Abstract
We present results of 2 similarly designed but separate phase 2 studies involving single-agent lenalidomide (CC-5013, Revlimid) in a total of 68 patients with symptomatic myelofibrosis with myeloid metaplasia (MMM). Protocol treatment consisted of oral lenalidomide at 10 mg/d (5 mg/d if baseline platelet count < 100 × 109/L) for 3 to 4 months with a plan to continue treatment for either 3 or 24 additional months, in case of response. Overall response rates were 22% for anemia, 33% for splenomegaly, and 50% for thrombocytopenia. Response in anemia was deemed impressive in 8 patients whose hemoglobin level normalized from a baseline of either transfusion dependency or hemoglobin level lower than 100 g/L. Additional treatment effects in these patients included resolution of leukoerythroblastosis (4 patients), a decrease in medullary fibrosis and angiogenesis (2 patients), and del(5)(q13q33) cytogenetic remission accompanied by a reduction in JAK2V617F mutation burden (1 patient). Grade 3 or 4 adverse events included neutropenia (31%) and thrombocytopenia (19%). We conclude that lenalidomide engenders an intriguing treatment activity in a subset of patients with MMM that includes an unprecedented effect on peripheral blood and bone marrow abnormalities.
Introduction
Myelofibrosis with myeloid metaplasia (MMM) is a clonal stem-cell disorder that is characterized by intense bone marrow stromal reaction including collagen fibrosis, osteosclerosis, and angiogenesis.1 The molecular pathogenesis of MMM has not been fully characterized despite the recent discovery of an activating JAK2 mutation (JAK2V617F) that is found not only in approximately half of the patients with MMM but also in the majority of those with either polycythemia vera or essential thrombocythemia.2 Other nonspecific genetic markers in MMM include deletions of the long arms of chromosomes 13 and 20 and occasionally that of chromosome 5.3 Clinical phenotype includes progressive anemia, marked splenomegaly, extramedullary hematopoiesis, and a leukoerythroblastic blood smear. Average life expectancy is estimated to be 5 to 7 years but exceeds 10 years in young patients with good prognostic features.4 However, quality of life is often compromised by frequent red blood cell transfusions as well as a markedly enlarged spleen that is usually accompanied by both mechanical discomfort and profound constitutional symptoms.
Conventional drug therapy in MMM has not been shown to improve survival and is used for palliative purposes only. In this regard, androgen preparations, corticosteroids, and erythropoietin are often used as first-line therapy for alleviation of anemia.1 Symptomatic splenomegaly is initially treated with hydroxyurea and subsequently with splenectomy.5 Involved field radiation therapy is most effective for nonhepatosplenic extramedullary hematopoiesis6 but has limited value in controlling symptomatic enlargement of the spleen and liver.7,8 Treatment with an allogeneic hematopoietic stem cell transplant, either myeloablative9 or reduced intensity conditioning,10 is directed at eradicating the mutant MMM clone. However, this particular treatment modality is risky in terms of both mortality and morbidity and may not be applicable to most patients. Therefore, novel therapeutic approaches are urgently needed.
There is increasing evidence that bone marrow fibrosis and angiogenesis in MMM are mediated by clonal cell–derived cytokines including transforming growth factor-β (TGF-β),11 platelet-derived growth factor (PDGF),12 basic fibroblast growth factor (bFGF),13 and tumor necrosis factor-α (TNF-α).14 Because of the potent antiangiogenic15 as well as cytokine modulating16 activity of thalidomide, we had previously piloted the specific drug in MMM and subsequently showed a clinically relevant benefit in terms of both anemia and splenomegaly with the respective response rates of 20% and 25%.17 Encouraged by this experience, we explored the clinical activity of the more potent thalidomide analog, lenalidomide (CC-5013; Revlimid),18 in 68 symptomatic patients with MMM who were accrued to 2 separate phase 2 studies at the Mayo Clinic (n = 27) and M. D. Anderson Cancer Center (n = 41).
Patients, materials, and methods
This paper summarizes the results of 2 separate phase 2 studies involving single-agent lenalidomide therapy in patients with MMM. Approval was obtained from the Mayo Clinic and the M. D. Anderson Cancer Center institutional review boards for these studies. Informed consent was obtained in accordance with the Declaration of Helsinki. Protocol entry criteria for both centers are outlined in Table 1. Conventional criteria were used for the diagnosis of MMM including all subtypes: agnogenic (AMM), postpolycythemic (PPMM), and postthrombocythemic (PTMM) myeloid metaplasia.19 Patients with acute myelofibrosis or myelodysplastic syndrome with myelofibrosis were not eligible for participation in the current study. Baseline bone marrow histology and cytogenetic studies were performed in all study patients from both treatment centers. In addition, pretreatment (all patients) and posttreatment (major anemia responders) bone marrow microvessel density assessment and JAK2V617F mutation analysis were performed in patients accrued to the Mayo Clinic study. Pretreatment JAK2V617F mutation analysis was performed in 35 patients in the M. D. Anderson Cancer Center study. Previously published methods were used to grade bone marrow reticulin fibrosis and microvessel density,20,21 perform karyotype and fluorescent in situ hybridization (FISH) analysis,22 and screen for JAK2V617F mutation.23,24 Concurrent therapy with other agents was not allowed in the current study. Response criteria used in the current study are outlined as a footnote accompanying Table 2. The National Cancer Institute Common Terminology Criteria for Adverse Events (version 3.0) were used to assess drug toxicity.25 In addition to the combined presentation of overall response information, each one of the 2 phase 2 studies was analyzed separately for both response and toxicity data. Where appropriate, statistical analysis was performed by using Stat view software, version 5.01 (SAS, Cary, NC).
Results
Sixty-eight patients with MMM were enrolled in 2 similarly designed but separate phase 2 studies at the Mayo Clinic (n = 27) and M. D. Anderson Cancer Center (n = 41). Treatment protocols consisted of single-agent oral lenalidomide according to the dose and schedule outlined in Table 1. Baseline clinical and laboratory characteristics of the study population are outlined in Table 3. Response and drug toxicity data from both treatment centers are summarized in Tables 2 and 4, respectively. Table 5 provides further pretreatment and posttreatment information on patients achieving major anemia response.
Study 1, Mayo Clinic
Patients. Twenty-seven patients were accrued between March 5, 2004, and June 15, 2005. Twenty-five (93%) of the 27 patients received previous treatment, which included thalidomide treatment in 8 (30%). Pretreatment hemoglobin level was at least 100 g/L in all instances, including 21 patients who were red blood cell transfusion dependent at study entry. Protocol treatment eligibility criteria included adequate renal and liver function, a platelet count of at least 100 × 109/L, and an absolute neutrophil count of at least 1 × 109/L (Table 1). Other baseline laboratory findings are detailed in Table 3. Cytogenetic abnormalities were detected in 13 (48%) patients. JAK2V617F mutation analysis was performed in 25 patients and revealed a homozygous, heterozygous, and wild-type pattern, by sequencing, in 4, 10, and 11 patients, respectively. The median grades (range) of reticulin fibrosis, microvessel density, and osteosclerosis for all 27 study patients were 4 (1-4), 3 (1-4), and 2 (0-3), respectively.
Treatment details and adverse events. All 27 patients were started on a daily dose of 10 mg/d. Two patients received treatment for fewer than 2 weeks because of cutaneous adverse events. Other drug side effects (Table 4) and disease progression were responsible for an additional 11 patients not completing the first 3 cycles of treatment. Fourteen (52%) patients received 3 to 6 cycles of treatment, depending primarily on the absence or presence of response to the first 3 cycles of treatment, respectively (Table 1). In addition to the events listed in Table 4, 3 patients (one with PTMM and 2 with AMM) experienced marked thrombocytosis (peak platelet count 727-1598 × 109/L), and 2 other patients each displayed erythrocytosis (hemoglobin level peak at 19.1 g/dL in a patient with PPMM) or biopsy-proven disseminated extramedullary hematopoiesis (1 patient with AMM), all temporally associated with the study drug. Among the 5 patients who experienced drug-associated dyspnea, pulmonary hypertension was documented in 2 patients. Most adverse events improved upon drug withdrawal, and none were directly connected to patient demise. To date, 8 deaths have been reported, all occurring after discontinuation of protocol therapy, and most were attributed to progressive disease: 2 patients died of acute leukemia approximately 14 and 60 weeks from last day of protocol treatment, 4 patients died of progressive disease without leukemic transformation approximately 3, 4, 24, and 36 weeks from protocol drug discontinuation, 1 patient died of congestive heart failure and renal insufficiency 3 weeks from drug discontinuation, and 1 patient died of sepsis and renal insufficiency 24 weeks from drug discontinuation. In addition, one of the patients who died with progressive disease also experienced sepsis and acute respiratory distress syndrome at the time of death.
Response to lenalidomide therapy. The median posttreatment follow-up at the time of this writing was 19 months (range, 6-20 months), and all patients either have completed or discontinued protocol drug therapy. Individual response rates in anemia, splenomegaly, hypercatabolic symptoms, and serum lactate dehydrogenase (LDH) level are outlined in Table 2. Overall, 10 (37%) of the 27 study patients responded in terms of either anemia or splenomegaly. These included 6 (22%) patients who either normalized their hemoglobin level (4 patients) or became red blood cell transfusion independent (2 patients). The remaining 4 patients displayed a minor spleen response, without an associated improvement in hemoglobin level, which lasted for 1 to 3 months. Remission in the 2 patients with minor anemia response lasted for at least 6 months each before disease progression off therapy.
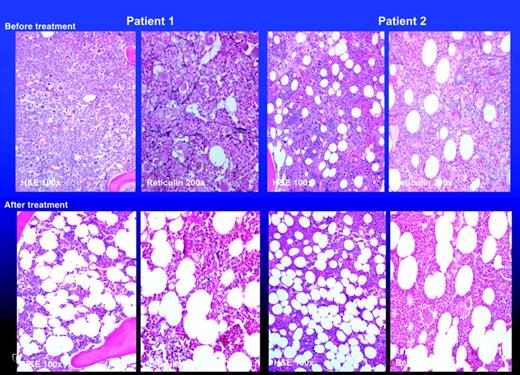
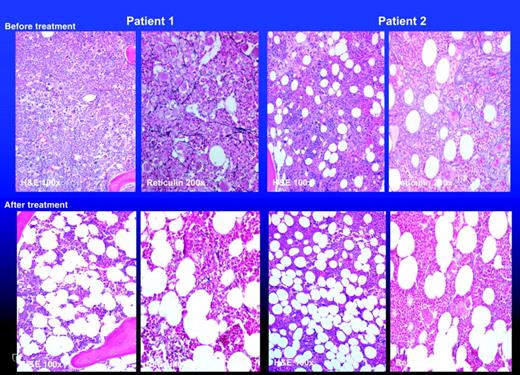
All 4 patients with a major response in anemia (ie, normalization of hemoglobin level) displayed resolution of peripheral-blood leukoerythroblastosis as well as normalization of serum LDH level (Table 5; patients 1, 2, 3, and 4). In addition, 2 of the 4 patients experienced a reduction in bone marrow fibrosis (Figure 1) and angiogenesis (Table 5; patients 1 and 2). The first of these 2 patients (Table 5; patient 1) with PPMM displayed a baseline del(5)(q13q33) cytogenetic abnormality as well as a heterozygous JAK2V617F mutation. The cytogenetic abnormality became undetectable at 6 months of protocol treatment. The disappearance of del(5q) was confirmed by FISH using probes for 5p15.2 (D5S23, D5S721) and 5q31 (EGR1) with documentation of treatment-associated reduction in the percentage of abnormal nuclei from 78% to 0% (normal, < 6%). Interestingly, the change in del(5q) status in the particular patient was accompanied by a reduction in JAK2V617F mutation burden (data not shown). The patient remains in remission at 3+ months after drug discontinuation. The second patient with bone marrow histologic response (Table 5; patient 2) had AMM with normal baseline cytogenetic findings and a heterozygous JAK2V617F mutation that was not affected by lenalidomide therapy despite continued remission at 5+ months after discontinuing protocol therapy that consisted of 3 cycles of lenalidomide. Similarly, JAK2V617F mutational status was not affected by treatment in the third major anemia responder who had a homozygous mutation (Table 5; patient 4). This patient and the fourth major anemia responder (Table 5; patient 3) now have relapsed off therapy after 2 and 6 months of treatment discontinuation.
Bone marrow histology (hematoxylin-eosin as well as reticulin stain) before and after treatment with lenalidomide in 2 patients with myelofibrosis with myeloid metaplasia who achieved major anemia response as well as resolution of peripheral-blood leukoerythroblastosis. The 2 patients represent patients 1 and 2 from Table 5. Images were obtained by using a Leeds Olympus AX70 microscope (Olympus, Minneapolis, MN) equipped with a 160×/0.4 objective lens and a Nikon DXM1200 digital camera (Nikon, Melville, NY); Nikon ACT-1 software version 2.62 was used to acquire digital images. No further image processing was conducted.
Bone marrow histology (hematoxylin-eosin as well as reticulin stain) before and after treatment with lenalidomide in 2 patients with myelofibrosis with myeloid metaplasia who achieved major anemia response as well as resolution of peripheral-blood leukoerythroblastosis. The 2 patients represent patients 1 and 2 from Table 5. Images were obtained by using a Leeds Olympus AX70 microscope (Olympus, Minneapolis, MN) equipped with a 160×/0.4 objective lens and a Nikon DXM1200 digital camera (Nikon, Melville, NY); Nikon ACT-1 software version 2.62 was used to acquire digital images. No further image processing was conducted.
Interestingly, 3 of the 4 major anemia responders had antecedent polycythemia vera or essential thrombocythemia, as compared to 3 of 22 without such a response (P = .01). Similarly, the 4 treatment responders displayed significantly less bone marrow fibrosis (P = .002). On the other hand, neither JAK2 mutational status nor degree of bone marrow angiogenesis appeared to affect lenalidomide-induced major anemia response (P = NS). Because of the now-recognized connection between lenalidomide treatment response and the presence of del(5q) in myelodysplastic syndrome (MDS),26 we employed additional FISH analysis in all 4 major anemia responders but did not identify a cytogenetically occult del(5q) abnormality. Finally, none of the 4 major anemia responders, but both patients with minor anemia response, were previously exposed to thalidomide therapy.
Study 2, M. D. Anderson Cancer Center
Patients. Forty-one patients were accrued between July 21, 2004, and July 8, 2005. Thirty-six (88%) of the 41 patients were previously treated and 13 (32%) had previous exposure to thalidomide. It is to be noted that the study at M. D. Anderson Cancer Center (MDACC) included patients with hemoglobin levels higher than 100 g/L if they were otherwise symptomatic from either splenomegaly or thrombocytopenia. Accordingly, pretreatment hemoglobin level was no more than 100 g/L in only 19 (46%) of the 41 study patients, including 13 (32%) who were red blood cell transfusion dependent at study entry. Similarly, protocol treatment eligibility criteria at MDACC included a platelet count of at least 30 × 109/L (Table 1). Other baseline laboratory findings are detailed in Table 3. Cytogenetic abnormalities were detected in 17 (42%) patients. Bone marrow angiogenesis was not evaluated in the study from MDACC. Thirty-five patients have been assessed for JAK2V617F mutation, and it was identified in 18 (51%) of them.
Treatment details and adverse events. The baseline platelet count dictated the starting dose for lenalidomide at MDACC; 10 mg/d if platelet count higher than 100 × 109/L, and 5 mg/d otherwise. Twenty-five (61%) and 12 (29%) patients received more than 3 or 6 cycles of therapy, respectively, depending on both drug tolerance and response assessment after 3 and 6 months of therapy (Table 1). Neutropenia (32%) and thrombocytopenia (27%) were the major grade 3 or 4 drug side effects. On the other hand, severe nonhematologic toxicity was infrequently seen (Table 4). Six patients (3 with PTMM, 2 with AMM, and 1 with PPMM) experienced drug-induced thrombocytosis (peak platelet count 933-1631 × 109/L). Both these and other adverse events improved upon drug withdrawal. To date, 5 deaths have been reported, and none were directly attributed to drug side effects. One patient died while on therapy (week 7) from non-neutropenic sepsis, whereas the other 4 had been off therapy for 5, 15, 31, and 33 weeks, respectively, at time of death. Causes of death included cerebrovascular accident, subdural hematoma, progression into acute leukemia, and complications from allogeneic stem cell transplantation.
Response to lenalidomide therapy. The median posttreatment follow-up at the time of this writing was 5 months (range, 1-14). To date, 21 (51%) patients remain on drug therapy. Response rates in anemia, splenomegaly, thrombocytopenia, and serum LDH level are outlined in Table 2. Ten (24%) of the 41 study patients responded in terms of anemia (2 patients), splenomegaly (6 patients), or both (2 patients). Among these, 4 (21%) of the 19 patients with a baseline hemoglobin level lower than 100 g/L, including 1 who was transfusion dependent, attained a major anemia response by normalizing their hemoglobin level (Table 5; patients 5, 6, 7, and 8). Of these 4 patients, 3 were negative for JAK2V617F (Table 5; patients 6, 7, and 8). All 4 had de novo MMM without antecedent history of either polycythemia vera (PV) or essential thrombocytopenia (ET). The spleen was palpably enlarged in 2 of these 4 patients before treatment and became impalpable in one patient (Table 5; patient 6) and decreased in size from 10 cm to 2 cm in the second patient (Table 5; patient 5) as a result of treatment. Only 1 of the 4 major anemia responders had a baseline cytogenetic abnormality (trisomy 9) that was not affected by treatment (Table 5; 5). To date, 3 of the 4 anemia responders remain in remission for 6 to 36 weeks on active therapy (Table 5; patients 5, 6, and 7). The fourth patient relapsed off therapy (Table 5; patient 8). Of the 8 patients with spleen response, 6 did not qualify for anemia response because of either a baseline hemoglobin level higher than 100 g/L or lack of a concomitant response in anemia. Of these 6 patients, so far 2 have relapsed while receiving protocol treatment. A platelet response was observed in 6 of 12 patients with thrombocytopenia, with a median platelet increase of 60 × 109/L over pretreatment values. With the limited available data with JAK2V617F, 4 of the 6 patients with JAK2V617F mutation responded.
Discussion
Among many drugs that have recently been investigated in MMM, thalidomide has displayed the best therapeutic activity in terms of anemia.27 In one of the original studies involving single-agent thalidomide therapy in MMM (n = 15), oral thalidomide at an average dose of 200 mg/d was poorly tolerated but produced anemia and spleen response rates of approximately 20% and 25%, respectively.17 A higher proportion of patients experienced an increase in platelet count. Subsequently, both lower drug doses (50 mg/d)28 and combination of low-dose thalidomide (50 mg/d) and prednisone (a tapering schedule starting at 30 mg/d)29 were shown to be better tolerated as well as more effective in terms of anemia response. This was the primary rationale for the current phase 2 studies in our respective institutions that evaluated the therapeutic activity of lenalidomide, a more potent as well as less neurotoxic thalidomide analog, in MMM.
Lenalidomide is an IMiD, a proprietary class of thalidomide analogs that have a broad cytokine modulatory activity and inhibit TNF-α, IL-1β, IL-6, and IL-12 while they up-regulate IL-2 and interferon-γ production by T helper-1 cells and IL-5 and IL-10 production by T helper-2 cells.30 The IMiDs co-stimulate T cells and are antiangiogenic. Depending on the assay used, lenalidomide is estimated to be 50-fold to 2000-fold more potent than thalidomide.31,32 Clinical treatment trials with single-agent lenalidomide have been reported in both nonhematologic33,34 and hematologic26,35 malignancies, with more promising results in the latter, especially in multiple myeloma and MDS. MDS is a clonal stem-cell disease that displays some similarities with MMM in terms of both disease biology and clinical features.36 In a recently published study,26 43 patients with primarily low-risk MDS and symptomatic anemia were treated with either 25-mg or 10-mg daily doses of lenalidomide continuously or for 21 of every 28 days (ie, syncopated). After 16 weeks of protocol treatment, response was documented in 56% of the patients, including 20 patients who became transfusion independent. In addition, 75% of patients with del(5q) featured a remarkable complete hematologic and cytogenetic response. As was the case in the current study, neutropenia and thrombocytopenia were the most common adverse events, with grade 3 or 4 toxicities that ranged in frequency from 59% (10 mg/d syncopated) to 77% (25 mg/d) and 53% (10 mg/d syncopated) to 54% (25 mg/d), respectively. Additional experience from a larger, multicenter phase 2 study led to the Food and Drug Administration approval on December 27, 2005 (under restricted distribution) of lenalidomide for transfusion-requiring low or intermediate-1 risk MDS associated with del(5q).
The current study clearly establishes lenalidomide as a viable treatment option in MMM. We were most impressed by the normalization of hemoglobin in 8 (17%) of 46 patients with a baseline hemoglobin level of below 100 g/L (3 were transfusion dependent before treatment). In particular, we were intrigued by the quality of response in 4 of these patients who also displayed resolution of leukoerythroblastosis (a hallmark of MMM). In addition, 2 of the 4 patients experienced a posttreatment reduction in bone marrow fibrosis and angiogenesis, and 1 with del(5q) clone attained a complete cytogenetic remission that was confirmed by a more sensitive FISH technique. The particular patient remained JAK2V617F positive, however, despite a reduction in mutation burden (data not shown). These observations suggest that del(5q), in this instance, might be a JAK2V617F subclone and that lenalidomide's peculiar effect on del(5q)-associated clonal myelopoiesis might be independent of the underlying histopathology. At the same time, it is evident that the drug might be active even in the absence of del(5q), as has been noted before with MDS.26 On the other hand, the fact that 3 of the 4 major anemia responders who displayed resolution of myelophthisis had secondary myelofibrosis did not go unnoticed, but the numbers were too small to draw any conclusions.
Of the 8 patients with major anemia response, 4 were accrued by the Mayo Clinic study and accordingly received a maximum of 6 months' therapy. To date, 2 of these 4 patients remain in remission after 3 and 5 months of treatment discontinuation, whereas the other 2 relapsed off therapy. Similarly, 3 of 4 major anemia responders from the M. D. Anderson clinical trial who continue to receive active therapy have not relapsed after 6 to 36 weeks, whereas the fourth patient has relapsed off therapy. Therefore, continued treatment might be necessary to sustain lenalidomide-induced remissions in MMM. Furthermore, the observation of a substantial reduction in serum LDH in more than two thirds of treated patients, regardless of documented clinical response, is intriguing, and its relevance within the context of a longer treatment schedule remains to be determined.
At the present time, the mechanism of hematological benefit from drug therapy in MMM is no more lucid for lenalidomide than it is for thalidomide. Regardless, as has been the case in multiple myeloma,37 combining lenalidomide with corticosteroids carries the prospect of better response rates, and such a possibility in MMM is currently being evaluated by an Eastern Cooperative Oncology Group–coordinated study. In the meantime, it is important to recognize the nontrivial occurrence of severe drug-induced myelosuppression that dictates close monitoring of complete blood count during treatment. On the other hand, the current study did not disclose excess risk of thromboembolic events (only one case among all 68 study patients), an issue of potential relevance in patients with multiple myeloma receiving lenalidomide- or thalidomide-based combination chemotherapy.38
Prepublished online as Blood First Edition Paper, April 11, 2006; DOI 10.1182/blood-2006-02-004572.
Supported by research funding from Celgene, Summit, NJ.
J.B.Z. and C.B. are employed by Celgene Corporation (Summit, NJ), whose product (lenalidomide) was studied in the present work.
A.T. and J.C. contributed equally to this study.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.