Abstract
We present the results of a phase 2 study using thalidomide, dexamethasone, and pegylated liposomal doxorubicin (ThaDD) in the treatment of 50 patients older than 65 years with newly diagnosed multiple myeloma. Thalidomide 100 mg was administered orally at bedtime continuously, dexamethasone 40 mg was administered orally on days 1 to 4 and 9 to 12, and pegylated liposomal doxorubicin 40 mg/m2 was administered intravenously on day 1 over the 28-day cycle. Response was assessed according to the EBMT criteria. Seventeen (34%) patients achieved CR, 7 (14%) nCR, 5 (10%) VGPR, 15 (30%) PR, and 5 (10%) MR, resulting in an ORR of 98%. Only 1 patient (2%) presented progressive disease. Time to progression (TTP), event-free survival (EFS), and overall survival (OS) projected at 3 years were 60%, 57%, and 74%, respectively, and these parameters were significantly higher in those patients achieving a response of at least VGPR versus those who did not. Grade 3 and 4 nonhematologic adverse events were constipation (10%), fatigue (6%), tremors (4%), mucositis (4%), and palmar-plantar erythrodysesthesia (2%). Grade 3 and 4 neutropenia occurred in 12% of patients. Grade 3 and 4 infections and thromboembolic accidents were observed in 22% and 14% of patients, respectively. In the treatment of elderly patients with newly diagnosed multiple myeloma, ThaDD is a very effective regimen with manageable toxicity.
Introduction
Although almost two thirds of patients with multiple myeloma (MM) are older than 65 years,1 no standard effective therapies have been yet identified for this population. The melphalan-prednisone combination (MP) is relatively well tolerated but does not provide satisfactory results. High-dose therapy followed by stem cell autotransplantation is not recommended in every single case, or it may present an unacceptable toxicity in patients older than 70 years.2 Intermediate melphalan doses (140 or 100 mg/m2), even if suitable for elderly patients, offer less satisfactory results than in younger patients, with a nonnegligible rate of morbidity and mortality.2,3
Targeted therapy has opened new horizons for the treatment of MM.4 These new drugs target not only particular intracellular pathways but also interfere with the exchanges occurring between plasma cells and bone marrow microenvironment, exchanges that are responsible for drug resistance and capable of preventing apoptosis. Thalidomide is actually the drug that has been better investigated when compared with new therapeutic agents. Administered as a single agent,5 in combination with dexamethasone,6-9 or with conventional chemotherapy,10-13 it has been found to offer very promising results in untreated patients with MM. In particular, the best results were observed when thalidomide was combined with melphalan13 or with antracyclines,10-12 although the toxicity of these combinations was severe and withdrawals from study protocols were frequent also in younger patients. However, it is yet unclear what is the better agent or agents or regimen or regimens to combine with thalidomide-dexamethasone to improve their efficacy minimizing the toxicity, especially in older patients.
Assuming that elderly patients often present comorbidities, poor performance status, and little bone marrow backup, we designed a specific regimen for patients older than 65 years. It included low-dose thalidomide to reduce dose-dependent side effects; pegylated-liposomal doxorubicin, showing promising anti-myeloma activity with both lower cardiotoxicity and myelotoxicity compared with those reported with conventional form; and high-dose pulsed dexamethasone, having a pivotal role in the treatment of MM. Here, we present the results of a phase 2, multicenter study using the above regimen (ThaDD) in patients older than 65 years with MM.
Patients, materials, and methods
Study design and patients
This is a prospective, multicenter, phase 2 study on a combined treatment with pegylated liposomal doxorubicin, dexamethasone, and thalidomide (ThaDD) in patients with newly diagnosed MM. From March 2003 to March 2005, 50 consecutive patients from 9 institutions were enrolled. Age; performance status (PS); and cardiopulmonary, liver, and renal functions did not prevent the inclusion of patients, but we excluded patients affected by other neoplasms, drug-resistant infections, preexisting grade 2 or greater peripheral neuropathy, and presenting psychiatric disorders. The study was approved by all local ethics committees, and all patients signed a written informed consent before entering the study.
Baseline evaluation included medical history and physical examination, blood count, serum protein electrophoresis, 24-hour urine Bence Jones protein determination and electrophoresis, liver and renal function assessment, β2-microglobulin, C-reactive protein, x-rays, bone marrow aspiration or biopsy, and fluorescence in situ hybridization (FISH) investigation. Unfavorable cytogenetics was defined as chromosome 13 abnormalities, t(4;14), t(14;16), and complex karyotypes.
All patients receiving at least one cycle of chemotherapy were considered evaluable for the assessment of both toxicity and response. Toxicity, as per the National Cancer Institute criteria, was assessed on a weekly basis during the first 28-day cycle and monthly in the course of treatment afterward with medical interview, physical examination, and laboratory tests.
Response to treatment was rated according to the EBMT criteria.14 Furthermore, we included 2 other categories: near-complete remission (nCR), defined as no detectable monoclonal protein by electrophoresis with positive immunofixation, and very good partial remission (VGPR), defined as a greater than 90% reduction in serum paraprotein. To evaluate response, serum or urine electrophoresis or both were performed once a month and bone marrow aspirate after 3 cycles of therapy. A complete restaging was performed at the completion of chemotherapy. Subsequently, patients were followed with history, physical examination, and laboratory tests every 3 months, bone marrow aspirate every 6 months, and skeletal X-rays every year.
Treatment
Patients received intravenous pegylated liposomal doxorubicin (Caelyx) 40 mg/m2 diluted in 250 mL 5% dextrose solution over 1 hour on day 1 every 28 days in day-hospital, dexamethasone 40 mg orally on days 1 through 4 and 9 through 12, and thalidomide 100 mg each evening continuously. Thalidomide was prepared in the Umberto I Hospital Pharmacy. Pegylated liposomal doxorubicin and dexamethasone were administered for 3 cycles, and those patients responding in a percentage of VGPR or greater were administered 2 additional cycles, whereas those achieving a response of PR or less were given 3 additional cycles. Patients showing progression were dropped. Supportive therapy included 1.25 mg/d warfarin, vitamin B6, zoledronic acid, erythropoietin, and hypoglycemic drugs or insulin if the blood glucose was higher than 9.99 mM (180 mg/dL). No antibacterial prophylaxis was initially given to patients. Because of the high incidence of respiratory infections, occurring after the first 28 cycles of chemotherapy, we administered 250 mg ciprofloxacin twice a day for all the remaining cycles.
If patients developed at least grade 3 neutropenia following pegylated liposomal doxorubicin infusion, granulocyte colony-stimulating factor was then administered for all subsequent cycles without reducing dosage. A 25% dose reduction and 2-week delay in the administration of pegylated liposomal doxorubicin were required when grade 4 mucositis and palmar-plantar erythrodysesthesia occurred. Drug discontinuation was mandatory in the event of grades 3 and 4 cardiotoxicity. Dexamethasone has to be reduced to 20 mg or discontinued in case of grade 2 or greater muscular toxicity. The onset of grade 3 or greater neurotoxicity was the only situation leading to thalidomide discontinuation, whereas the occurrence of other side effects, thromboembolic disease, and infectious complications did not.
Statistical methods
The study primary end points were response rate and toxicity. Secondary end points included time to progression (TTP), event-free survival (EFS), and overall survival (OS). Outcome was analyzed on a modified intent-to-treat basis.
It was assumed that the combination would induce a response rate (defined as a reduction by ≥ 50% of myeloma proteins) 20% higher than that reported with conventional MP regimen. Considering an α-value less than .05 and a β-value of 0.80, 43 patients have to be enrolled according to Simon 2-stage design.
Univariate analysis of factors affecting response was performed by chi-squared test for contingency table, whereas Cox proportional hazard model was applied to recognize factors affecting time-dependent variables. TTP, EFS, and OS were calculated from enrollment to disease progression or death resulting from progression, any event (except therapy interruption because of toxicity), and death, respectively. For the comparison of the TTP, EFS, and OS according to response (< VGPR versus ≥ VGPR), we performed a landmark analysis using as starting point the date scheduled for response confirmation (4-5 months after the start of first cycle). The curves were plotted according to the Kaplan-Meier method, and they were compared by log-rank test. A P value less than .05 was considered significant. All analyses were performed with SPSS software (SPSS Science, Chicago, IL).
Results
Patient characteristics
Fifty patients with untreated MM were enrolled in this study, and their characteristics at study entry are shown in Table 1. Note that 64% of patients were older than 70 years, PS was at least 2 in 20%, ISS was at least 2 in 74%, and β2-microglobulin level was at least 3.5 mg/L in 60% of patients. Moreover, 14% of patients presented impaired renal function and 7 (24%) of 29 patients with valuable FISH analysis showed unfavorable abnormalities.
Response to therapy
After 4 cycles of therapy, 17 (34%) of 50 patients achieved CR, 7 nCR (14%), 4 VGPR (8%), 14 PR (28%), and 7 MR (14%), resulting in a 98% ORR (Table 2). Only 1 patient (2%) showed signs of progressive disease. At the end of therapy, 1 patient achieved VGPR and 1 PR both from MR. The maximal response to treatment was reached after a median of 2 cycles (range, 1-5 cycles). During treatment 3 patients died, 2 of heart failure and 1 of multiple organ failure after the response was assessed.
All 7 patients with impaired renal function achieved an objective response (4 ≥ VGPR, 2 RP, 1 MR), and normal renal function was restored.
No single characteristic was significantly associated with quality of response (< VGPR versus ≥ VGPR).
Survival
After a median 18 months of follow-up (range, 6-36 months), 12 patients relapsed and 10 died (3 during treatment, 7 in follow-up). Seven patients (14%) underwent autotransplantation and were censored at the time of transplantation. Median number of CD34+ cells yielded was 8.3 × 106/kg (range, 4.8 × 106-12.6 × 106/kg). All patients engrafted rapidly after intermediate- or high-dose melphalan.
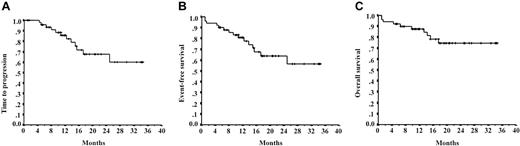
Median TTP, EFS, and OS were not reached, whereas TTP, EFS, and OS projected at 3 years were 60%, 57%, and 74%, respectively (Figure 1A-C).
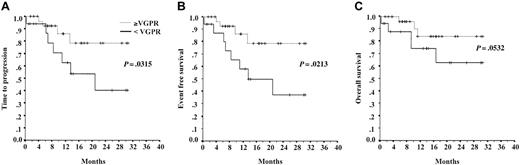
No single characteristic was significantly predictive of TTP, EFS, and OS except response to treatment. Landmark analysis demonstrated that patients achieving a response of at least VGPR had a significantly higher 3-year TTP (78% versus 40%; P = .031), EFS (78% versus 37%; P = .021), and OS (84% versus 61%; P = .053) (Figure 2A-C).
Survival times. Time to progression (A), event-free survival (B), and overall survival (C) of 50 patients treated with ThaDD regimen.
Survival times. Time to progression (A), event-free survival (B), and overall survival (C) of 50 patients treated with ThaDD regimen.
Compliance to therapy
Overall, we administered 206 cycles of ThaDD (median, 4 cycles; range, 1-6 cycles). Two patients (4%) refused to continue therapy, one because of the occurrence of pulmonary embolism and another for septic shock. In 1 patient pegylated liposomal doxorubicin dosage was reduced for the occurrence of severe mucositis, whereas 11 patients (22%) underwent the scheduled treatment with a few days' delay because of infection in 9 cases, severe neutropenia in 1 patient, and mucositis in another patient.
One patient discontinued dexamethasone because of muscle aches and severe asthenia, and 2 patients (4%) interrupted thalidomide treatment for the occurrence of grade 3 tremors, whereas 2 patients refused to continue thalidomide because of severe constipation.
Hematologic toxicity and infection
Neutropenia of any grade and grades 3 and 4 occurred in 42% and 12% of patients, respectively. Twenty-one patients (42%) experienced a febrile episode (10% of all courses), being of at least grade 3 in 22% of them (5% of courses). In the majority of cases (90%) fever occurred in nonneutropenic patients and following the first 3 cycles (90%). However, during the first 28 cycles (5 patients) administered without antibiotic prophylaxis we documented 7 infectious complications (25%), whereas in subsequent 178 courses, in which we administered ciprofloxacin 250 mg twice daily, only 14 new episodes of infections (7%) occurred. Lung infiltrates were identified in 7 episodes (14%). Eleven episodes were classified as fever of unknown origin, 1 patient developed neutropenic septic shock, and in the last 2 patients urinary infection and ocular abscess were documented. No patient experienced herpetic or other opportunistic infections, and none died of infections. Only one patient was dropped from the protocol because of infectious complications (septic shock).
Thrombocytopenia occurred in 12% of patients, but none of grade 3 or greater. Nearly all patients (95%) were administered erythropoietin to prevent severe anemia.
Nonhematologic toxicity
Nonhematologic toxicity is shown in Table 3. Most side effects were rated mild to moderate, but 18 patients (36%) experienced grades 3 and 4 adverse events. Severe side effects related to thalidomide were fatigue (6%), constipation (4%), and tremors (4%). Regarding toxicity by pegylated liposomal doxorubicin, 2 patients (4%) experienced grades 3 and 4 mucositis and 1 patient experienced grade 3 palmar-plantar erythrodysesthesia. Dexamethasone mainly caused slight muscle weakness, but 1 patient developed severe myopathy.
Survival times according to response. Landmark comparison of time to progression (A), event-free survival (B), and overall survival (C) in patients obtaining a response of at least VGPR (dotted lines) or less than VGPR (solid lines).
Survival times according to response. Landmark comparison of time to progression (A), event-free survival (B), and overall survival (C) in patients obtaining a response of at least VGPR (dotted lines) or less than VGPR (solid lines).
Venous thromboembolic events occurred in 7 patients (14%), but only 1 patient showed clinical evidence of pulmonary embolism. All events involved the femoral or popliteal veins.
Discussion
High-dose therapy (HDT) followed by autologous stem cell transplantation (ASCT) has improved the outcome of both young15 and elderly patients with multiple myeloma.2,3 However, nearly half of patients with MM are ineligible for this procedure because of old age or inadequate end-organ function or because they refuse transplantation. These patients have a poor short-term prognosis, whichever conventional therapy they receive. Therefore, the melphalan-prednisone combination remains the standard treatment for older patients with MM, although the results are entirely unsatisfactory.16 It is obvious that more effective alternative treatments are needed for elderly patients with MM. Thalidomide-dexamethasone is becoming the up-front regimen before HDT and ASCT.17 However, this combination administered to patients who are not candidates for autotransplantation led to results similar to those achieved with conventional chemotherapy.8 Better results can be obtained when chemotherapeutic agents are added to or administered before18 the thalidomide-dexamethasone combination.10-13 At present, it remains unclear which single or other chemotherapy regimen is the best one to be combined with thalidomide-dexamethasone to achieve a higher CR rate associated with an acceptable toxicity. Moreover, it is unknown whether the best quality of response obtained with these combinations does affect survival parameters of patients with MM.
We decided to explore a vincristine, adriamycin, dexamethasone (VAD)–like regimen in which vincristine was replaced by thalidomide, because the administration of both drugs has been considered conflicting in terms of neurotoxicity. Standard doxorubicin was replaced by a pegylated liposomal form, being less toxic and potentially more effective than the conventional agent because of its pharmacokinetics properties. Dexamethasone was given in adequate doses because it plays a key role in the treatment of MM.
With the present combination, 58% of patients showed a greater than 90% reduction in serum M protein level and 48% experienced its negativization (CR/nCR) with an excellent compliance to treatment. Better responses were achieved mainly within 3 months from therapy initiation; EFS and OS were, respectively, 65% and 70% at 3 years. It must be highlighted that patients who achieved high-quality responses had a significantly better TTP, EFS, and OS by landmark analysis. This means that a higher-quality response obtained with this protocol turns in better survival parameters.
Our results are clearly superior to those obtained with conventional chemotherapy in terms of both response rate and survival.19-21 Among studies assessing the efficacy of the thalidomide-based regimens in untreated elderly patients with MM, the only one that is comparable to ours in terms of median age, exclusion criteria, and administered thalidomide dose is Palumbo et al,13 who treated 129 patients with a combination of thalidomide, oral melphalan, and prednisone. With this regimen they observed combined CR and nCR in 28% of patients, near half the value that we obtained (48%). This difference may be explained either by low-dose melphalan and steroids used to reduce toxicity or to an actual superior antimyeloma activity of the pegylated liposomal doxorubicin–dexamethasone combination versus the melphalan-prednisone combination. Grades 3 and 4 hematologic, neurologic, and vascular toxicities were more frequent in melphalan, prednisone, and thalidomide (MPT) combination and, despite a higher incidence of grades 3 and 4 infections we observed, no patients developed opportunistic infections, even if no antiviral prophylaxis was administered. Actually the introduction of ciprofloxacin antibiotic prophylaxis led to a significant reduction of infections rate (< 10%). Moreover, no patients died of infectious complications.
Although no deaths were related to thromboembolic events and our incidence of deep vein thrombosis (DVT; 14%) is close to the lowest rates reported by other studies,10-13,18 it needs to be reduced. Even though the best DVT prophylaxis in patients receiving thalidomide-based regimens has not been established so far, retrospectively, we believe that fixed-dose warfarin might have been inadequate as DVT prophylaxis in our protocol. We think that in the future trials and in clinical practice more effective DVT prophylaxis than fixed-dose warfarin should be considered in patients treated with thalidomide and anthracyclines.
Other investigators have reported the results of chemotherapy combinations with thalidomide, dexamethasone, and pegylated liposomal doxorubicin, but, unlike us, they also administered vincristine. Almhanna et al,11 with 400 mg thalidomide daily, obtained at least an nCR response rate which was almost similar to ours, but the incidence of neurologic and vascular toxicities was much higher despite the median age of that study population (59 years) being lower than in our patient cohort (71.5 years).11 Moreover, in a recent study the same investigators reported that patients receiving full-dose vincristine in the doxorubicin, vincristine, and reduced-frequency dexamethasone with thalidomide (DVd-T) regimen showed a significantly worse PFS than those receiving the reduced-dose or stopping vincristine.22 Administering a combination similar to DVd-T but with a lower dose of thalidomide (200 mg daily) and dexamethasone, Zervas et al10 achieved only a 10% CR rate in a study population, including also younger patients. Schutt et al,12 using epirubicin, high-dose thalidomide, and low-dose dexamethasone, reported a 19% CR rate, but the frequency of neurologic toxicity and vascular and infectious complications was nearly prohibitive. Our observations and data from the cited studies suggest the following: the response to thalidomide combined with chemotherapy is not dose dependent; high-dose dexamethasone proves to be crucial; liposomal-pegylated doxorubicin seems more effective than both epirubicin and low-dose melphalan, and, if administered as a single agent without vincristine, offers excellent results with minor toxicity.
Furthermore elderly patients with MM have to be evaluated as to whether they will be suitable candidates for HDT. Actually, in patients aged 50 to 70 years treated with intermediate-dose melphalan (100 mg/m2) with ASCT, Palumbo et al3 obtained a 25% CR + nCR rate and 37% EFS at 3 years. Using a higher dose of melphalan (140-200 mg/m2) Badros et al2 achieved a 27% CR rate and a 20% EFS rate at 3 years after tandem transplantations performed in patients 70 years or older. Both the investigators reported acceptable toxicity, particularly in patients in which melphalan did not exceed 140 mg/m2. These results showed that high-dose therapy is feasible and effective also in elderly patients, implying that any regimen designed for patients older than 65 years should not preclude this procedure, and our combination allows this. Actually, in our study 7 patients considered eligible for HDT were successfully treated with mobilization and autotransplantation. However, we believe that it may be questionable to perform autotransplantation in older patients with MM, considering the results of the thalidomide, steroids, and chemotherapy combinations. Well-designed studies are warranted to address this issue.
Recently, new drugs such as lenalidomide and bortezomib have been introduced in the treatment of patients with MM. In a phase 1 and 2 study, Mateos at al23 used the combination bortezomib-melphalan-prednisone in 53 previously untreated elderly patients. They obtained a 39% CR/nCr rate despite a high frequency and seriousness of hematologic and neurologic toxicities as well as opportunistic infections.23 Lenalidomide was associated also with melphalan-prednisone in 24 patients older than 65 years. No CR/nCr rates have been achieved, and hematologic, dermatologic, and metabolic toxicities were nonnegligible.24
In conclusion, the ThaDD combination has been effective in the treatment of elderly patients with newly diagnosed MM. The toxicity was manageable also in older fragile patients, and complications such as infections and DVT can be prevented with adequate antibiotic and antithrombotic prophylaxes. Moreover, our combination allowed us to perform HDT as consolidation therapy. We think that ThaDD therapy has to be explored further in comparative studies to confirm our results.
Prepublished online as Blood First Edition Paper, June 8, 2006; DOI 10.1182/blood-2006-03-013086.
All the authors were involved in the accrual of patients, chart review, draft review, and manuscript approval. M. Marconi and M.O. were responsible for data collection; M.O., P.L., M. Marconi, and L.C. were involved in the conception, design, and data analysis of the study; and M.O. and L.C. were responsible for manuscript writing.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.
We thank all patients involved in the study and their families for their patience and cooperation, the day hospital nursing and medical staff for their precious cooperation, Dr Valentina Cola for providing galenic thalidomide, Dr Giancarlo Discepoli for providing cytogenetic analyses, and Dr Barbara Amoroso for the editing of the manuscript.