Abstract
Acquired imatinib resistance in advanced Philadelphia-positive acute lymphoblastic leukemia (Ph+ ALL) has been associated with mutations in the kinase domain (KD) of BCR-ABL. We examined the prevalence of KD mutations in newly diagnosed and imatinib-naive Ph+ ALL patients and assessed their clinical relevance in the setting of uniform frontline therapy with imatinib in combination with chemotherapy. Patients enrolled in the German Multicenter Study Group for Adult Acute Lymphoblastic Leukemia (GMALL) trial ADE10 for newly diagnosed elderly Ph+ ALL were retrospectively examined for the presence of BCR-ABL KD mutations by denaturing high-performance liquid chromatography (D-HPLC), cDNA sequencing, and allele-specific polymerase chain reaction (PCR). A KD mutation was detected in a minor subpopulation of leukemic cells in 40% of newly diagnosed and imatinib-naive patients. At relapse, the dominant cell clone harbored an identical mutation in 90% of cases, the overall prevalence of mutations at relapse was 80%. P-loop mutations predominated and were not associated with an inferior hematologic or molecular remission rate or shorter remission duration compared with unmutated BCR-ABL. BCR-ABL mutations conferring high-level imatinib resistance are present in a substantial proportion of patients with de novo Ph+ ALL and eventually give rise to relapse. This provides a rationale for the frontline use of kinase inhibitors active against these BCR-ABL mutants.
Introduction
Incorporation of the ABL kinase inhibitor imatinib into frontline treatment of Philadelphia-positive acute lymphoblastic leukemia (Ph+ ALL) has significantly improved the antileukemic efficacy of induction therapy. Several cooperative ALL study groups have demonstrated complete remission rates consistently above 90%, irrespective of whether imatinib is used alone or combined with multiagent chemotherapy.1-9 These results are superior to previously reported complete remission (CR) rates of 65% to 90% in younger patients10-13 and 40% to 60% in Ph+ ALL patients older than 60 to 65 years of age.14-17 Although accumulating evidence suggests that imatinib-containing therapeutic regimens may also improve long-term outcome in these patients,3,6-8,14 relapse remains a predominant cause of treatment failure.3,7-9
Numerous point mutations in the kinase domain (KD) of BCR-ABL that impair imatinib binding to varying degrees have been identified as a major mechanism of acquired resistance in patients with chronic myeloid leukemia (CML).18-25 Data on BCR-ABL mutations in patients with Ph+ ALL or lymphoid blast crisis of CML are more limited. Two studies of patients with advanced Ph+ lymphoid leukemias identified 5 different KD mutations in 14 of the 17 evaluated patients with acquired resistance to imatinib.26,27 Preponderance of the E255K/V P-loop mutation, which occurred in 6 of 9 patients (67%) following their treatment with imatinib was suggested by one of these reports26 but not by the other.27 However, all point mutations arose at positions within the KD that are known to be important for drug binding and to confer significant resistance to imatinib in vitro.18-20 This demonstrated that different mutations within the BCR-ABL KD can be responsible for refractoriness of Ph+ lymphoid leukemias to imatinib, and also suggested that KD mutations may be a frequent mechanism of acquired imatinib resistance during salvage therapy with imatinib. Moreover, the short median time to progression of 2 to 3 months in these patients raised the possibility that KD mutations might pre-exist before imatinib is started.28-30 However, BCR-ABL KD mutations were not detected in patients with chemotherapy-resistant acute lymphoid leukemia prior to imatinib treatment by Hofmann et al26 or von Bubnoff et al,27 both of whom used a direct sequencing approach. Using a more sensitive cloning and sequencing strategy, we subsequently demonstrated the presence of a low-level KD mutation in 2 of 4 patients with advanced, imatinib-naive Ph+ ALL, suggesting that pre-existing imatinib-resistant mutant clones may be positively selected in some patients.31 These findings are analogous to the detection of drug-resistant mutants in pretreatment samples in some CML patients who had not yet received imatinib; these were predominantly patients with advanced disease who were known to have subsequently developed imatinib resistance.20,32-35 The proportion of mutant alleles in these studies was mostly low, necessitating the use of highly sensitive detection techniques. Interestingly, one of these studies found a positive correlation between the presence of mutations and prior exposure to thioguanine,35 suggesting that treatment history, particularly with regard to certain types of prior chemotherapy, may have a significant impact on the prevalence of KD domain mutations in imatinib naive patients.
By means of highly sensitive denaturing high-performance liquid chromatography (D-HPLC) (WAVE) and allele-specific oligonucleotide–polymerase chain reaction (ASO-PCR) and by cDNA sequencing, we investigated the prevalence, pattern, and evolution of BCR-ABL KD mutations in pretherapeutic leukemic samples and bone marrow samples collected throughout imatinib-based therapy from patients with newly diagnosed Ph+ ALL, and in leukemic samples from relapsed patients. The results of mutational analysis were correlated with hematologic response, BCR-ABL transcript levels measured by quantitative and nested reverse transcription (RT)–PCR and remission duration in this cohort of elderly Ph+ ALL patients who had been enrolled in a prospective study exploring frontline treatment with imatinib in combination with repeated cycles of chemotherapy.9,36
Patients, materials, and methods
Patients
Bone marrow samples were collected prior to and serially throughout imatinib-based therapy from patients with de novo Ph+ ALL who were enrolled in a prospective, randomized clinical trial of the German Multicenter Study Group for Adult Acute Lymphoblastic Leukemia (GMALL) study group investigating frontline imatinib-based therapy in elderly patients. The overall design of this clinical study has been described in detail previously.9,36 Briefly, patients older than 55 years with newly diagnosed Ph+ ALL who had received no ALL treatment other than brief prephase therapy with cyclophosphamide and dexamethasone were randomly assigned to receive a 4-week induction with either imatinib or chemotherapy, followed by extended therapy with imatinib and parallel chemotherapy that was identical for all patients independent of the initial randomization. The trial was approved by the Ethics Committee of the University of Frankfurt (Frankfurt, Germany). Prior to the study, informed consent was obtained in accordance with the Declaration of Helsinki.
Bone marrow samples
Samples (5-10 mL) for the present retrospective analysis were available from 48 of the 55 patients enrolled in the randomized trial described in “Patients.” A total of 365 bone marrow (n = 271) or blood (n = 94) samples were harvested prior to and during treatment or at relapse. In the majority of cases, mononuclear cells were separated by Ficoll centrifugation and mRNA was extracted and reverse-transcribed to cDNA, which was stored at −20°C. Alternatively, cDNA was obtained in an identical manner from viable cells that had been cryopreserved and stored in liquid nitrogen according to standard procedures.
Samples collected at or soon after diagnosis were available from 42 patients, including pretreatment samples from 22 patients and samples obtained during the first 4 weeks of induction from 20 patients. Of the latter group, 10 patients had been allocated to induction chemotherapy and thus were imatinib naive at the time of first mutational analysis, and 10 patients had received a maximum of 4 weeks of imatinib by the time of first evaluable analysis.
Relapse samples were available for mutational analysis from 26 of the 27 patients who have relapsed to date. To explore the kinetics of mutations during successive consolidation cycles, we analyzed a total of 300 samples collected throughout study treatment. In 30 patients, samples were available from at least 5 time points, and in 7 patients from 4 time points. Clinical results from this randomized trial are reported in detail elsewhere.9
Mutational analysis by direct sequencing
Heminested PCR was performed essentially as described by Hochhaus et al22 using the following primers: first step, B2B (bcr exon 13; ACAGCATTCCGCTGACCATCAATAAG) or Bcr-C (bcr exon 1; ACCGCATGTTCCGGGACAAAAG) plus A7− (Abl exon 7, AGACGTCGGACTTGATGGAGAACT); second step, AN4+ (Abl exon 4, AGACGTCGGACTTGATGGAGAACT) plus A7−. A 15-μL aliquot of the PCR product (675 bp) encoding the bcr-abl ATP binding pocket and the activation loop was purified (QIAquick PCR Purification kit; Qiagen, Hilden, Germany) and sent for direct sequencing to a commercial laboratory (MWG Biotech, Ebersberg, Germany). Sequences were compared with the unmutated sequence by use of Embl Alignment (ABL, accession no. U07563). Sequence analysis was performed on both strands for each fragment.
Analysis of BCR-ABL KD mutations
RNA extraction and reverse transcription–PCR.
Total cellular RNA was obtained by phenol-chloroform extraction, isopropanol precipitation, and washing with 700 mL/L ethanol. RNA was quantified spectrophotometrically at 260 and 280 nm. Total cellular RNA (maximum, 3 μg) was reverse-transcribed to cDNA by use of 5 μM random hexamer primers and 200 U of M-MLV reverse transcriptase (Promega, Mannheim, Germany).
Denaturing HPLC.
We employed the methodology for D-HPLC detection of BCR-ABL mutations essentially as described by Soverini et al37,38 with modifications of the primers and temperatures. A nested PCR was performed using the following primers: F-Bcr-A or ALL-TB plus R-Abl-A; second step, F-Abl-B/R-Abl-B and F-Abl-C/R-Abl-C. In this way, the Abl kinase domain was divided into 2 partially overlapping sequences: Abl-B spanning codons 206 to 335 and Abl-C spanning codons 262 to 421. Primer sequences were as follows (5′- 3′): ALLTB, GCA AGA CCG GGC AGA TCT; F-Bcr-A, GAG CAG CAG AAG AAG TGT TTC AGA; R-Abl-A, CTC TAG CAG CTC ATA CAC CTG GG; F-Abl-B, CAT CAT TCA ACG GTG GCC GAC GG; R-Abl-B, GTT GCA CTC CCT CAG GTA GTC; F-Abl-C, GAA GAA ATA CAG CCT GAC GGT G; and R-Abl-C, CGT CGG ACT TGA TGG AGA A.
Aliquots of 10 μL of this PCR product was injected into a semiautomated high-throughput D-HPLC system WAVE (Transgenomic, Omaha, NE). Separation was performed on DNAsep cartridge (ion pair reverse-phase C18 column; Transgenomic) under “Mutation detection” application type and ultraviolet (UV) detection at 260 nm. The optimal melting T° for each mutation was selected using standard Stanford DHPLC melt program (http://insertion.stanford.edu/melt.html). Nevertheless, the elution profiles of all PCR products were determined at several different temperatures: 60°C, 61°C, 62°C, or 64°C for Abl-B and 60°C, 61°C, and 62°C for Abl-C. The mobile phase was 0.1 M triethylammonium acetate (TEAA) solution in water (pH 7) (buffer A) and 0.1 M TEAA and 25% acetonitril (buffer B). The PCR product was eluted at a flow rate of 0.9 mL/min with a gradient of 40% to 72% for buffer B over 8 minutes. Navigator 1.5.3. Software (Transgenomic) was used for data analyses. The chromatograms of investigated patient samples were compared with those of wild-type (WT) (ie, unmutated) controls. Samples showing a chromatogram different from WT were scored as positive. If there was no PCR product at a given time point despite sufficient sensitivity of the assay, the sample was considered unmutated.
Optimization of mutation detection was performed by mixing the PCR products known to be positive for individual mutations (M244V, G250E, E255K, E255V, T315I, F317L, M351T, E355G, F359C, F359V, L384M) in a 1:1 ratio with the PCR products of unmutated BCR-ABL. A specific abnormal elution profile was received for each sequencing variation at optimal melting T°. The results were confirmed by direct sequencing. A detection limit of the dHPLC system in the range of 0.05% to 0.01% was established by performance of titration dilutions starting from 100% to 0.01%, mixing PCR product of each mutation with WT.
Confirmation of E255K and T315I mutations with allele-specific PCR
In order to confirm the results obtained with D-HPLC by another method, aliquots of RNA from samples harboring the E255K or T315I mutation as indicated by D-HPLC (n = 23) were sent in a blinded manner to the University of Leipzig. Samples were then reverse transcribed and analyzed by 3 runs of ASO-PCR as previously described35 with minor modification on an ABI (Applied Biosystems Inc., Darmstadt, Germany) 7300 System using Sybr Green (Bio-Rad Laboratories, Hercules, CA) fluorescence.
Samples were scored positive if (1) at least one run showed a positive result, (2) amplification was detected at least 2 cycles before the maximum cycle number of the assay (≤ 48 cycles), (3) the melting curve was identical to the positive control (to exclude fluorescence from nonspecific amplification products), and (4) no specific amplification was detected from any of the BCR-ABL wild-type or BCR-ABL–negative controls before cycle 49.
In each individual experiment, the sensitivity was monitored by amplification of a serial dilution of E255K or T315I plasmid DNA. Strict precautions were taken to avoid false-positive results.
Statistical methods
Differences in response rates in relation to the mutational status at start of treatment were analyzed by Fisher exact test. Remission duration in patients with and without early mutations were plotted according to the methods of Kaplan-Meier, with differences between patient groups analyzed by the log-rank test. Statistical analyses were performed using the GraphPad Prism (GraphPad Software, San Diego, CA) software package.
Results
Frequency and type of KD mutations at relapse
Leukemic cells collected during relapse were available for mutational analysis from 26 (bone marrow [BM], n = 22; peripheral blood [PB], n = 4) of the 27 patients who were enrolled in the GMALL study for elderly Ph+ ALL (ADE10) and have relapsed to date. Details of this randomized phase II trial are reported elsewhere.9 Direct sequencing identified a BCR-ABL KD mutation in 21 of the 26 patients (84%), exclusively unmutated BCR-ABL was found in relapse samples from 5 patients (16%). The mutations and their frequencies are depicted in Table 1. P-loop mutations predominated with an overall frequency of 46% (12 of 26 patients), the gatekeeper mutation T315I was identified in 4 (15%) patients. Mutations in the activating loop were uncommon (n = 2), and no mutations were located in the catalytic domain. A dual mutation was identified in 2 patients, T315I/E255K and L384M/Y253H, respectively. The mutant clone consistently was the dominant population: it exceeded 50% in all relapse samples. To ensure that mutations present only in minor subclones of the ALL cells were not missed due to the limited sensitivity of direct sequencing, relapse samples from 18 patients, including 3 of the 5 patients with unmutated BCR-ABL, were subjected to D-HPLC analysis. The elution profile was consistent with the mutational status determined by sequencing in all cases; no additional mutations were detected in any of the samples.
Frequency and type of mutations prior to imatinib
To determine whether BCR-ABL mutations were already present prior to the first imatinib exposure, we examined all 32 imatinib-naive patients from whom samples (BM, n = 21; PB, n = 11) had been collected at the time of diagnosis (n = 22) or within the first 4 weeks of induction chemotherapy (n = 10), irrespective of whether or not they eventually relapsed. Utilizing a sensitive D-HPLC technique (WAVE), a mutation was detected in 12 of the 32 (37.5%) preimatinib samples available for analysis (Table 2). The elution profile of the D-HPLC indicated a P-loop mutation in 83% (10 of 12 patients) and a T315I mutation in 17% (2 of 12 patients) of these cases.
Bone marrow samples collected during the first 2 weeks (n = 5) or during the fourth week of imatinib induction (n = 5) were available for D-HPLC analysis from an additional 10 patients. A KD mutation was detected in 5 of these 10 patients (G250E, n = 1; E255K, n = 2; T315I, n = 1; F317L, n = 1), and 5 patients displayed unmutated BCR-ABL (n = 4) or yielded no PCR product despite good assay sensitivity (n = 1). Interestingly, mutations were detected more frequently in samples from patients who had received imatinib for 4 weeks (4 of 5; 80%) than in patient samples obtained within the first 2 weeks of imatinib treatment (1 of 5; 20%) (P = n.s.), suggesting early selection and outgrowth of leukemic cells harboring a BCR-ABL mutation. Taken together, we detected a BCR-ABL KD mutation in 17 of the 42 (40.5%) patients who were examined prior to or during the first 4 weeks of antileukemic therapy, whereas 25 patients (59.5%) showed an initial unmutated BCR-ABL configuration (Table 2). We explored whether the presence of BCR-ABL mutations prior to imatinib were associated with age, gender, type of transcript, white blood count, or cytogenetic findings at diagnosis and found no statistically significant association with either of these parameters. The frequency of the mutant allele in all of the above-mentioned samples was always below 2% (range, 0.1%-2%).
Concordance between D-HPLC and ASO-PCR for detection of early mutations
The proportion of cells considered by D-HPLC analysis to harbor a BCR-ABL mutation during the early treatment period was too low to permit confirmation by direct sequencing. We therefore attempted to validate the D-HPLC results by means of an allele-specific PCR for the 2 most frequent mutations, E255K and T315I. There was complete concordance between D-HPLC and ASO-PCR for both the E255K mutation (12 samples from 3 patients) and the T315I mutation (8 samples from 2 patients).
Concordance between BCR-ABL mutational status before treatment and at relapse
Intraindividual comparison of the BCR-ABL status at onset of treatment and at relapse was performed in 19 of the 27 patients who have relapsed to date. As shown in Table 3, there was nearly complete concordance: in 10 of the 11 patients in whom mutant BCR-ABL was detected pretreatment, the same mutation was present at relapse. In addition, 6 of the 9 patients who presented with unmutated BCR-ABL at start of treatment showed a mutation at relapse, and 3 had unmutated BCR-ABL at relapse. Relapse was associated with a mutation other than the one detected at start of treatment in only one patient (Table 4). Our D-HPLC analysis of samples collected throughout treatment of the 30 patients in whom samples from at least 4 time points were evaluable never revealed a transient appearance of a mutation that was not subsequently present at relapse.
Hematologic and molecular response in relation to initial mutational status
The KD mutants detected in our patients are known to profoundly impair the inhibitory effect of imatinib on BCR-ABL kinase activity,18-20 raising the possibility of an inferior treatment response in patients with detectable pretreatment mutations. We therefore compared the CR rates after induction and the rates of BCR-ABL negativity during consolidation in all patients in whom results of mutational analysis conducted prior to or during induction therapy were available, irrespective of their subsequent clinical outcome (Table 5). Of the patients randomized to imatinib induction, all 9 patients with a known KD mutation (100%) and 9 of 10 patients with unmutated BCR-ABL (90%) achieved a CR. Similarly, the response to chemotherapy induction did not differ significantly between patients with a known KD mutation and those expressing unmutated BCR-ABL, with CR rates of 63% (5 of 8 patients) and 55% (6 of 11), respectively (Table 5).
To determine whether the quality of the hematologic response during study treatment differed between patients with and without an initial mutation, we compared the frequencies with which these 2 patient groups achieved BCR-ABL negativity by both quantitative (TaqMan) and nested RT-PCR analysis on at least one occasion during combined imatinib/chemotherapy consolidation (Table 5). Contrary to expectations, these data do not suggest an inferior molecular response in Ph+ ALL patients expressing most of the known BCR-ABL mutants at the start of treatment. It is noteworthy that all 3 patients harboring the T315I gatekeeper mutation achieved a CR after induction, and that BCR-ABL transcripts became temporarily undetectable during consolidation in 2 of these 3 patients, even though all 3 patients subsequently relapsed with a dominant T315I mutant population of leukemic cells.
Outcome in relation to pretreatment detection of BCR-ABL mutations
Because essentially all BCR-ABL mutations detected at the beginning of treatment convey high-grade resistance to imatinib, they may be expected to considerably impair the response to imatinib-based combination therapy. Samples for initial mutational analysis were available from 42 of the 55 patients (76%) enrolled. We compared the response duration and outcome in patients who were initially found to express either unmutated or mutated BCR-ABL. Three of the 17 patients (18%) who initially presented with a BCR-ABL mutation were nonresponders and died (all 3 randomized to induction chemotherapy), 11 patients (64%) relapsed, 2 patients (12%) died in CR, and only 1 patient (6%) was in ongoing CR 3 years after entering the study.
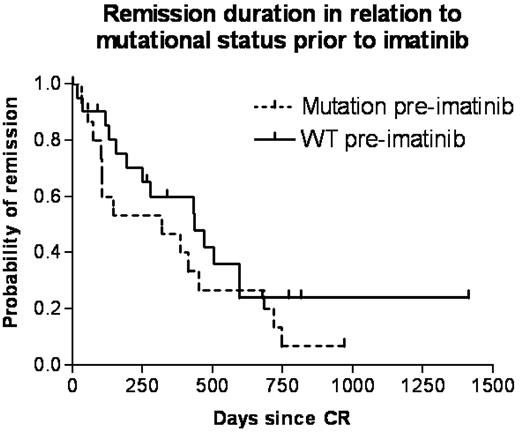
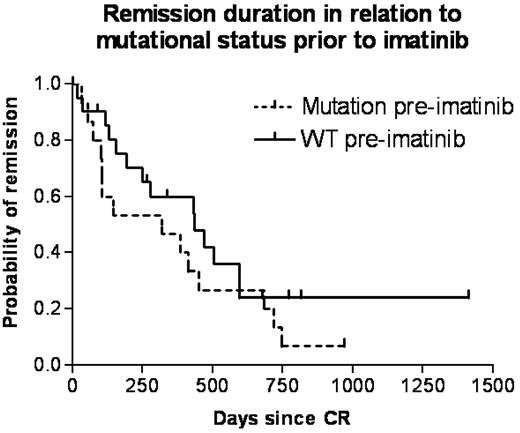
Twenty-five patients initially expressed unmutated BCR-ABL. Ten of these patients (40%) are in ongoing CR (range, 89-1412 days), 4 patients (16%) died in CR after a remission duration of 18 to 130 days, and 11 patients (44%) relapsed (median remission duration, 433 days; range, 154-596 days). Remission duration as calculated by the method of Kaplan and Meier did not differ significantly between patients with or without a detectable early mutation (Figure 1). Notably, only the small subgroup of patients with a T315I mutation (n = 3) had a shorter median time to progression (median, 102 days; range, 53-319 days) compared with 339 days (range, 18-1412 days) in patients with no mutations (n = 25) and 384 days (range, 31-970 days) for P-loop (n = 13), although patients numbers are too small to permit calculation of statistical significance.
Kaplan-Meier estimate of remission duration. Kaplan-Meier estimate of remission duration was calculated separately for patients found to have an unmutated BCR-ABL (WT; solid line) or any kinase domain mutation (hatched line) prior to imatinib exposure. Remission duration was calculated from time of first documented complete remission (CR or CRi) to hematologic relapse. Patients who died in CR were censored at the time of death (death in CR was considered a non-event for calculation of remission duration by Kaplan-Meier analysis). Median remission duration was 436 days in the group of patients with initially unmutated BCR-ABL and 319 days in patients harboring an initial KD mutation (P = .24).
Kaplan-Meier estimate of remission duration. Kaplan-Meier estimate of remission duration was calculated separately for patients found to have an unmutated BCR-ABL (WT; solid line) or any kinase domain mutation (hatched line) prior to imatinib exposure. Remission duration was calculated from time of first documented complete remission (CR or CRi) to hematologic relapse. Patients who died in CR were censored at the time of death (death in CR was considered a non-event for calculation of remission duration by Kaplan-Meier analysis). Median remission duration was 436 days in the group of patients with initially unmutated BCR-ABL and 319 days in patients harboring an initial KD mutation (P = .24).
Discussion
The prevalence of pretherapeutic BCR-ABL KD mutations in patients with newly diagnosed Ph+ ALL and the mutation frequency associated with acquired imatinib resistance is not known. Here, we demonstrate that approximately 40% of patients with de novo Ph+ ALL who had no prior exposure to imatinib and no or minimal exposure to chemotherapy, ie, prephase therapy with 5 days of dexamethasone and 3 days of low-dose cyclophosphamide, harbored a small leukemic clone with a KD mutation, and that this mutation was identical with the mutation present in the dominant leukemic population at relapse. The frequency of the mutant allele at the time of diagnosis was always below the level of detectability by direct cDNA sequencing, in agreement with previous reports by ourselves and others,26,27 and thus requires more sensitive methods for detection. D-HPLC is a highly sensitive technique that was shown for a large and diverse group of genes to be particularly useful for screening samples potentially harboring low-level mutations.39-45 Its applicability to the analysis of BCR-ABL KD mutations has been well established.37,38,46,47 In our patients, the elution characteristics indicated predominance of mutations located in the ATP binding pocket (P-loop) in 46% of cases, the E255K and G250E mutations being the most frequent. The T315I gatekeeper mutation, which directly interferes with imatinib binding and thus completely abrogates imatinib activity19 was detected in 2 patients within 4 weeks of diagnosis. To confirm that D-HPLC correctly identified the pretreatment mutations, we subjected the same samples to analysis by ASO-PCR for the most frequent E255K and T315I mutations. In all cases, results of D-HPLC and ASO-PCR identified the same mutation, thereby validating the D-HPLC results regarding the high frequency of pretherapeutic KD mutations and the accuracy of discriminating between individual mutations. Of note, all KD mutations detected in pretherapeutic or imatinib-naive samples have been shown to confer high-level imatinib resistance in vitro,18-20,48 strongly implicating these mutations in playing a causal role in the development of clinical resistance.
Remarkably, pre-existence of mutations including the T315I mutation did not adversely effect either the CR rate following imatinib or chemotherapy induction or the achievement of BCR-ABL negativity in response to combination therapy when compared with patients exhibiting only unmutated BCR-ABL at diagnosis, a finding reminiscent of CML.35 Considering the 95% CR rate, this implies that imatinib initially suppressed the dominant, unmutated leukemic population in almost all cases, without simultaneous outgrowth of the pre-existing mutant subclones. Similarly, remission duration did not differ significantly between patients with initial unmutated BCR-ABL and mutant BCR-ABL other than the T315I mutation; only the latter mutation was associated with substantially more rapid relapse, although the number of patients is too small to permit definite conclusions. Nevertheless, it is conspicuous that all but 2 patients with an up-front mutation relapsed, in contrast to an approximately 50% relapse rate among patients initially presenting with unmutated BCR-ABL. Although this difference could be due to chance, it is tempting to speculate that the leukemic cells in a subset of patients may exclusively express unmutated BCR-ABL, and that this is associated with a lower probability of relapse during imatinib therapy. Testing of this hypothesis requires prospective mutational analysis using assays with considerably greater sensitivity than those currently employed. Given the frequency with which mutations eventually appeared in patients who seemed to express only unmutated BCR-ABL at diagnosis, such mutational analysis is clearly warranted.
Taken together, our data demonstrate that the combination of imatinib with postremission consolidation chemotherapy may constrain, for a prolonged period of time, the growth of leukemic clones even if they express BCR-ABL mutations conferring high-level imatinib resistance. It is uncertain whether the minimal residual activity of imatinib against P-loop mutations enhances the antileukemic effects of chemotherapy.
Despite the high CR rate and often prolonged remission duration, all but 2 patients who were initially found to harbor a KD mutation and did not die in CR relapsed. There was nearly complete concordance between the mutations detected initially and at the time of relapse. Comparison of the mutational status up-front and at relapse revealed a switch of an initially detected KD mutation in only 1 of 11 patients in whom a mutation was detected up-front. Conversely, 67% of patients who displayed no mutation at baseline were found to have a dominant mutant clone at relapse; we were unable to determine whether mutant cells were present initially but below the detection threshold of the D-HPLC assay, or whether they developed during imatinib-based therapy. A KD mutation was observed in approximately 80% of patients at the time of relapse, in good agreement with results recently published by Soverini et al.49 Relapse involving leukemic cells expressing unmutated BCR-ABL was distinctly uncommon. As determined by direct sequencing in combination with D-HPLC, the mutant clones always became the dominant population at relapse, consistent with an expansion of pre-existing imatinib-resistant mutant clones under imatinib selection. Taken together, these results underscore the pivotal role of BCR-ABL KD mutations in acquired imatinib resistance in patients with newly diagnosed Ph+ ALL.
A recent study has found that different KD mutants of BCR-ABL display altered kinase activity and transformation potency irrespective of their sensitivity to imatinib.50 In particular, the ATP binding loop mutants Y253F and E255K exhibited increased transformation potency in relation to unmutated BCR-ABL. In the patients in our study, the mutant clones including the frequent Y253F and E255K mutants always constituted a tiny minority within the population of leukemic cells in imatinib-naive patients. These data suggest that the mutations identified most frequently in Ph+ ALL do not confer an intrinsic, clinically apparent proliferative advantage over leukemic cells expressing unmutated BCR-ABL. Most studies reporting the presence of pretherapeutic KD mutations in CML patients also found them to be present in only a minority of cells comparable with the level we established for Ph+ ALL,32-35 with the exception of one report in CML that found mutant alleles to represent 40% of the BCR-ABL message.20 It is unclear whether this discrepancy is due to methodological differences between the studies or patient selection.
As was shown recently, the kinase activity of various KD mutants does not necessarily correlate with their transforming capabilities, suggesting that additional factors influence transformation potency.50 In our study, the reappearance of a mutant leukemic clone that had been identified initially but then became undetectable by our RT-PCR in response to imatinib-based therapy heralded rapid relapse. This sudden acceleration of the growth kinetics of a leukemic clone that had been effectively suppressed for often prolonged time periods is reminiscent of the rapid outgrowth of leukemic cells harboring KD mutations in Ph+ ALL patients who received imatinib as salvage therapy in the early phase II studies (Hofmann et al26 and data not shown). This eventual loss of response to imatinib-based therapy in de novo Ph+ ALL patients is consistent with the acquisition of additional, nonmutational resistance mechanisms by the mutant clones, a concept also proposed for CML.51,52 Conceivably, the genotoxic chemotherapeutic agents used in combination with imatinib in our treatment regimen may have contributed to this type of clonal evolution as has been suggested for CML, where prior exposure to thioguanine was associated with an increased frequency of KD mutations.35 This hypothesis could also explain the significantly inferior remission rates and duration previously observed in patients with advanced Ph+ ALL who had been heavily pretreated with cytotoxic agents.29,30
In summary, BCR-ABL KD mutations conferring high-level imatinib resistance are detectable at low level in a large proportion of elderly patients with newly diagnosed and as yet untreated Ph+ ALL. These pre-existing mutant clones initially do not impart an inferior hematologic or molecular remission rate and may be suppressed for prolonged time periods by combined treatment with imatinib and chemotherapy, but they almost invariably give rise to eventual relapse. Even among patients apparently expressing only unmutated BCR-ABL at diagnosis, relapse is commonly associated with the outgrowth of a mutant clone. This finding has implications both for selection of treatment strategies and for molecular monitoring during therapy. The option of an allogeneic stem cell transplantation, possibly with reduced-intensity conditioning in the case of more advanced age, should be assessed. In patients not eligible for stem cell transplantation (SCT), an apparently good response to imatinib-based treatment should not prompt premature discontinuation of therapy. Moreover, it appears advisable to continue therapy with imatinib in combination with a different modality, eg, chemotherapy, for extended periods of time even in good molecular responders; loss of a hematologic response should prompt mutational analysis. To significantly improve outcome, it will be necessary to eliminate clones harboring KD mutations during the early phase of treatment, before they have acquired additional resistance mechanisms. The recent development of several novel ABL kinase inhibitors that possess greater activity against both unmutated BCR-ABL and most KD mutants, eg, nilotinib and dasatinib, offers great promise in this regard.53-61 These second-generation ABL kinase inhibitors are currently being incorporated into the frontline treatment of patients with newly diagnosed Ph+ ALL in clinical trials. By suppressing a greater proportion of leukemic clones harboring a BCR-ABL KD mutation, the number of leukemic cells susceptible to the accumulation of additional resistance mechanisms is likely to be reduced. Treatment efficacy may also be enhanced by combining several kinase inhibitors, because they have been shown to act synergistically and moreover are likely to complement each other with respect to their activity profile against different KD mutations.61 Such clinical trials will need to be accompanied by highly sensitive and frequent serial analyses of mutational status and minimal residual disease.
An Inside Blood analysis of this article appears at the front of this article.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The following investigators contributed by enrolling and caring for patients in the randomized, multicenter trial that forms the basis for the analysis described in this paper: Departments of Hematology and Oncology of the University Hospitals Münster (M. Stelljes); Essen (U. Dührsen); Tübingen (M. Schmalzing); Berlin/Charite (P. le Coutre); Mainz (J. Beck); Ulm (M. Schmid); Mannheim (M. Müller); Freiburg (M. Lübbert); Rostock (M. Freund); Chemnitz (A. Thiel); Berlin/Benjamin-Franklin (S. Schwartz); Kiel (M. Kneba); Marburg (A. Neubauer); Heidelberg (J. Dengler); Homburg/Saar (M. Pfreundschuh); the St. Johannes Hospital, Duisburg (A. Giagounidis); Klinikum Essen-Werden (M. Wattad); Städtische Kliniken Krefeld (M. Planker); St. Marien-Krankenhaus Siegen (W. Gassmann); Klinikum Villingen-Schwenningen (W. Brugger); Gütersloh (P. Düwel); Klinikum Neukölln, Berlin (Grüneisen); Traunstein (E. Hagenreiner); Berlin (A. Matylis); and Oldenburg (C. Schimmelpfennig) (all in Germany).
We thank Doreen Badowski, Brigitte Gehrke, Tamara Hirdes, Sandra Markovic, Heike Nürnberger, and Martine Pape for their excellent technical assistance.
This work was supported by grants from the German Federal Ministry of Education and Research (BMBF) Competence Network “Acute Leukemias” (grant 01G50441), the German Genome Research Network (NGFN), the Wilhelm Sander Stiftung and the Adolf-Messer Foundation (Germany), and Novartis Pharma AG (Nürnberg, Germany).
Authorship
Contribution: H.P. designed the study, performed experiments, analyzed data, and wrote the manuscript; B.W. conducted the clinical study, analyzed data, and wrote the manuscript; A.P., J.O., T.L., A.H., S.W., and P.B. performed experiments and analyzed data; L.W. and A.B. conducted the clinical study and analyzed data; D.H. designed the study and wrote the manuscript; and O.G.O. designed the study, conducted the clinical trial, analyzed data, and wrote the manuscript. H.P. and B.W. contributed equally to this paper.
Conflict-of-interest disclosure: O.G.O., A.H., and D.H. have received research support from Novartis. O.G.O. and A.H. have received honoraria from Novartis for advisory board activity and lectures. All other authors declare no competing financial interests.
Correspondence: Oliver G. Ottmann, Center for Internal Medicine II, Department of Hematology/Oncology, Johann Wolfgang Goethe University Frankfurt, Theodor Stern Kai 7, D-60590 Frankfurt, Germany; e-mail: ottmann@em.uni-frankfurt.de.