Background: Autologous stem cell transplantation is an effective treatment modality for patients with multiple myeloma. While most of the patients relapse after ASCT with a median time to progression of 2 years, there is a significant heterogeneity in the duration of response. It has been hypothesized that the effect of high dose alkylator therapy used for conditioning may have a dual effect on the myeloma cells as well as marrow microenvironment. It is also known that hematopoiesis, especially thrombopoiesis, depends to some extent on signals form the marrow microenvironment. We examined if there was any relationship between delayed platelet engraftment and outcome after ASCT.
Methods: We examined the outcomes in a group of patients undergoing ASCT for myeloma at our institution to compare the response duration to platelet engraftment kinetics. We studied 687 patients undergoing ASCT with melphalan conditioning followed by peripheral blood stem cell transplant.
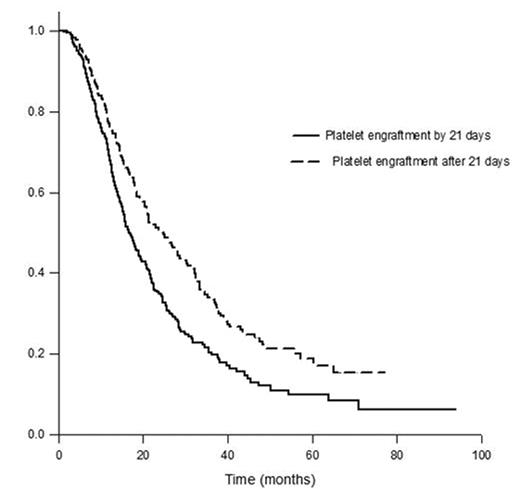
Results: Among the 687 patients undergoing ASCT, 200 pts (29%) achieved a platelet count of 50,000 by day 21 (early group) and the rest achieved this level after 21 days or never engrafted (late group). The median time to progression (TTP) among the late group was 24.8 months (95% CI; 19.6, 30 months) vs. 16.8 months (95% CI; 15.1, 18.6 months) for the late group (p < 0.001) (Figure). Patients in the late engraftment group were more likely to achieve a complete response compared to the early group; 39% vs. 30%, p = 0.02. In a multivariate analysis examining factors predicting for longer time to progression after ASCT, delayed platelet engraftment was independent of transplant within 12 months of diagnosis, CR with ASCT, absence of cytogenetic abnormalities, B2M < 3.5 mg/L and a plasma cell labeling index < 1% at the time of ASCT (Table).
Conclusions: In this study, we have demonstrated for the first time a relationship between delayed platelet engraftment after ASCT and the duration of response following ASCT. This intriguing finding raises several hypotheses. It is possible that the delayed platelet engraftment is a marker of marrow microenvironment dysfunction secondary to high dose therapy, given the role of marrow microenvironment on thrombopoiesis. It is possible that this is a surrogate marker for the biological effectiveness of the melphalan dose, which can affect the other cells in the marrow microenvironment as well. It is likely a reflection of the marrow microenvironment dependence on the myeloma cells for its survival. These findings should be confirmed in other larger patient groups.
Predictors of progression
| Variable . | Hazard Ratio . | P . |
|---|---|---|
| Platelet Engraftment > 21 days | 0.80 (0.60, 0.96) | 0.02 |
| Late transplant (>12 months from diagnosis) | 1.6 (1.3, 2.0) | <0.01 |
| Plasma cell labeling index > 1% | 1.9 (1.5, 2.4) | <0.01 |
| Complete response | 0.41 (0.33, 0.51) | <0.01 |
| Abnormal Cytogenetics | 1.8 (1.4, 2.3) | <0.01 |
| B2M > 3.5 | 1.2 (0.96, 1.5) | 0.12 |
| Variable . | Hazard Ratio . | P . |
|---|---|---|
| Platelet Engraftment > 21 days | 0.80 (0.60, 0.96) | 0.02 |
| Late transplant (>12 months from diagnosis) | 1.6 (1.3, 2.0) | <0.01 |
| Plasma cell labeling index > 1% | 1.9 (1.5, 2.4) | <0.01 |
| Complete response | 0.41 (0.33, 0.51) | <0.01 |
| Abnormal Cytogenetics | 1.8 (1.4, 2.3) | <0.01 |
| B2M > 3.5 | 1.2 (0.96, 1.5) | 0.12 |
Figure
Disclosure: No relevant conflicts of interest to declare.