Abstract
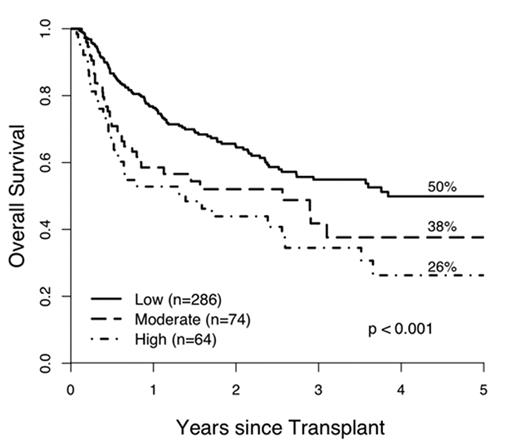
There are no independent laboratory diagnostic tests for acute GVHD. We first identified 7 potential plasma biomarkers (IL-2R-α, CRP, IL-8, TIMP-1, TNFR1, HGF, CA-19.9) of acute GVHD using a combination of proteomic approaches and antibody microarrays. We next conducted a retrospective analysis using plasma samples from 424 patients at the University of Michigan under IRB approval. We obtained samples at the first clinical signs of acute GVHD prior to treatment and at equivalent time points in patients without GVHD (Table 1). The median duration of follow-up was 420 days with a minimum follow-up of 180 days. Patients with veno-occlusive disease, idiopathic pneumonia syndrome, or septic shock were not included. We measured plasma levels of the 7 proteins by sequential ELISA. Logistic regression models with and without leave-one-out-cross-validation (LOOCV) tested the correlation of the laboratory values with the diagnosis of acute GVHD using area under the receiver-operating-characteristic (ROC) curves (AUC). The training set consisted of 282 randomly selected patients; the validation set included the remaining 142 patients. The final optimal fingerprint of four proteins excluded CRP because of its association with non-specific inflammation and included IL-2R-α, TNFR1, IL-8 and HGF, with AUCs of 0.91 and 0.89 in the training set (without and with LOOCV, respectively) and 0.86 in the validation set. The fingerprint had a strong association with grade of GVHD (p<0.001) and target organ (p=0.002) at onset; interestingly, HGF had the strongest association. Using a predicted probability of acute GVHD of at least 50%, the fingerprint had a 72% sensitivity and 89% specificity. When we categorized the predicted risk of acute GVHD into low (0.00–0.59), moderate (0.60–094) and high (0.95–1.00), the plasma fingerprint predicted long-term survival (Figure 1, p<0.001). We conclude that this plasma protein fingerprint has good sensitivity, high specificity, strong association with initial grade and target organ of acute GVHD, and effectively stratifies patients into three risk groups for GVHD that correlate with long term survival.
Figure
Patients characteristics
| . | GVHD- (N=242) . | GVHD+ (N=182) . | |||
|---|---|---|---|---|---|
| Age-yr Median (range) | 45 (1–69) | 49 (1–71) | |||
| Donor type (%) | MRD: 169 (70%) | MRD: 105 (58%) | |||
| URD: 73 (30%) | URD: 77 (42%) | ||||
| Conditioning regimen Intensity (%) | Full: 182 (75%) | Full: 114 (63%) | |||
| Reduced: 60 (25%) | Reduced: 68 (37%) | ||||
| Day after BMT of samples : median (range) | 30 (7–104) | 29 (5–119) | |||
| Grade at GVHD Onset (%) | Grade 0 | Grade 1 | Grade 2 | Grade 3–4 | |
| 242 (57%) | 48 (12%) | 100 (24%) | 34 (7%) | ||
| Organ Target at GVHD Onset (%) | n/a | Skin | Gut | Liver | Combined |
| 119 (65%) | 38 (21%) | 7 (4%) | 18 (10%) | ||
| . | GVHD- (N=242) . | GVHD+ (N=182) . | |||
|---|---|---|---|---|---|
| Age-yr Median (range) | 45 (1–69) | 49 (1–71) | |||
| Donor type (%) | MRD: 169 (70%) | MRD: 105 (58%) | |||
| URD: 73 (30%) | URD: 77 (42%) | ||||
| Conditioning regimen Intensity (%) | Full: 182 (75%) | Full: 114 (63%) | |||
| Reduced: 60 (25%) | Reduced: 68 (37%) | ||||
| Day after BMT of samples : median (range) | 30 (7–104) | 29 (5–119) | |||
| Grade at GVHD Onset (%) | Grade 0 | Grade 1 | Grade 2 | Grade 3–4 | |
| 242 (57%) | 48 (12%) | 100 (24%) | 34 (7%) | ||
| Organ Target at GVHD Onset (%) | n/a | Skin | Gut | Liver | Combined |
| 119 (65%) | 38 (21%) | 7 (4%) | 18 (10%) | ||
Author notes
Disclosure: No relevant conflicts of interest to declare.