 1: λmax 258 nm, ϵ 13 400; pH 7, 11: λmax 260 nm, ϵ 16 000. Nuclear magnetic resonance (NMR; 500 MHz, DMSO-d6) δ 8.33 and 8.13 (2s, 2H, C-2, and C-8), 7.25 (s, 2H, NH2), 5.83 (d, 1H, J = 7.0 Hz, C-1′), 5.42 and 5.17 (2d, 2H, J = 6.5 Hz, 2′ and 3′ OH), 4.83 (m, 1H, C-2′), 4.32 (m, 1H, C-3′), 4.24 (m, 1H, C-4′), 3.77 (dd, 1H, C-4′).
EFA stability
EFA (lot 1I-108) was dissolved in PBS at 0.1 mg/mL and stored at room temperature. This solution was monitored by high-performance liquid chromatography (HPLC) using a reversed-phase column and gradient elution and with UV detection at 260 nm. Samples were analyzed at time 0, 24 hours, and 48 hours.
Cell lines
The T-ALL-derived cell lines MOLT-4 and CEM were obtained from ATCC (Rockville, MD) and were maintained in RPMI 1640 medium (Biowhittaker, Walkersville, MD) supplemented with 2 mM L-glutamine (Sigma, St Louis, MO) and BD ITS+ Premix (BD Biosciences, San Jose, CA) containing insulin, transferrin, selenous acid, bovine serum albumin, and linoleic acid (complete serum-free media).
Patient population and isolation of T-ALL cells
Heparinized bone marrow or peripheral blood samples were obtained at diagnosis or relapse from T-ALL patients enrolled in Pediatric Oncology Group Protocols no. 9000 and no. 9400 (ALL Biology Study). Approval was obtained from the University of California in San Diego institutional review board for these studies. Informed consent was provided according to the Declaration of Helsinki. To safeguard patient confidentiality, each patient was assigned a code number. Mononuclear cells from bone marrow or peripheral blood were isolated by isopycnic sedimentation through Ficoll-Hypaque (specific gravity 1.077 g/mL; Pharmacia, Piscataway, NJ) at 400g for 30 minutes followed by 2 washes with RPMI 1640. The content of lymphoblasts in these patient samples, as determined by Wright stain, was 80% or higher.
XTT assay
CEM and MOLT-4 human T-ALL cell lines were plated in complete serum-free medium at 0.4 × 105 cells/well in a final volume of 0.2 mL in flat-bottom microtiter well plates. L-alanosine (a generous gift from the Drug Synthesis and Chemistry Branch/Developmental Therapeutics Program/Division of Cancer Treatment, National Cancer Institute, Bethesda, MD) was added to cultures at 40 μM, and EFA and MTA (Sigma) were added simultaneously at increasing concentrations. Cells were cultured for 72 hours and viable cells were quantified using an XTT colorimetric assay kit (Sigma) according to the manufacturer's recommendations.
3H-thymidine incorporation assay
Primary T-ALL cells and peripheral blood mononuclear cells (PBMCs) from healthy donors were plated at 0.1 × 106 cells/well into 96-well plates (0.2 mL/well) in RPMI supplemented with 10% fetal bovine serum, 2 mM glutamine, and 1% penicillin/streptomycin (complete medium). Phytohemagglutinin (PHA) was added to PBM cultures at 5 μg/mL to stimulate proliferation. L-alanosine was then added to wells at concentrations of 20 or 40 μM along with increasing concentrations of EFA. Cells were cultured for 3 days and then pulsed with 3H-thymidine for 6 hours.
Colony-formation assay
Cultures of hematopoietic progenitor cells were prepared as described previously.32 Briefly, 2 × 105 mononuclear cells from healthy bone marrow donors were plated in 35-mm Petri dishes at 37°C in Iscove modified Dulbecco medium containing 1% methylcellulose, 30% dialyzed horse serum, 2 units of erythropoietin, 15 ng IL-3 (Amgen, Thousand Oaks, CA), 50 units GM-CSF (Genetics Institute, Cambridge, MA), 0.1 μM α-thioglycerol, 1% BSA, 50 IU/mL penicillin, and 50 mg/mL streptomycin. The cultures were treated with increasing concentrations of EFA or MTA for 14 days. An erythroid burst-forming unit (BFU-E) was identified as a large aggregate of more than 64 hemoglobinized cells or as clusters of 3 or more subcolonies consisting of 8 or more hemoglobinized cells per subcolony. The granulocyte-monocyte colony-forming unit (CFU-GM) was enumerated as a group of more than 50 granulocytic/monocytic translucent cells.
Western blot analysis
Protein was extracted from primary leukemia cells and PBMCs (10 × 106 to 20 × 106) with 30 μL of SDS lysis buffer (50 mM Tris-HCl, pH 6.8; 2% SDS; 0.1% bromophenol blue; 10% glycerol; 5 mM DTT). Samples were heated in boiling water for 10 minutes and then the lysate was passed through a 28-gauge needle to shear chromosomal DNA. Supernatants were then collected after spinning in a microfuge at 16 000 g for 10 minutes at 4°C. Proteins were resolved on a 10% SDS-polyacrylamide gel (NuPAGE; Invitrogen, San Diego, CA) run at 200 V for 45 minutes. Proteins were transferred to an Immobilin-P membrane (Millipore, Bedford, MA). Membranes were blocked with 5% nonfat milk in TBST (20 mM Tris-HCl, pH 7.5; 137 mM NaCl; 0.05% Tween 20) and then probed with a MTAP antibody (a generous gift from Dr Dennis Carson) at a dilution of 1:10 000. Membranes were also probed with a β-actin antibody (AC15; Sigma-Aldrich, St Louis, MO) at a dilution of 1:100 000. Blots were incubated for 1 hour at room temperature with alkaline phosphatase-conjugated antimouse (KPL, Gaithersburg, MD) secondary antibody diluted 1:1000. This was followed by washing in TBST, rinsing with dH2O, and incubation with ECF substrate (Amersham Biosciences, Piscataway, NJ) for 5 minutes at room temperature. Proteins were visualized by a STORM 840 Phoshorimager (Molecular Dynamics, Piscataway, NJ).
PCR amplification of MTAP exon 8
Genomic DNA was isolated using a genomic DNA isolation kit from GIBCO BRL (Gaithersburg, MD). Polymerase chain reaction (PCR) amplification of exon 8 of MTAP was performed using 50 ng of genomic DNA as described previously.20
MTAP and GAPDH RT-PCR
Two micrograms of total RNA was reverse-transcribed by use of the SUPERSCRIPT II TM First Strand Synthesis System for reverse transcriptase (RT)-PCR (Invitrogen). MTAP PCR was performed in a 50-μL reaction volume containing 1 μL cDNA, 1 × reaction buffer (Applied Biosystems, Foster City, CA), 1.0 mM MgCl2, 0.04 mM dNTP mix, 10 pmol of each primer, and 1U Taq polymerase (Amplitaq Gold; Applied Biosystems). Primers used for MTAP were MTAP469F, GACCACTATGAGACCTCAGTC; and MTAP973AS, TTAATGTCTTGGTAATAAAACAGAAAACTGGG. Primers used for GAPDH were GAPDHS, TGGTATCGTGGAAGGACTCATGAC; and GAPDH-AS, ATGCCAGTGAGCTTDCCCGTTCAGC. Samples were denatured and the enzyme activated for 12 minutes at 94°C followed by 24 cycles (21 for GAPDH) of 94°C (30 s), 58°C (30 s), and 72°C (60 s).
Results
Sensitivity of primary relapse T-ALL to cytotoxicity of L-alanosine
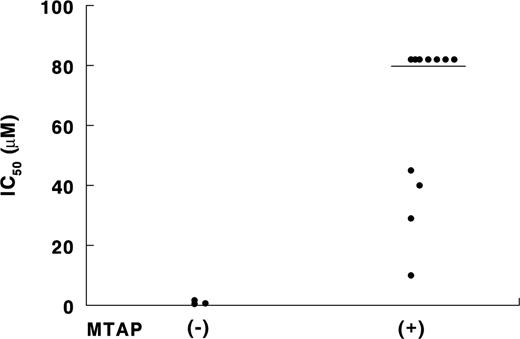
We have previously established that MTAP- primary T-ALL cells obtained from patients at diagnosis are more sensitive to the cytotoxicity of L-alanosine than are MTAP+ cells.20 Similarly, among 14 relapsed patients in the present study, MTAP- T-ALL cells displayed increased sensitivity to L-alanosine over MTAP+ cells. The average L-alanosine IC50 for 3 MTAP- T-ALL was 1.0 ± 0.6 μM and that for 4 MTAP+ patients was 31.0 ± 15.5 μM, with the remaining 7 MTAP+ patients having an IC50 of greater than 80 μM (Figure 2). MTAP status of T-ALL cells was determined by PCR and/or Western blot analysis as described in “Materials and methods” (data not shown). These findings indicate that MTAP- T-ALL cells at relapse are as sensitive to L-alanosine as those at diagnosis that had an IC50 of 4.8 ± 5.3 μM L-alanosine (range, 0.3-11.3 μM) in our previous study.19 Our results suggest that L-alanosine would be an effective chemotherapeutic agent for MTAP- T-ALL at both diagnosis and relapse. This finding is especially important since initial clinical trials of L-alanosine will be conducted in patients with relapsed T-ALL, which is often resistant to standard chemotherapy.
Synthesis and stability of EFA
To further increase the therapeutic index of L-alanosine, it is desirable to include a substrate of MTAP in combination with L-alanosine as a salvage agent for normal cells that constitutively express MTAP. MTA, the endogenous MTAP substrate, is significantly toxic to cells, especially to bone marrow progenitors (Figure 3A; Yu et al19 ), and thus is not an ideal salvage agent for normal cells as part of an MTAP-selective therapy using L-alanosine. For this reason, a less toxic MTAP substrate, EFA, was prepared and evaluated as a salvage agent for normal cells. EFA was prepared (see “Materials and methods”) by condensing D-erythrose triacetate with a suitable trimethylsilylated base in the presence of a Lewis acid catalyst such as trimethylsilyl trifluoromethane sulfonate. The use of 2,6-dichloropurine as the base exclusively provides the desired 9-β-D product with no significant amount of the 7-isomer being observed. Treatment of the dichloro intermediate with ammonia in methanol followed by replacement of the 2-chloro group by hydrogen furnished EFA (Figure 1).
Sensitivity of primary T-ALL from relapsed patients to L-alanosine. Primary T-ALL cells from relapsed patients were treated with increasing concentrations of L-alanosine for 3 days. Control cells were cultured in media alone. Cells were then pulsed with 3H-thymidine for 6 hours and incorporation of 3H-thymidine was determined in a scintillation counter. MTAP status was determined by PCR and/or Western blot analysis. Horizontal line separates primary T-ALL cells that are resistant to the cytotoxicity of L-alanosine (IC50 ≥ 80 μM) from those that are sensitive.
Sensitivity of primary T-ALL from relapsed patients to L-alanosine. Primary T-ALL cells from relapsed patients were treated with increasing concentrations of L-alanosine for 3 days. Control cells were cultured in media alone. Cells were then pulsed with 3H-thymidine for 6 hours and incorporation of 3H-thymidine was determined in a scintillation counter. MTAP status was determined by PCR and/or Western blot analysis. Horizontal line separates primary T-ALL cells that are resistant to the cytotoxicity of L-alanosine (IC50 ≥ 80 μM) from those that are sensitive.
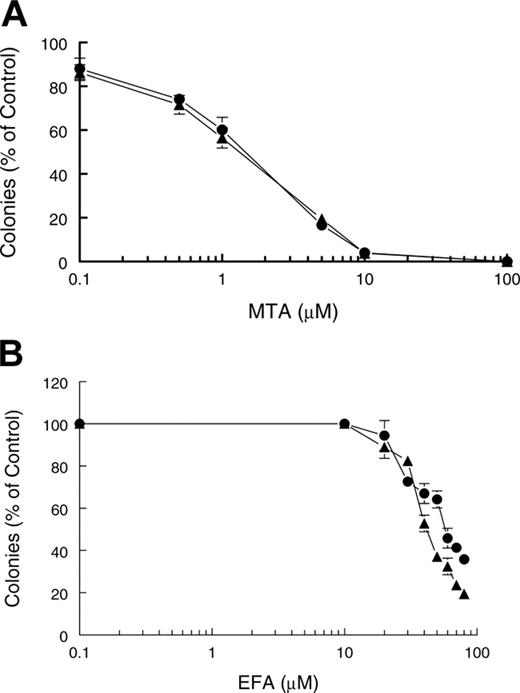
Effect of MTA and EFA on normal bone marrow BFU-Es and CFU-GMs. Bone marrow cells were treated with increasing concentrations of (A) MTA or (B) EFA for 14 days after which (•) BFU-Es and (▴) CFU-GMs were enumerated as described in “Materials and methods.” All assay conditions were performed in triplicate and error bars represent standard deviation.
Effect of MTA and EFA on normal bone marrow BFU-Es and CFU-GMs. Bone marrow cells were treated with increasing concentrations of (A) MTA or (B) EFA for 14 days after which (•) BFU-Es and (▴) CFU-GMs were enumerated as described in “Materials and methods.” All assay conditions were performed in triplicate and error bars represent standard deviation.
EFA remained stable in solution at room temperature at 97.2% purity with no degradation products over a 48-hour period of monitoring by HPLC (data not shown). As a solid stored at room temperature, EFA was determined to be stable for several years by monitoring decomposition products.
EFA is less toxic than MTA against hematopoietic progenitor cells
Hematopoietic progenitor cells are very sensitive to the toxicity of many chemotherapeutic agents, including L-alanosine, posing a limitation in cancer therapy. To evaluate the suitability of EFA as a salvage agent for normal hematopoietic cells from L-alanosine cytotoxicity, the sensitivity of hematopoietic progenitor cells to MTA (Figure 3A) and EFA (Figure 3B) was assessed in a colony-formation assay. The toxicity of EFA to BFU-Es and CFU-GMs was significantly less than that of MTA. The IC50 of EFA was 57 μM for BFU-Es and 42 μM for CFU-GMs (Figure 3B). In contrast, the IC50 for MTA was 1.6 μM for BFU-Es and 1.4 μM for CFU-GMs (Figure 3A).19 These results indicate that EFA would be a superior salvage agent for normal cells.
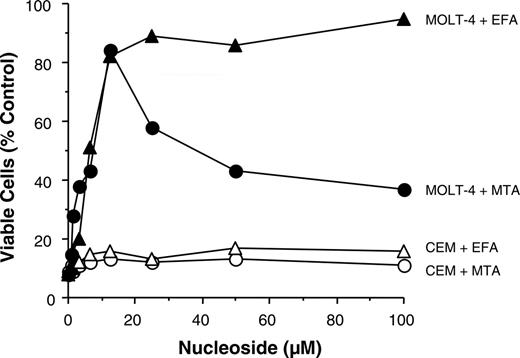
EFA is superior to MTA in salvaging a MTAP+ T-ALL cell line from L-alanosine toxicity
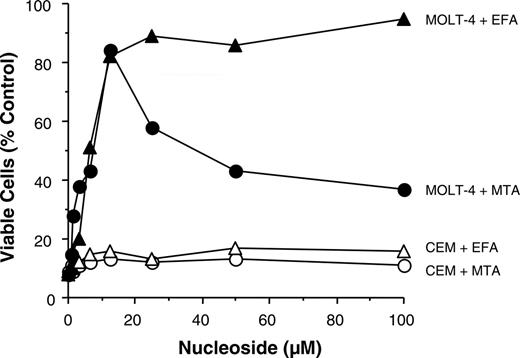
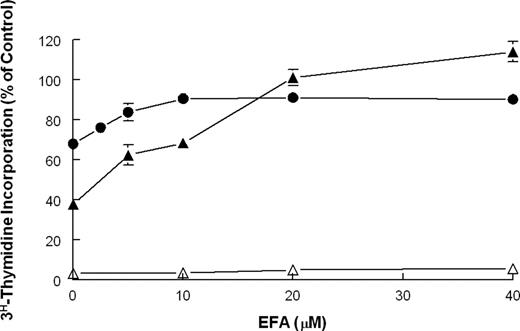
The ability of EFA to selectively rescue MTAP+ cells from L-alanosine toxicity was examined by determining cell viability after treatment of MOLT-4 (MTAP+) and CEM (MTAP-) cells with 40 μM L-alanosine in the presence of increasing concentrations of EFA or MTA for 72 hours. The results demonstrated that EFA effectively rescued MTAP+ MOLT-4 cells from L-alanosine toxicity with cell viability at 90% of control at 25 μM EFA (Figure 4). Even with EFA concentrations as high as 100 μM, there was little cytotoxicity with cell viability remaining at at least 90% of control. In contrast, although significant rescue (84% of control) was achieved with MTA at 12.5 μM, higher concentrations of MTA were quite toxic (Figure 4). At concentrations greater than 20 μM, MTA was also toxic to PHA-stimulated lymphocytes from healthy donors in an independent experiment (data not shown). Neither salvage agent rescued MTAP- CEM cells as expected (Figure 4). Collectively, the results indicate that EFA is a far more effective salvage agent than MTA due to its lower cytotoxicity.
Selective rescue of MTAP+ T-ALL cell line from L-alanosine toxicity by EFA or MTA. CEM and MOLT-4 human T-ALL cell lines were treated with 40 μM L-alanosine in the presence of increasing concentrations of EFA or MTA. Cells were cultured for 72 hours and viable cells were quantified using an XTT colorimetric assay kit. ▴ indicates MOLT-4 + EFA; •, MOLT-4 + MTA; ▵, CEM + EFA; ○, CEM + MTA.
Selective rescue of MTAP+ T-ALL cell line from L-alanosine toxicity by EFA or MTA. CEM and MOLT-4 human T-ALL cell lines were treated with 40 μM L-alanosine in the presence of increasing concentrations of EFA or MTA. Cells were cultured for 72 hours and viable cells were quantified using an XTT colorimetric assay kit. ▴ indicates MOLT-4 + EFA; •, MOLT-4 + MTA; ▵, CEM + EFA; ○, CEM + MTA.
Rescue of normal PBMCs and primary MTAP+ T-ALL cells from L-alanosine toxicity by EFA
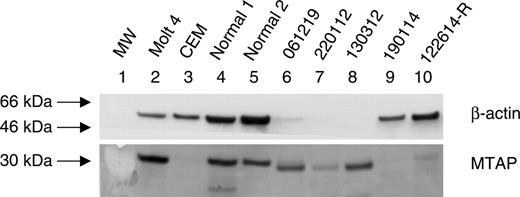
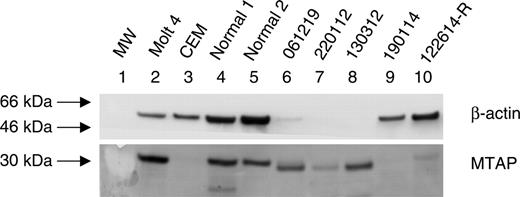
In order to confirm the effectiveness of EFA as a salvage agent for MTAP+ cells, both MTAP+ and MTAP- primary T-ALL cells as well as PHA-stimulated PBMCs obtained from healthy donors were treated with 20 or 40 μM L-alanosine in the presence of increasing concentrations of EFA for 72 hours. Cell proliferation was then measured by a 3H-thymidine incorporation assay. The MTAP status of patient T-ALL cells was determined by Western blot analysis and the results are displayed in Figure 5. Very limited protein was available from T-ALL cells of patients 061219, 220112, and 130312, as evidenced by the lack of detection of β-actin in these samples. However, despite low levels of protein, MTAP was detected in these samples as well as in PBMCs from healthy donors and MOLT-4 cells (positive control). MTAP protein was not detected in T-ALL cells of patients 190114 and 122614-R, nor was it detected in CEM cells that lack the MTAP gene. Primary T-ALL cells (patient 061219) that expressed MTAP were rescued from L-alanosine toxicity by 20 μM EFA, whereas MTAP- T-ALL cells (patient 190114) were not rescued even at 40 μM EFA in a representative experiment (Figure 6). Similarly, PHA-stimulated lymphocytes from a healthy donor were rescued from L-alanosine toxicity by EFA at 20 μM (Figure 6). Interestingly, PHA-stimulated lymphocytes from 2 other healthy donors were relatively insensitive to the toxicity of 40 μM L-alanosine (data not shown). The results of similar experiments obtained with 7 T-ALL patients, including 2 who relapsed (patients 122614-R and 131518-R), are summarized in Table 1. In these experiments, cells were treated with 40 μM L-alanosine and increasing concentrations of EFA. Rescue of MTAP+ primary T-ALL cells from L-alanosine toxicity was observed with EFA concentrations as low as 2.5 μM (patient 131518-R) but generally required 20 μM EFA (Table 1). T-ALL cells that lacked MTAP protein (patients 190114 and 122614-R) were not rescued by EFA (Figure 6; Table 1). Interestingly, although T-ALL cells of patient 260512 harbored the MTAP gene based on PCR analysis and expressed message (Table 1; data not shown), these cells were not rescued from L-alanosine toxicity by EFA, presumably because the MTAP protein was not expressed. Protein was not available from this sample to confirm the lack of MTAP protein. A lack of rescue by EFA was also observed with T-ALL cells of patient 122614-R (Figure 6; Table 1), which harbored the MTAP gene and expressed message (Table 1; data not shown) but did not express MTAP protein (Figure 5). The very small amount of rescue observed with this sample is most likely due to the presence of contaminating normal cells, as these samples, especially from relapse patients, are never 100% pure. Taken together, these data indicate that EFA is an effective agent for the salvage of MTAP+ cells from L-alanosine toxicity.
Expression of MTAP in primary T-ALL and PBMCs from a healthy donor. Protein was extracted and subjected to Western blot analysis as described in “Materials and methods.” Membrane blots were probed with an MTAP antibody followed by an alkaline phosphatase-conjugated antimouse secondary antibody. Membranes were also probed with a β-actin antibody as a control for protein loading. Proteins were visualized using a STORM 840 Phoshorimager. Protein from MOLT-4 and CEM cell lines were used as a positive and negative control, respectively. MW indicates molecular weight standards.
Expression of MTAP in primary T-ALL and PBMCs from a healthy donor. Protein was extracted and subjected to Western blot analysis as described in “Materials and methods.” Membrane blots were probed with an MTAP antibody followed by an alkaline phosphatase-conjugated antimouse secondary antibody. Membranes were also probed with a β-actin antibody as a control for protein loading. Proteins were visualized using a STORM 840 Phoshorimager. Protein from MOLT-4 and CEM cell lines were used as a positive and negative control, respectively. MW indicates molecular weight standards.
Discussion
The antitumor activity of L-alanosine was first reported 4 decades ago. However, its potential as a selective agent became apparent only in the recent years when we (Batova et al20 ) and others (Hori et al33 ) established that MTAP-deficient cancer cells were more sensitive to L-alanosine toxicity than normal cells with abundant MTAP. To date, numerous cancers including acute nonlymphoid leukemia, T-ALL, non-small-cell lung cancer, melanoma, rectal and breast carcinoma, glioma, mesothelioma, and soft-tissue sarcoma have been reported to be deficient in MTAP and possibly more remain to be identified.3-9,11,14,15,34-36 Among these, glioma,11 mesothelioma,16 and metastatic melanoma36 have an incidence of MTAP inactivation of greater than 50%. The significant number of cancer types with MTAP deficiency combined with the high incidence of MTAP inactivation in some of these tumors underscores the importance of MTAP-targeted chemotherapy with agents such as L-alanosine. The ability of L-alanosine to circumvent chemoresistance as a consequence of MDR expression makes this agent even more attractive.37 Our finding that relapsed T-ALL cells are as sensitive to L-alanosine as diagnosis samples lends further support for the therapeutic potential of L-alanosine for cancers resistant to standard chemotherapy.
Selective rescue of normal PBMCs and MTAP+ primary T-ALL from L-alanosine toxicity by EFA. Primary T-ALL and PHA-stimulated lymphocytes from a healthy donor were treated with 20 μM and 40 μM L-alanosine, respectively, and with increasing concentrations of EFA for 3 days. Control cells were cultured in media alone. Cells were then pulsed with 3H-thymidine for 6 hours and incorporation of 3H-thymidine was determined in a scintillation counter. All culture conditions were performed in triplicate and error bars represent standard deviation. ▴ indicates normal PBMCs; •, MTAP+ T-ALL patient 061219; and ▵, MTAP- T-ALL patient 122614-R (relapsed patient).
Selective rescue of normal PBMCs and MTAP+ primary T-ALL from L-alanosine toxicity by EFA. Primary T-ALL and PHA-stimulated lymphocytes from a healthy donor were treated with 20 μM and 40 μM L-alanosine, respectively, and with increasing concentrations of EFA for 3 days. Control cells were cultured in media alone. Cells were then pulsed with 3H-thymidine for 6 hours and incorporation of 3H-thymidine was determined in a scintillation counter. All culture conditions were performed in triplicate and error bars represent standard deviation. ▴ indicates normal PBMCs; •, MTAP+ T-ALL patient 061219; and ▵, MTAP- T-ALL patient 122614-R (relapsed patient).
The provision of an MTAP substrate in combination with L-alanosine increases the tumor selectivity of L-alanosine since the MTAP substrate provides a source of adenine for normal cells and thereby allows the rescue of normal cells, whereas MTAP-deficient tumor cells are killed. Thus, the therapeutic index of L-alanosine can be increased by the administration of a MTAP substrate in combination with L-alanosine. The endogenous MTAP substrate, MTA, as well as 5′-deoxyadenosine have associated toxicities and thus are not ideal salvage agents. MTA is toxic to hematopoietic progenitor cells in vitro with an IC50 equal or less than 1 μM as reported by us (Yu et al19 ) previously and as demonstrated in this study. This toxicity is presumably due to feedback inhibition of polyamine synthesis. 5′-deoxyadenosine is a partial agonist of adenosine receptors38 and thus is prone to the toxicities observed with adenosine including inflammation, immunosuppression, and vasodilation.29,30,39,40 In an effort to generate an MTAP substrate without the toxicities associated with adenosine, EFA was synthesized and evaluated as a salvage agent to rescue MTAP+ cells from L-alanosine toxicity. EFA has previously been shown to be a competitive inhibitor at adenosine receptors38 and thus would not elicit the toxicities associated with adenosine. Whether EFA would have any in vivo toxicity due to its action as a competitive inhibitor of adenosine remains to be determined. Our results have demonstrated that EFA selectively rescues MTAP+ cells in vitro, including PHA-stimulated normal lymphocytes, without the toxicity observed with MTA. Furthermore, EFA was at least 26- to 41-fold less toxic than MTA against hematopoietic progenitors in colony-forming assays. Taken together, our results indicate that EFA would be a more optimal salvage nucleoside than MTA. In conclusion, the results of the current study lay the foundation for clinical trials of L-alanosine in combination with EFA in the treatment of MTAP- cancers including those refractory to standard chemotherapy.
Prepublished online as Blood First Edition Paper, October 18, 2005; DOI 10.1182/blood-2005-06-2430.
Supported by grants from Leukemia & Lymphoma Society 6184 (A.L.Y.) and from the Cindy Matters Fund (A.L.Y.) and in part by Grants MO1 RR00827 from the General Clinical Research Center program and by Genomics Research Center, Academia Sinica (J.Y. and A.L.Y.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.