Abstract
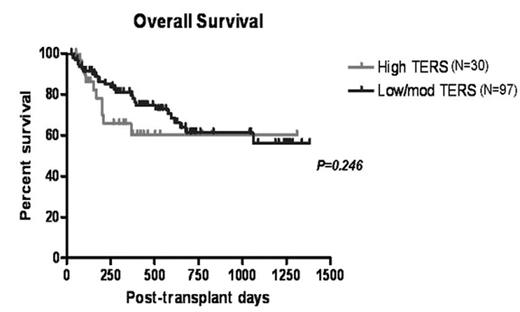
Several studies have begun to examine the relationship between psychosocial variables and outcome in hematopoietic stem cell transplantation (HSCT). Data presented at the 2006 ASH Convention, demonstrated a significant relationship between psychosocial variables, such as those assessed on the Transplant Evaluation Rating Scale (TERS), and objective outcomes, such as length of hospitalization and survival. The 2006 data included 200 consecutive patients (136 autologous, 65 allogeneic) undergoing HSCT. Based on the patient’s TERS score, each patient was stratified into one of two groups (low/moderate risk (n=173) vs. high risk (n=28)) based on their predicted psychosocial risk for problems during transplant. With the addition of 166 patients (Current N=366: 239 autologous, 127 allogeneic) the difference in length of hospitalization between low/moderate risk (10 days) versus high risk (19 days) patients remains significant (p<.02). For allogeneic patients (N=127), there continues to be an improved overall survival in low/moderate risk patients in the first 12 to 18 months following HSCT compared to high risk patients (p = .246). To determine whether similar factors impact utilization of resources in patients undergoing HSCT, we prospectively conducted psychosocial assessments on 112 consecutive allogeneic HSCT patients. An analysis of cost was completed for all patients in both the low/moderate risk group and high risk group. The mean cost differential for high risk patients is noted to be 27% higher than those patients in the low/moderate risk group (p = .122). This trend reinforces earlier data presented and suggests a correlation between pre-transplant psychosocial risk factors and resource utilization in HSCT.
Overall Survival
Author notes
Disclosure: No relevant conflicts of interest to declare.