The incidence of follicular lymphoma (FL) in industrialized countries has been increasing since the 1950s. Polymorphisms in genes encoding key enzymes controlling folate-methionine metabolism, including methylenetetrahydrofolate reductase (MTHFR), methionine synthase (MS or MTR), serine hydroxymethyltransferase (SHMT), and thymidylate synthase (TS or TYMS), modify the risk of various cancers and possibly FL. This study specifically looks for an association between MTHFR, MTR, TYMS, and SHMT polymorphisms and the risk of FL. We carried out a case-control study with 172 patients diagnosed with FL and 206 control subjects. We report that the risk of FL was doubled by the association of one mutant allele at both MTHFR polymorphisms. Individuals with MTR 2756AA had 2-fold higher risk of FL, and subjects not having at least one TYMS 2R allele showed a 2-fold higher risk of FL. The MTR 2756AA genotype conferred a greater multivariate-adjusted relative risk of FL, and the risk was multiplied by almost 5 in the TYMS2R(-)/MTR 2756AA combination. In conclusion, common polymorphisms in key enzymes of the folate-methionine metabolism pathway result in an increased risk of FL and suggest that inadequate intake of dietary folate and other methyl donor nutrients may contribute to the development of this malignancy. (Blood. 2006;108:278-285)
Introduction
The incidence of both follicular lymphoma (FL) and other nonHodgkin lymphomas (NHLs) has been steadily rising since the 1950s.1-3 Although this remains mostly unexplained, it has been suggested that greater exposure to environmental carcinogens, particularly to pesticides and solvents, may be responsible.4-7 Moreover, susceptibility to genomic damage has also been linked to dietary folate deficiency, because this metabolic pathway is important for both nucleotide synthesis and methylation. The genes encoding folate metabolic enzymes display several single nucleotide polymorphisms (SNPs)—for example, methylenetetrahydrofolate reductase (MTHFR C677T and MTHFR A1298C), serine hydroxymethyltransferase (SHMT C1420T), and methionine synthase (MS or MTR A2756G)—and variable number tandem repeats (VNTRs) for thymidylate synthase (TS or TYMS VNTR 2R and 3R). The corresponding common variants decrease or increase the enzymatic activity of the proteins encoded8-10 and have been implicated in the development of adult and childhood acute lymphocytic leukemia (ALL)11-16 and in various other malignan cies including endometrial cancer,17 cervical intraepithelial neoplasia,18,19 colon cancer,20 and pancreatic cancer.21
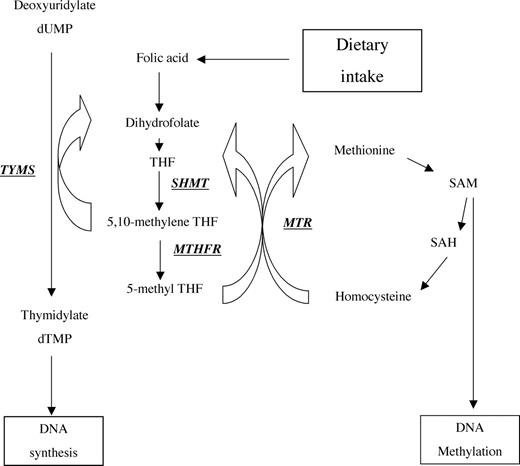
Methylenetetrahydrofolate reductase (MTHFR) catalyzes the reduction of 5,10-methylenetetrahydrofolate (methylene THF) to 5-methyltetrahydrofolate (5-methyl THF), the major circulatory form of folate and carbon donor for the remethylation of homocysteine to methionine (Figure 1). Thus, MTHFR provides the link between folate and homocysteine metabolism. It is also a critical enzyme in diverting one carbon from nucleic acid synthesis to methionine synthesis and methylation reactions. The MTHFR gene, which is located on chromosome 1p36, has 2 known polymorphisms involving nucleotide positions 677 (C→T; alanine→valine) and 1298 (A→C; glutamic acid→alanine). Both polymorphisms lead to reduced MTHFR activity, although to different extents, and result in the accumulation of 5,10-methylene THF and diminution of 5-methyl THF. The function of the second polymorphism, A1298C, in the C-terminal regulatory domain of the MTHFR gene remains controversial. Individuals with combined heterozygosity for 677CT/1298AC have been reported with reduced enzyme activities, elevated plasma homocysteine, and decreased plasma folate, similar to those with the 677TT genotype.10,22 Chen et al found that this polymorphism did not significantly correlate with plasma folate and homocysteine levels. The combined heterozygosity did not modify the colorectal cancer risk; nor was it significantly associated with plasma folate and homocysteine. It was concluded that the MTHFR A1298C polymorphism is a less important independent risk factor than the C677T polymorphism for colorectal cancer.22
Recently, in a large NHL population-based case-control study including DLCL subtype (diffuse large cell and immunoblastic lymphoma) and FL subtype (follicular small, mixed, and large cell lymphomas), Skibola et al11 found significant associations for several genes involved in folate metabolism. The MTHFR 677TT genotype was associated with borderline increased risk of FL (odds ratio [OR], 1.8; 95% confidence interval [CI], 0.98-3.1).
Overview of folate and methionine metabolic pathways. TYMS binds methylenetetrahydrofolate (5,10-methylene THF), which serves as a hydroxymethyl donor in the conversion of dUMP to dTMP in the DNA synthesis pathway. SHMT catalyzes the reversible conversion of serine and THF to glycine and methylene THF. MTHFR catalyzes the reduction of 5,10-methylene THF to 5-methyl THF. MTR catalyzes the transfer of methyl base from 5-methyl THF to homocysteine. Adapted From Matsuo et al15 with permission.
Overview of folate and methionine metabolic pathways. TYMS binds methylenetetrahydrofolate (5,10-methylene THF), which serves as a hydroxymethyl donor in the conversion of dUMP to dTMP in the DNA synthesis pathway. SHMT catalyzes the reversible conversion of serine and THF to glycine and methylene THF. MTHFR catalyzes the reduction of 5,10-methylene THF to 5-methyl THF. MTR catalyzes the transfer of methyl base from 5-methyl THF to homocysteine. Adapted From Matsuo et al15 with permission.
Methionine synthase (MS or MTR), a vitamin B12-dependent enzyme, catalyzes the transfer of methyl base from 5-methyl THF to homocysteine, producing methionine and tetrahydrofolate (THF) (Figure 1). The gene is located on chromosome 1q43.9 MTR is critical for maintaining an adequate intracellular S-adenosylmethionine (SAM) level for DNA methylation and ensuring that homocysteine concentrations do not reach toxic levels. SAM is a crucial methyl group donor involved in more than 100 methylation reactions including DNA methylation. Severe deficiency of vitamin B12 or of MTR causes hypomethioninemia, hyperhomocysteinemia, and hyperhomocystinuria. An A2756G (aspartic acid→glycine) polymorphism resulting in a lower enzyme activity was found among healthy individuals9 and was thought to result in homocysteine elevation and DNA hypomethylation.23 However, plasma levels of folate, vitamin B12, and homocysteine did not differ significantly between MTR genotypes, in contrast to the MTHFR polymorphisms.23
Serine hydroxymethyltransferase (SHMT), a vitamin B6-dependent enzyme,24 catalyzes the reversible conversion of serine and THF to glycine and methylene THF. There are 2 SHMT isoenzymes: One is found in the cytosol and is encoded by the SHMT1 gene on chromosome 17p11.2, and the other is in mitochondria and is encoded by the SHMT2 gene on chromosome 12q13. SHMT is pivotal in providing one-carbon units for purine, thymidylate, and methionine synthesis as well has having other metabolic functions.25 Recently, a C1420T polymorphism (L474F also numbered C1444T) has been described that results in low plasma and red blood cell folate levels in individuals homozygous for the 1420C allele.26 In a case-control study on ALL, individuals carrying the 1420T allele exhibited a decrease in ALL risk.12 In a large series of 458 NHL cases, Skibola et al11 did not observe any significant differences in genotype frequencies of the SHMT1 and the reduced folate carrier gene polymorphisms between the cases and controls. In view of the role of SHMT in the provision of one-carbon units for numerous folate pathways, disturbances in protein expression or enzyme activity due to this polymorphism could mimic a folate deficiency by limiting the availability of one-carbon moieties for both remethylation of homocysteine and DNA synthesis.
Thymidylate synthetase (TS or TYMS) catalyzes the conversion of dUMP to dTMP and thus plays a critical role in maintaining a balanced supply of deoxynucleotides required for DNA synthesis (Figure 1). The substrate for TYMS, 5,10-methylene THF, is a central metabolite in folate metabolism and is diverted into a variety of pathways, including thymidine synthesis, purine synthesis, and toward the provision of methyl groups for DNA methylation. The gene is located on chromosome 18p11.32. TYMS has a unique tandem repeat sequence in the 5′ untranslated region (UTR) immediately upstream from the ATG initiation codon that is polymorphic, containing either 2 (2R) or 3 (3R) 28-bp repeats.27 Repeated sequences in TYMS are believed to regulate TYMS gene expression by forming secondary structures in the 5′-terminal domain of the TYMS mRNA.28
We hypothesized that changes in the expression levels or activity of these key enzymes associated with the folate-methionine metabolic (Figure 1) polymorphisms may affect the risk of chromosomal translocations and DNA hypermethylation at particular gene promoters. These phenomena are common features of lymphoproliferative disorders such as malignant FL.15,16,29 We therefore conducted a retrospective study of 5 polymorphisms in these 4 genes (MTHFR, MTR, SHMT, and TYMS) using DNA from stored tissue samples from 172 anonymous patients, each with a confirmed diagnosis of FL. We also studied a group of 206 healthy control subjects for comparison.
Patients, materials, and methods
Study population
All subjects included were unrelated whites. A total of 172 DNA samples were collected from FL patients (98 men and 74 women) recruited at the Necker-Enfants Malades Hospital (B.V. and E.M., Paris, France) and the Lyon Sud Hospital (G.S., Lyon, France) between 1990 and 2000. Approval was obtained from the participating institutional review boards for these studies. Informed consent was provided according to the Declaration of Helsinki. All DNA samples were made anonymous to preserve confidentiality. A group of anonymous healthy controls (n = 206) was recruited from the CEPH (Centre d'Etudes du Polymorphisme Humain) and UR383 laboratory personal cohort.
Genotype analyses
DNA from cases and controls was extracted from total blood samples using a Wizard kit (Promega, Madison, WI) or from Ficoll-collected peripheral blood mononuclear cells by classic phenol chloroform extraction. Patients were selected on the basis of their having histologically confirmed FL according to the World Health Organization (WHO) classification and having undergone DNA analysis for molecular detection of BCL2-IgH rearrangement and/or IgH clonality; to avoid contamination with tumoral DNA, only blood samples that were BCL2-IgH negative were analyzed.
Genotyping was performed as follows. DNA (20 ng) was amplified in a total volume of 20 μL polymerase chain reaction (PCR) buffer (50 mM KCl, 10 mM Tris-HCl pH 8.3), 0.2 mM dNTP, 10 pmol forward and reverse primer (Table 1), 1.5 mM MgCl2, and 1 unit of Taq polymerase (Invitrogen, Carlsbad, CA). Standard conditions for PCR cycling were initial denaturation at 94°C for 5 minutes followed by 35 cycles of 94°C for 10 seconds and 10 seconds of annealing and elongation at 72°C for 20 seconds (Primus; MWG Biotech, Ebersberg, Germany). The resulting fragments were analyzed by denaturing high performance liquid chromatography (dHPLC) (Transgenomic, Elancourt, France).
Statistical analysis
The frequencies of each genotype were calculated as q = (2a+b)/n, where a equals the number of homozygotes, b equals the number of heterozygotes, and n equals the number of alleles analyzed. Contingency tables were used to assess the statistical significance of the differences in the distribution of genotypes between cases and controls. For groups of fewer than 5 individuals, the Fisher exact test was used. The level of significance was set at P = .05. The relative risk associated with certain genotypes was estimated by calculating crude ORs with 95% CIs. Subsequent analysis included logistic regression analyses. Following this univariate analysis, we next investigated possible gene-gene interactions using multiplicative interaction terms in a conditional logistic regression model. The level of significance was set at a P value of .05. Statview software (Abacus concept) was used for statistical analyses. Power calculation was performed using R software “bpower” function, “Hmisc” library. The power of the test given the observed data was provided as well as the power to detect an association for different values of OR—namely 1.5, 2.0, and 2.5 (Table 2).
Results
Study population and sample collection
The average age of the control group was 30 years, and the average age of the patients with FL was 56 years. The 2 groups could not be completely paired according to age. However, because the incidence of FL in the general population is low (3.3 per 100 000), we considered the age difference between the 2 groups to be negligible for the purposes of this study. The observed and expected genotype frequency distributions were similar in the control group for each polymorphism analyzed, in accordance with the Hardy-Weinberg equilibrium, indicating that there was no selective mechanism for a specific genotype. The comparison between the distributions of genotypes in our French control population and in other published white populations did not show any difference.11
Genotyping and univariate analyses of MTHFR, MTR, SHMT, and TYMS polymorphisms
Genotype frequencies of MTHFR C6777T, MTHFR A1298C, MS or MTR A2756G, SHMT C1420T, and TS or TYMS tandem repeats were determined in the cases and controls (Table 2). With the exception of TYMS, the genotypes could be assigned to 3 functional classes with 0 (wild type [w]/w), 1 (w/mutant [m]), or 2 (m/[m]) variant alleles associated with phenotypic changes. All subjects were assigned a genotype based on this classification MTHFR C677T and MTHFR A1298C: The allele frequency of the MTHFR C677T mutant allele was 33.3% and 36.6% in the controls and in the patients, respectively; that of the MTHFR A1298C mutant allele was 27.2% and 31.9% in the patients and in the controls, respectively. Because this enzyme is active in several related metabolic pathways, the polymorphisms were evaluated against the background of various other genotypes. Using MTHFR 677CC as the reference group, individuals with the MTHFR 677CT/TT genotypes had an OR of 1.32 (95% CI, 0.873-1.994; P = .189). Using MTHFR 1298AA as the reference group, individuals with the MTHFR 1298AC/CC genotypes had an OR of 1.25 (95% CI, 0.831-1.884; P = .284) (Table 2). The estimated risk was below 1.0 for each combination of alleles, but statistical significance could not be satisfactorily assessed because of the small number of patients.
Although the 1298AC and 1298CC genotypes are associated with a smaller (65% of the control value) impairment of MTHFR enzyme activity than 677CT or 677TT, heterozygotes for both mutations have lower MTHFR enzyme activity (similar to that associated with the 677TT genotype). Individuals who were heterozygous for the C677T mutation alone did not have higher than wild-type homocysteine values, whereas double heterozygotes (C677T/A1298C) had higher fasting homocysteine than single heterozygotes for the C677T variant.10,30 They also had higher homocysteine and lower plasma folate levels than heterozygotes for either one mutation alone.
We tested for associations between susceptibility to FL and each of the MTHFR 677 and 1298 genotypes, but the ORs were not significant; this may have been either a true negative result or a consequence of lack of power because of the relatively small numbers of individuals with the 1298CC genotype (17 cases and 15 controls). We next investigated the joint effects of the 2 polymorphisms (Table 3). We grouped the individuals according to the association of at least one mutant allele on each polymorphism, based on a possible synergetic effect of mutant alleles 677 and 1298.10 We defined a group, B, in which individuals harbored at least one variant allele at either MTHFR 677 and 1298: Group B thus comprised the 677CT/1298AC, 677CT/1298CC, 677TT/1298AC, and 677TT/1298CC genotypes. Group A (reference group) consisted of all the other genotypes: 677CC/1298AA, 677CC/1298AC, 677CC/1298CC, 677CT/1298AA, and 677TT/1298AA (Table 3). We found that group B individuals were at a 2-fold greater risk than group A individuals for developing FL.
MTR A2756G
The allele frequency of the MTR 2756G mutant allele with lower enzyme activity was 15.3% for controls and 8.8% for patients. Frequencies of the MTR 2756AA, MTR 2756AG, and MTR 2756GG genotypes were 72.3%, 24.8%, and 2.9%, respectively, for controls, and 84.2%, 14%, and 1.8% for patients (χ2, 7.62; P = .02). The risk of FL for MTR 2756AG individuals was half that for MTR 2756AA individuals' risk (OR, 0.49; 95% CI, 0.29-0.83; P = .009), and that for the MTR 2756AA genotype was double that for the MTR 2756AG/GG genotypes (OR, 2.04; 95% CI, 1.22-3.41; P = .006) (Table 2).
SHMT1 C1420T
The allele frequency of the SHMT1 1420T mutant allele was 32.7% for controls and 29.9% for patients. Frequencies of the SHMT 1420CC, SHMT 1420CT, and SHMT 1420TT genotypes were 44.4%, 45.8%, and 9.8%, respectively, for controls and 49.1%, 42%, and 8.9% for patients. Comparing the SHMT1 1420CC genotype with SHMT 1420CT/TT genotypes gave no evidence of any association between susceptibility to FL and the SHMT1 C1420T polymorphism (OR, 1.21; 95% CI, 0.80-1.82; P = .362) (Table 3).
TS or TYMS tandem repeats
The allele frequency of the TYMS triple tandem repeat 3R allele was 40% in the controls and 55.6% in the cases (P < .001). The TYMS 2R/2R genotype was present in 38.2% of the controls and 22.7% of the cases, the 2R/3R genotype in 42.2% of the controls and 42.0% of the cases, and the 3R/3R genotype in 18.6% of the controls and 34.1% of the cases. Until recently, only 2 forms of this tandem repeat (2R and 3R) had been described,31,32 but other variant forms (4R, 5R, and 9R) have been reported recently.33,34 However, the influence of these novel variant forms (1R and 4R) on TYMS gene expression is still unknown. We also found other numbers of tandem repeats, including 2R/4R (0.5% of controls and 1.1% of cases) and 1R/3R (0.5% of controls and 0% of cases) in our white subjects.
We calculated the ORs for individuals without the 2R allele by comparison with those with at least one 2R allele, based on the hypothesis that gene expression would be greater the larger the number of TYMS 28-bp repeats. Using those harboring at least one TYMS 2R allele (2R+) as the reference, subjects harboring the TYMS 3R/3R genotype (no TYMS 2R allele or 2R-) had double the risk of developing FL (OR, 2.12; 95% CI, 1.32-3.4; P = .002) (Table 2).
Bivariate (interaction) analyses
ORs were determined for combinations of the genes MTR, TYMS, and MTHFR (Table 4).
The cases with at least one TYMS 2R allele (2R+) and MTR 2756AG/GG were defined as the reference group because they were expected to have the lowest susceptibility. The combination of the 2 genotypes at risk increased the ORs considerably. Indeed, the OR for TYMS 2Rassociated with MTR 2756AA was 4.75 (OR, 4.75; 95% CI, 2.25-10.03; P < .001). Thus, the genotypes TYMS 2R- and MTR 2756AA seem to have a synergetic effect on the risk of FL.
In the same way, using TYMS 2R+ associated with MTHFR group A as the reference, the OR was 3.88 for TYMS 2R- with MTHFR group B (OR, 3.88; 95% CI, 1.53-9.86; P = .004). Using MTHFR group A with MTR 2756AC/GG as the reference, we also found significantly increased ORs for the combination of the genotype MTR 27562756AA with genotypes of MTHFR group A (OR, 2.31; 95% CI, 1.24-4.28; P = .008) and of MTHFR group B (OR, 4.74; 95% CI, 2.24-9.86; P < .001). The MTR 756AA genotype therefore appears to play an important role in the synergetic effect with MTHFR group B genotypes.
Thus, the MTR 2756AA genotype confers roughly a 5-fold increased risk when it is combined with MTHFR group B or TYMS 2R-.
Power
Power was calculated for the observed OR (Table 2). It provided the power of the test given the observed data. For example, the power to detect the observed OR for MTHFR 1298AC/CC was 18%. We present the power to detect an association for different values of OR—namely, 1.5, 2.0, and 2.5. The power of the test given the observed data was low for MTHFR 677 and MTHFR 1298, MTR, and SHMT. As stated earlier, the power to detect, for example, the observed OR for MTHFR 1298AC/CC was 18%. However, we wondered whether the lack of significant association between FL risk and MTHFR 1298AC/CC polymorphism could be interpreted as the absence of association or as simply inconclusive. We thus calculated the power to detect an association for different values of OR—namely, 1.5, 2.0, and 2.5. For our example, this association would have been detectable with a power of 49%, 91%, and 99%, respectively.
Discussion
In the present study, we clearly found associations between various gene polymorphisms controlling folate metabolism and increased risk of FL. Analyses of combinations showed that MTHFR group B, MTR AA, and TYMS 2R- had the greatest susceptibility, and the statistical significance was high. Power calculations were performed to clarify whether the absence of any association could be interpreted as a true absence of association or a lack of statistical power. In addition to gene-nutrient interactions involving folate and other methyl donors, there were significant gene-gene interactions in the folate-methionine metabolism pathways that account for vulnerability to FL.
Deficiencies in thymidylate increase the rate of misincorporation of uridylate into DNA, which may in turn lead to an increased rate of DNA strand breaks and other chromosomal damage.35 Consequently, the reduced MTHFR activity of the MTHFR 677 and MTHFR 1298 variants, which leads to increased levels of cytosolic 5,10-methylene THF available for thymidylate synthesis, may protect cells from DNA damage induced by uridylate misincorporation. Accordingly, this variant was found to be protective against colorectal cancer and ALL. Consistent with this model, several independent studies have shown that the mutant (valine) allele of MTHFR may confer a 2-fold reduction in the risk of colon cancer36,37 and of NHL,15 and a 4-fold reduction in risk of ALL12,13,37 but no reduction in that of AML.37
Conversely, the MTHFR 677T variant has also been associated with a 2.8-fold increase in risk of endometrial cancer17 and with a 2.9-fold increase in risk of cervical intraepithelial neoplasia18,19 and pancreatic cancer.21 The increased risk associated with defective MTHFR alleles might be a consequence of impairment of DNA methylation due to a reduction in the availability of 5,10-methylene THF. Individuals who are homozygous for the mutant 677TT allele show a higher degree of genomic DNA hypomethylation than do homozygotes for the wild-type 677CC allele.38 Interestingly, however, these examples show that diametrically opposed effects may result from identical causes. This could be explained by different tissue/stage-specific requirements.
In the present study the lack of significant association between FL risk and MTHFR 677CT/TT and MTHFR 1298AC/CC polymorphism could be interpreted as the absence of association or as simply inconclusive. As an example, given the power, 49%, 91%, and 99%, to detect an association with the MTHFR 1298AC/CC polymorphism for different values of OR—namely 1.5, 2.0, and 2.5, respectively—our study would not allow us to conclude for these 2 individual polymorphisms considered independently. By contrast, grouping individuals harboring at least one variant allele at both MTHFR 677 and 1298 (group B), we found that group B individuals were at a statistically significant 2-fold greater risk than group A individuals for developing FL (P = .004). These results demonstrate the involvement of MTHFR.
Unlike our study, a previous work found that defective MTHFR alleles were associated with a reduced risk of malignant lymphoma.15 However, this case-control study used a smaller population of 98 cases and included various different lymphoma subtypes. In contrast, our study analyzed a larger population (172 subjects) and included only patients with a single lymphoma subtype: follicular lymphoma (FL). Moreover, our population was white, whereas the population investigated by Matsuo et al was Japanese. More recently, in a large population-based case-control study carried on 458 NHL white cases and 812 controls, including DLCL subtype and FL subtype, only borderline associations with MTHFR have been demonstrated. Haplotype B (677C-1298C) was associated with a borderline decrease in the NHL risk estimate (OR, 0.88). In addition, haplotype C (677C-1298A) was associated with a borderline increased risk of DLCL (OR = 1.2) and of FL (OR = 1.3).
The MTR 2756AA genotype increases the activity of the MTR enzyme, which results in an increase of the methionine level and DNA methylation. Lincz et al29 reported that the MTR 2756AG/GG genotypes conferred a 2.4-fold lower risk of FL but no lower risk of DLCL. In agreement with these results, we report that the MTR 2756AA genotype increased the risk of FL. Differences in DNA methylation status between NHL subtypes have not been thoroughly investigated, but it is likely that there are differences between classifications.39 In the study by Skibola et al11 on NHL subjects, MTR 2756AG/GG and MTHFR 677TT genotypes were associated with an increased risk of 30% for NHL and of 80% for FL.
In the present study, comparing the SHMT 1420CC genotype with SHMT 1420CT/TT genotypes gave no evidence of any association between susceptibility to FL and the SHMT C1420T polymorphism. This is in agreement with data from the large series of 458 NHL cases by Skibola et al.11 However, as already stated for MTHFR individual polymorphisms, the lack of power does not allow us to conclude for an absence of association. Interestingly, in a case-control study on ALL, Skibola et al12 found that individuals with SHMT1 1420CT exhibited a 2.1-fold decrease in ALL risk and the TT genotype conferred a 3.3-fold reduction in risk.
An increase in TYMS gene expression could disrupt the balanced supply of the 4 precursors for the replication and repair of DNA, especially in rapidly proliferating cells such as hematopoietic stem cells.40 Gene expression in vitro and in vivo is higher when the triple 28-bp repeat is present than when the double repeat is present.28,41 This enhanced expression may increase the conversion of dUMP to dTMP, reducing the level of uracil that might otherwise be incorporated into DNA. Impairments of the TYMS enzyme have been associated with chromosome damage and fragile site induction.42,43 We calculated the ORs for individuals without the 2R allele by comparison with those with at least one 2R allele, based on the hypothesis that gene expression would be greater the larger number of TYMS 28-bp repeats. Using those harboring at least one TYMS 2R allele (2R+) as the reference, subjects harboring the TYMS 3R/3R genotype (no TYMS 2R allele or 2R-) had double the risk of developing FL.
Studies by Hishida et al16 and Skibola et al37 found that the genotype 3R/3R without a 2R allele is, in contrast, protective against malignant lymphoma and adult ALL. In ALL, individuals with TYMS 2R3R exhibited a 2.8-fold reduction in ALL risk while the TYMS 3R3R genotype conferred an even greater level of protection of 4-fold.12 However, as shown by Skibola et al,11 the estimated OR for the 2R allele is also influenced by the presence or absence ofa6bp (1494del6) in the 3′UTR region. Taking the 3R/3R as the reference, the 2R/2R genotype was associated with a 50% increased risk of NHL individuals carrying the 6bp+6bp+ genotype.11 In the same study, 3 other different TYMS genotypes, in linkage disequilibrium, were all inversely associated with a decreased risk of 43% and 71% in NHL and DLCL, respectively.11
It seems reasonable that each potentially at-risk genotype for a multifactorial disease has low penetrance if considered alone. Combinations of such genotypes would be expected to increase the risk of FL. Indeed, we found significantly increased ORs for the combination of the genotype MTR 2756AA with genotypes of MTHFR group A and of MTHFR group B. In the study by Skibola et al,12 the MTR 2756AG/GG and MTHFR 677TT genotypes were associated with an increased risk of 30% for NHL and of 80% for FL.12 The OR for TYMS 2R-associated with MTR 2756AA was 4.75. The combination of TYMS 2R- with MTHFR group B genotypes increased susceptibility by a factor 4. Our results suggest that an enhanced availability of methylene THF and the consequent increase in dTMP production in the DNA synthesis pathway due to TYMS tandem repeat polymorphisms and MTHFR (677 and 1298) polymorphisms might contribute to FL oncogenicity. Thus, testing several genes belonging to the same pathway or biologic system is a potentially powerful method for evaluating the combined effect of candidate genes and may be the basis for a potentially clinically useful assessment of an individual's risk of a specific type of cancer.44
Epigenetic changes play 2 distinct roles in the molecular progression of cancer. Progressive methylation and silencing of a subset of genes first occurs in normal tissues, as a function of age, time-dependent events, predisposing these normal cells to neoplastic transformation. Later in disease progression, epigenetic alterations play an important role in a subset of tumors, resulting in epigenetic instability. The methylation changes involve promoters (hypermethylation of tumor suppressor gene or hypomethylation of oncogenes), noncoding repetitive DNA sequences,45 and endogenous virus genomes or retroviral transposable elements, which become hypomethylated tissue-specifically during aging in C57BL mice.46 There is compelling evidence that DNA methylation varies with aging and between tissues, individuals, and disease conditions in humans and various animals.47 There is considerable variation in the degree of methylation among individuals of comparable ages, and age-related gene methylation changes occur in a tissue-specific fashion.48 Global DNA hypomethylation has also been demonstrated for age-related diseases such as cancer. The risk of developing FL increases with age. The pathogenesis of FL involves the transformation of a germinal center-derived B cell with a t(14;18) chromosomal translocation, resulting in a cell survival advantage through antiapoptotic mechanisms. Previous studies suggest that hypomethylation of the BCL-2 gene may be associated with this translocation event.49 Genomic DNA methylation decreases in response to moderate folate depletion in elderly women.50 Interestingly, genetic variations in genes involved in the folate-methionine pathways can further influence occurrence of these alterations. The number of hypermethylated CpG islands in tumor tissue from cancer patients correlates with inheritance of the MTR 2756A allele, suggesting that the germ-line differences in this gene may determine predisposition to cancers characterized by large numbers of DNA methylation sites.39 Studies in colorectal cancer support this theory,51,52 and our results and those of Lincz29 suggest that a similar mechanism of carcinogenesis may apply to FL.
Moreover, in multifactorial diseases, gene-nutrient interactions may also be determinant. In studies of lymphocyte extracts, individuals homozygous for the MTHFR 1298C allele displayed high enzyme activity and high plasma homocysteine concentrations.8,53 However, the fasting homocsyteine concentrations in mutant individuals are dependent upon folate status; individuals homozygous for this mutation were hyperhomocysteinemic only when folate levels were at the lower end of the normal range.54 Recent data suggest that the protective effect of folate may be mediated by enzyme stabilization.55 Interestingly, maternal folate supplementation in pregnancy was shown to protect against ALL in childhood.13,14 However, a puzzling gene-nutrient interaction between the TYMS VNTR and folate intake was recently reported.33 High folate intake (more than 440 μg/d [highest tertile] versus 440 μg/d or less) and vitamin B12 can have strikingly opposed effects depending on the TYMS genotype. Because of the patients' anonymity, it was not possible to trace individual cases to test for a relationship with folate and homocysteine status.
In conclusion, there is a strong association between aberrations in folate-methionine metabolism pathways (pathways that concern DNA synthesis and DNA methylation) and risk of FL. Low or inadequate intakes of folic acid, choline, methionine, and the folate cofactors, vitamins B2,B6, and B12, may exacerbate the risk of FL in individuals with “high-risk” genotypes. A combination of unfavorable genotypes, diet, and vitamin B status may be important in susceptibility to FL. Further research in this area may help establish how dietary and nutritional modifications may alter the risk of FL in susceptible individuals. Although there may be dietary or lifestyle differences between populations that could influence the effects of these susceptibility genotypes, reproducing these findings (or other genes belonging to the same pathway) in other ethnic groups is necessary.
Prepublished online as Blood First Edition Paper, January 12, 2006; DOI 10.1182/blood-2005-04-1567.
Supported in part by the Association pour la Recherche sur le Cancer (ARC) and a grant from the Ligue Nationale Contre le Cancer (LNCC) (S.N.).
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank the staff of the Necker-Enfants Malades Hospital and Lyon Sud Hospital for their help with the recruitment of LF patients and data collection.