Abstract
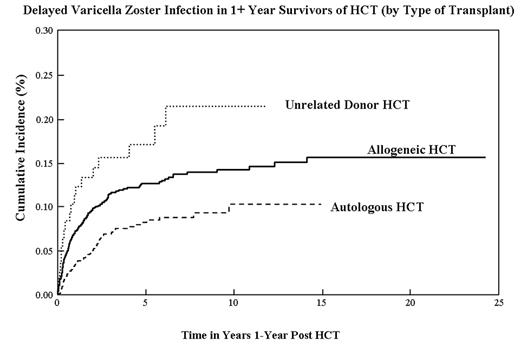
Patients undergoing HCT are at an increased risk of developing primary and reactivated VZV infection, with the majority of reactivations occurring within the first year post-HCT. Short term use of acyclovir as prophylaxis has been shown to be effective in reducing VZV risk, however prolonged use of acyclovir as prophylaxis is controversial, and the long term incidence of delayed VZV infection, and hence the recommended duration of antiviral prophylaxis is not clear. To assess the incidence and risk factors associated with delayed VZV infection (occurring one or more years after HCT), we conducted a retrospective chart review of 1578 consecutive patients undergoing HCT at City of Hope Cancer Center between 1976 and 1998, and surviving one or more years after HCT. Diagnosis of VZV was based on the clinic note dictated by the physician, with validation using appropriate laboratory tests in those individuals diagnosed with VZV. Information on pre-transplant therapeutic exposures and post-transplant health complications was obtained via medical record abstraction. The median age at HCT was 35 years (range, 0.6–71.5), median length of follow-up 6.4 years, and the cohort included 934 males (59.2%). In total, 178 patients (11.3%) developed VZV infection after surviving at least one year after HCT (19 patients (1.2%) had primary VZV (chickenpox), 138 patients (8.7%) localized herpes zoster, and 21 patients (1.3%) disseminated herpes zoster). The overall cumulative incidence was 13.9% (95% Confidence Interval [CI], 11.6–16.2%) at 15 years from HCT for the first reported VZV infection developing one or more years after HCT. (autologous HCT: 10.2% [7.2–13.3%] at 10 years); allogeneic sibling donor HCT survivors: 14.2% [11.6–16.8%]; unrelated donor HCT: 21.5% [12.3–30.7%]). Multivariate analysis of the allogeneic transplant cohort showed that prophylaxis/treatment of GvHD with prednisone (Relative risk (RR), 2.14; 95% CI, 1.27 to 3.61) and Mycophenolate Mofetil (RR, 1.93; 95% CI, 1.08 to 3.45) were associated with increased risk. No risk factors were identified for the development of VZV among autologous HCT recipients by multivariate analysis. VZV infection is a frequent and significant source of morbidity after HCT (bacterial superinfection, scarring, post-herpetic neuralgia), and can be potentially fatal if disseminated. This study describes the magnitude of risk of delayed VZV infection in autologous and allogeneic HCT recipients and identifies the use of immunosuppressive agents such as Prednisone and Mycophenolate Mofetil as risk factors, suggesting the possible use of acyclovir as prophylaxis during prolonged periods of immune suppression.
Incidence of Delayed Varicella Zoster in 1+ Year Survivors of HCT
Incidence of Delayed Varicella Zoster in 1+ Year Survivors of HCT
Delayed Varicella Zoster Infection in 1+ Year Survivors of HCT (by Type of Transplant)
Delayed Varicella Zoster Infection in 1+ Year Survivors of HCT (by Type of Transplant)
Disclosure: No relevant conflicts of interest to declare.
Author notes
Corresponding author