Abstract
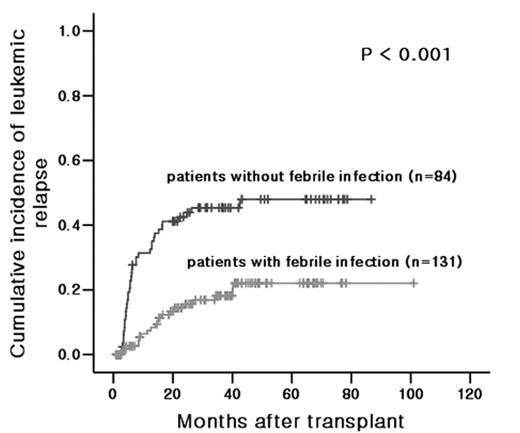
The therapeutic potential of allogeneic hematopoietic stem cell transplantation (HSCT) for leukemia relies on the graft-versus-leukemia (GVL) effect, which eradicates residual malignant cells through an immunological reaction between the donor immune cells and the recipient leukemic cells. A complex network of immune cells and cytokines mediates the GVL effect. As the infection activates immune cells and releases various inflammatory cytokines, it can change the milieu of GVL and influence the risk of post-transplant relapse. The infection usually occurs early after myeloablative allogeneic HSCT, and the activation of host antigen presenting cells, donor T cells and donor NK cells has been shown to occur quite early for experimental allogeneic HSCT. We have investigated whether infection early after allogeneic HSCT is associated with the relapse and the incidence of graft-versus-host disease (GVHD) in patients with acute leukemia. At a single transplantation center between January 2000 and May 2006, 215 patients with acute leukemia that underwent myeloablative allogeneic HSCT from a HLA-matched donor in a first complete remission state were analyzed. The median follow-up period was 30 months (range, 0.8–101.0 months). The conditioning regimens for the transplants of all the patients consisted of total body irradiation and cyclophosphamide. The analysis revealed that patients that had experienced a febrile infection that was were cause by bacteria or a fungus early after transplant had a lower actuarial probability of leukemic relapse than patients that did not experience a febrile infection (P < 0.001). However, relapse-free survival was not different between the two groups (P = 0.419) because of high early death rate in the patients who experienced febrile infection. Non-febrile infections such as cytomegalovirus infection and herpes infection were not statistically relevant to leukemic relapse (P = 0.114). An early post-transplant febrile infection was not relevant to acute GVHD (P = 0.69). Using the multivariate Cox proportional hazard model, early post-transplant infection (hazard ratio = 0.420; 95% CI = 0.209–0.845; P=0.015), chronic GVHD (hazard ratio = 0.495; 95% CI = 0.275–0.890; P=0.019) and unfavorable cytogenetics (hazard ratio = 2.324; 95% CI= 1.253–4.310; P=0.007) were independent prognostic factors for post-transplant relapse. These findings indicate that a febrile infection, but not a non-febrile infection, in the early posttransplant period can reduce the risk of leukemic relapse after allogeneic HSCT, but may not induce GVHD, presumably by enhancing the GVL reaction with sparing GVHD. Our analysis suggests that it may be valuable to study the effect of cytokines that are released during febrile infection, as the cytokines may be able to be used to potentiate the GVL effect without enhancing GVHD to maintain a long-term complete response after allogeneic HSCT.
Author notes
Disclosure: No relevant conflicts of interest to declare.