Abstract
Background: In childhood acute lymphoblastic leukemia (ALL), a rapid decline of circulating blasts in response to induction chemotherapy or prednisone is one of the most important prognostic factors for achieving remission and for relapse-free survival (RFS). However, in AML parameters of chemosensitivity have been restricted to the assessment of residual bone marrow (BM) blasts during aplasia. We hypothesized that time to peripheral blood (PB) blast clearance would have prognostic relevance with respect to RFS in AML.
Methods: From 1994 to 2006 outcomes of 86 adults (47 males; median age 52 y) with previously untreated AML (non- acute promyelocytic leukemia) achieving CR and receiving high-dose cytarabine (HDAC)-based consolidation have been included in this retrospective analysis. The median and range of white blood cell count (WBC), platelet count and PB blast percent were 5.3 × 109/L (0.9–267), 59 ×109/L (5–361) 22.5% (0–97), respectively. A 100 cell manual slide differential count was done in all with PB blasts unless the WBC was less than 0.5 ×109/L. Karyotype was classified as favorable, intermediate and unfavorable in 10, 63 and 12 cases, respectively and failed in one. Induction consisted of idarubicin at 12 mg/m2/ d (n=70) or daunorubicin at 45 mg/m2/d (n=16) on days 1–3 with infusional cytarabine at 100 mg/m2/ d on days 1–7 and repeated in those with persistent BM blasts on day 14 (n=17). The first consolidation was the same as that used to achieve CR. Thereafter, 3 courses of HDAC at 3g/m2 (1.5 g/m2 if ≥ 60 y) q12 h on days 1, 3 and 5 were planned.
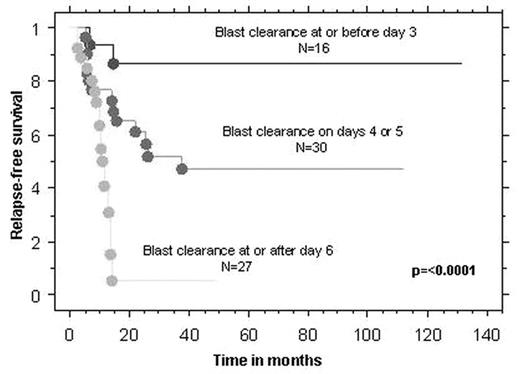
Results: At the time of analyses, 43% had died, primarily of relapse (97%). Median overall survival (OS) and RFS were 30.2 m (5.5–133) and 14 m (2–131.5), respectively. The median time to PB blast clearance was five days (range: 2–10). For this analysis, only those with PB blasts at initiation of induction (n=73) were included. We defined the day of PB blast clearance as the first day after commencing induction that PB blasts were absent. Separation according to blast clearance on or before day 5 resulted in the most balanced distribution and strongest significant difference between each subgroup of 45 and 28 patients, with significantly different rates of relapse of 33% and 79%, respectively (p<0.0001). We also defined three “blast risk groups” as good, intermediate and poor, according to PB blast clearance on or before day 3, on days 4 or 5, or on day 6 or beyond, respectively. This provided 3 well-balanced groups (good, intermediate and poor) of 16, 30 and 27 patients with significantly different and escalating relapse rates of 12.5%, 47% and 78%, respectively (Fig 1). Univariate analysis of several variables identified PB blast clearance day (p<0.0001), number of inductions to CR (p =0.0043) and cytogenetic risk group (p=0.028) as being significantly associated with RFS. On multivariable analysis, only the first sustained its significance. The results were similar for OS.
Conclusion: In adults who achieve CR after induction chemotherapy for non-APL AML, early PB blast clearance predicts superior RFS and OS.
Author notes
Disclosure: No relevant conflicts of interest to declare.