Abstract
Background: Relapse/progression after allogeneic hematopoietic cell transplantation (HCT) remains the major cause of treatment failure. In this study, the subsequent clinical outcome in a modern transplant setting was overviewed to improve decision-making.
Patients and immediate therapy: Between 2000 and 2006, 294 patients with leukemia/MDS received allogeneic HCT after myeloablative (n=145) or reduced-intensity (n=149) conditioning. Among them, 93 patients (32%) either relapsed or showed disease progression; the relapse rate was 40% for AML (57/144 patients), 18% for MDS (13/72), 14% for CML (5/35), and 42% for ALL (18/43). The median overall survival (OS) after relapse or progression was 167 days (range; 5 to 1456 days). Twenty-eight patients (30%) were elected to receive no interventions with curative intent other than withdrawal of immunosuppressant, less-intensive chemotherapy or DLI, mostly due to comorbidities or refractoriness of the disease, and all but 3 patients died with disease progression at a median of 61 days. Two other patients underwent immediate HCT without intervention due to graft failure. Among the remaining 63 patients (68%) who received therapeutic interventions including re-induction chemotherapy with or without DLI, 26 (41%) achieved subsequent complete remission (CR).
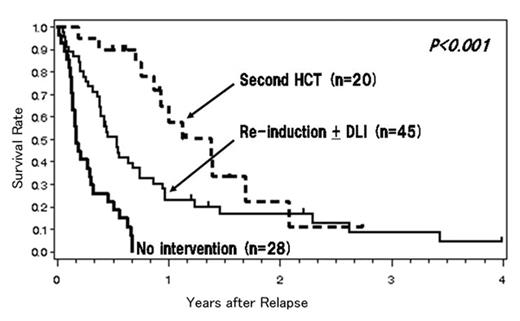
Salvage transplantation: Forty-five patients (15 in CR and 30 in non-CR) did not undergo a second HCT due to various reasons including progressive disease (n=28), infection (n=6), GVHD (n=3), refusal (n=3), and rather stable disease (n=5). Overall, 20 patients underwent salvage HCT using myeloablative (n=8) or reduced-intensity (n=12) conditioning: 11 in CR and 9 in non-CR. The incidence of TRM after the second HCT was not remarkable (5%). The probability of achieving CR after the second HCT was 75%, compared to 35% after other interventions (p=0.001), and the 1-year OS after relapse was significantly better in patients with the second HCT than that in others (58% vs 14%, p<0.0001), but these favorable outcomes may simply reflect the patient-selection bias. The 2-year OS did not differ between the two groups, which suggests that it is difficult to maintain CR after a second HCT. Currently, 15 of the 93 patients (16%) are alive with a median follow-up of 346 days (range; 33 to 1456 days), and 10 of these patients are still in CR. Notably, 5 patients are alive in CR without a second HCT: 3 suffered from central nervous system relapse without systemic relapse and received localized therapy alone (follow-up; 494 to 1456 days), and the remaining 2 have had a rather short follow-up after DLI. Multivariate analysis showed that re-induction chemotherapy, CR after intervention, a second HCT, and a longer time to post-transplantation relapse (≥100 days) were associated with improved OS after relapse.
Conclusion: For patients with chemosensitive systemic relapse, a second allogeneic HCT may improve survival and could be considered as an effective therapeutic option.
Author notes
Disclosure: No relevant conflicts of interest to declare.