Abstract
Allogeneic hematopoietic stem cell transplantation (HSCT) is a treatment option with curative potential that exploits graft versus myeloma effect (GVM). However, myeloablative allogeneic HSCT has been associated with high transplant-related mortality and its impact on risk of relapse has been questioned. The differences in conditioning regimens, GVHD prophylaxis and short follow up have limited our ability to assess the impact of GVM when comparing allogeneic and autologous HSCT.
Method: We evaluated the long term outcomes of 74 consecutive patients under the age of 60 who underwent autologous (n=46) or related allogeneic HSCT (n=28) between 3/1994 and 12/2000 following a single myeloablative conditioning regimen of TBI (3 Gy daily on days -10 to -8), oral Busulfan 2.4 mg/kg per day (day -7 to -4) and Cyclophosphamide 60 mg/kg IV daily (day-3 and -2). GVHD prophylaxis was tacrolimus or cyclosporine with or without methotrexate.
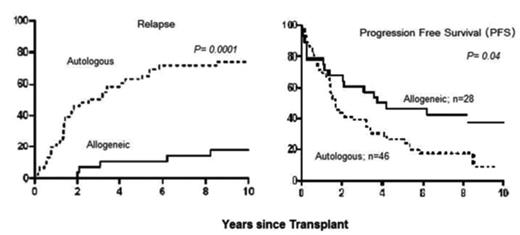
Results: There were no significant differences observed between groups in regard to gender, immunoglobulin subtype, stage, and time to HSCT and disease status at HSCT. However, there were younger patients with advanced disease in the allogeneic group (Table 1). With median follow up of 10 years as of 12/2006, the allogeneic group had superior progression free survival than autologous group (37% v 9%; P = 0.04). After HSCT, 12 of 22 and 9 of 39 evaluable patients improved to complete remission in the allogeneic and autologous group, respectively (55% v 23%; P=0.02). Overall survival favored the allogeneic group but was not statistically significant (46% v 23%; P=0.56). The cumulative incidence of relapse was 18% in the allogeneic group and 74% in the autologous group (P=0.0001). The cumulative incidence of non-relapse mortality (NRM) was 32% in allogeneic group and 11% in autologous group (P=0.001). The cumulative incidence of acute GVHD (grade II-IV) was 46% and the cumulative incidence of chronic GVHD was 73%.
Conclusion: The superior long term progression free survival and lower relapse rate in the allogeneic group suggests strongly GVM effect. However, the NRM in the allogeneic group partially offset the overall survival benefit. The higher than expected OS rate for both allogeneic and autologous group may be related to a beneficial effect of myeloablative conditioning. Future strategies with reduced toxicity myeloablative conditioning regimens and improved GVHD prophylaxis may reduce NRM while harnessing GVM effect.
Selected Characteristics
| Characteristics . | Autologous . | Allogeneic . | P . |
|---|---|---|---|
| HSCT; hematopoietic stem cell transplantation, CR; complete remission, PR; Partial remission | |||
| Median age at HSCT; y (range) | 53 (38–59) | 47 (30–56) | 0.01 |
| Disease status at HSCT, n | 0.12 | ||
| CR | 11 (24%) | 2 (7%) | |
| PR | 32 (70%) | 22 (79%) | |
| Stable or progressive | 3 (6%) | 4 (14%) | |
| Disease Status after HSCT, n | 0.79 | ||
| CR | 20 (44%) | 14 (50%) | |
| PR | 13 (28%) | 8 (29%) | |
| Stable or progressive | 6 (13%) | 0 (0%) | |
| Non-evaluable | 7 (15%) | 6 (21%) | |
| Characteristics . | Autologous . | Allogeneic . | P . |
|---|---|---|---|
| HSCT; hematopoietic stem cell transplantation, CR; complete remission, PR; Partial remission | |||
| Median age at HSCT; y (range) | 53 (38–59) | 47 (30–56) | 0.01 |
| Disease status at HSCT, n | 0.12 | ||
| CR | 11 (24%) | 2 (7%) | |
| PR | 32 (70%) | 22 (79%) | |
| Stable or progressive | 3 (6%) | 4 (14%) | |
| Disease Status after HSCT, n | 0.79 | ||
| CR | 20 (44%) | 14 (50%) | |
| PR | 13 (28%) | 8 (29%) | |
| Stable or progressive | 6 (13%) | 0 (0%) | |
| Non-evaluable | 7 (15%) | 6 (21%) | |
Author notes
Disclosure: No relevant conflicts of interest to declare.