Abstract
Bone disease is one of the most debilitating manifestations of multiple myeloma. A complex interdependence exists between myeloma bone disease and tumor growth, creating a vicious circle of extensive bone destruction and myeloma progression. Proteasome inhibitors have recently been shown to promote bone formation in vitro and in vivo. Preclinical studies have demonstrated that proteasome inhibitors, including bortezomib, which is the first-in-class such agent, stimulate osteoblast differentiation while inhibiting osteoclast formation and bone resorption. Clinical studies are confirming these observations. Bortezomib counteracts the abnormal balance of osteoclast regulators (receptor activator of nuclear factor-κB ligand and osteoprotegerin), leading to osteoclast inhibition and decreased bone destruction, as measured by a reduction in markers of bone resorption. In addition, bortezomib stimulates osteoblast function, possibly through the reduction of dickkopf-1, leading to increased bone formation, as indicated by the elevation in bone-specific alkaline phosphatase and osteocalcin. The effect of bortezomib on bone disease is thought to be direct and not only a consequence of the agent's antimyeloma properties, making it an attractive agent for further investigation, as it may combine potent antimyeloma activity with beneficial effects on bone. However, the clinical implication of these effects requires prospective studies with specific clinical end points.
Introduction
Myeloma bone disease is the result of increased destruction of bone that cannot be compensated for by new bone formation. Approximately 80% of patients with multiple myeloma (MM) develop skeletal complications including bone pain, osteolytic lesions, pathologic fractures, and hypercalcemia.1 Osteolytic bone destruction is the most debilitating manifestation of MM and has a severe impact on patients' quality of life. Moreover, myeloma-associated lytic bone lesions do not repair, even in patients who are disease free for years.2,3
Mechanisms of myeloma bone disease
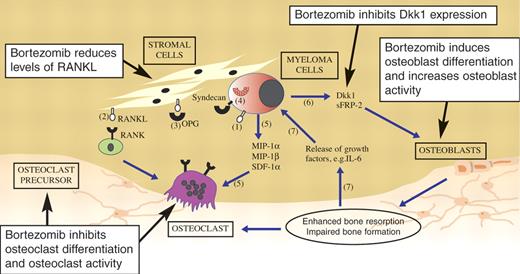
The pathophysiology of myeloma bone disease has been studied extensively over recent years. This has led to new insights into the complex interactions between myeloma cells and osteoclasts and osteoblasts. Histomorphometric studies have revealed that myeloma cells promote osteoclastic bone resorption and suppress osteoblast activity,4,5 thereby causing an imbalance between the processes of bone resorption and formation, which is so characteristic of myeloma bone disease6–9 (Figure 1).
Pathophysiology of myeloma bone disease and the suggested sites of action of bortezomib. (1) Myeloma cells produce RANKL and (2) cause stromal cells to overexpress RANKL. Bortezomib reduces levels of RANKL. (3) OPG is the soluble RANKL antagonist. (4) Myeloma cells inhibit OPG production and also bind circulating OPG by syndecan-1, thus facilitating its internalization and degradation. Bortezomib restores the RANKL/OPG balance. (5) Myeloma cells express MIP-1α, MIP-1β, and SDF-1α, which recruit osteoclast precursors and enhance osteoclast activity. (6) Myeloma cells secrete Dkk1 and sFRP-2, which inhibit osteoblast differentiation and function. Bortezomib inhibits Dkk1 expression and increases osteoblast differentiation and activity. (7) The resulting enhanced bone resorption releases cytokines and growth factors that in turn promote myeloma cell proliferation and survival. Adapted from Heider et al7 with permission.
Pathophysiology of myeloma bone disease and the suggested sites of action of bortezomib. (1) Myeloma cells produce RANKL and (2) cause stromal cells to overexpress RANKL. Bortezomib reduces levels of RANKL. (3) OPG is the soluble RANKL antagonist. (4) Myeloma cells inhibit OPG production and also bind circulating OPG by syndecan-1, thus facilitating its internalization and degradation. Bortezomib restores the RANKL/OPG balance. (5) Myeloma cells express MIP-1α, MIP-1β, and SDF-1α, which recruit osteoclast precursors and enhance osteoclast activity. (6) Myeloma cells secrete Dkk1 and sFRP-2, which inhibit osteoblast differentiation and function. Bortezomib inhibits Dkk1 expression and increases osteoblast differentiation and activity. (7) The resulting enhanced bone resorption releases cytokines and growth factors that in turn promote myeloma cell proliferation and survival. Adapted from Heider et al7 with permission.
The molecular mechanisms responsible for the increased osteoclastic bone resorption are also becoming clear. Under normal circumstances, receptor activator of nuclear factor-kappa B ligand (RANKL) and its decoy receptor osteoprotegerin (OPG) regulate osteoclast formation, activity, and bone resorption. Myeloma cells disrupt the balance between RANKL and OPG by increasing the expression of RANKL and decreasing the expression of OPG.10–12 The resulting increase in RANKL favors the formation and activation of osteoclasts, leading to increased bone resorption.10,11,13–15 Altering the balance in this system with OPG or soluble RANK constructs has been shown to prevent the development of myeloma bone disease.11,13,16 In addition to RANKL and OPG, macrophage inflammatory protein-1α (MIP-1α) and MIP-1β have been shown to be produced by myeloma cells and promote osteoclastic bone resorption.17–23 MIP-1α may act in a RANKL-dependent manner.21 Additional factors, including stromal cell-derived factor-1α (SDF-1α),24 interleukin 3 (IL-3),25 and hepatocyte growth factor,26 have also been implicated in regulating the increase in osteoclast formation or activity. The bone destruction brought about by the myeloma cells results in the release of cytokines and growth factors, either from osteoclasts themselves or present in bone matrix that may further promote myeloma cell growth and survival, thus establishing a cycle of dependence between the tumor cells and osteoclastic bone destruction.27
In addition to their stimulatory effect on osteoclasts, myeloma cells have been shown to suppress bone formation.4,5 In vitro studies have confirmed that myeloma cells can inhibit the differentiation of osteoblast precursors and can induce apoptosis in mature osteoblasts.28–31 Although our understanding of the molecular mechanisms responsible for increased osteoclastic resorption has improved, our grasp of the molecular mechanisms responsible for the inhibition of bone formation is less clear. The Wingless-type (Wnt) signaling pathway is one pathway that has been shown to play a key role in osteoblast differentiation32 and has been implicated in osteoblast suppression in myeloma. Tian et al33 have shown that dickkopf-1 (Dkk1), an inhibitor of the Wnt signaling pathway, is secreted by myeloma cells and may inhibit osteoblast differentiation and activity in vitro. Dkk1 has also been found to be increased in the serum of patients with myeloma but not in patients with monoclonal gammopathy of undetermined significance (MGUS).33,34 However, these studies require independent confirmation, as not all investigators have seen that Dkk1 regulates bone formation in MM30 and been able to show that serum concentrations are increased. Soluble frizzle-related protein-2 (sFRP-2), another inhibitor of Wnt signaling, has also been implicated in suppression of bone formation in myeloma.35 Furthermore, other molecules, including IL-7 and IL-3, have been reported to be elevated in myeloma and block osteoblast differentiation either directly or indirectly in vitro.30,36 The precise role of each of these molecules has not been established and their role in vivo is often less clear; however, the result of these multiple interactions is the inhibition of osteoblast differentiation and reduced bone formation.
Current management of myeloma bone disease
Bisphosphonates are specific inhibitors of osteoclast activity and are the current mainstay of therapy for myeloma bone disease.37–39 Clinically, bisphosphonates reduce, but do not completely prevent, skeletal damage. Bisphosphonates inhibit osteoclast recruitment and maturation, prevent differentiation, and induce osteoclast apoptosis.40 Furthermore, antimyeloma activity of pamidronate and zoledronic acid has been suggested.41,42 However, these agents impact on osteoclast activity only and do not restore bone formation. Thus, new approaches to inhibiting osteoclastic resorption and preventing the inhibition of bone formation are still required to prevent the development of myeloma bone disease.
The ubiquitin-proteasome pathway and bone metabolism
The ubiquitin-proteasome pathway is the major intracellular mechanism for the degradation of proteins that are involved in a range of normal cellular processes including the control of the cell cycle, transcriptional activation, apoptosis, and cell signaling. Many of these biologic pathways are directly related to the development and progression of cancer and may also be directly involved in regulating bone turnover.43,44 In patients with active myeloma, serum proteasome concentrations are significantly elevated and reduced in responders to chemotherapy.45 Furthermore, circulating proteasome levels have been identified as an independent prognostic factor in patients with active MM,45 even though there is no evidence that there is any correlation between the inhibition of proteasome activity and a response to therapy.
Proteasome inhibition has been implicated in the regulation of bone metabolism through the reduction of RANKL-mediated osteoclast differentiation via the inhibition of nuclear factor-kappa B (NFκB) signaling. Binding of RANKL to RANK on the surface of osteoclast precursors induces NFκB activation, which leads to osteoclast differentiation and bone resorption. However, in the presence of proteasome inhibitors, IκB, the inhibitor of NFκB, which is normally degraded by the proteasome, remains bound to NFκB and prevents the activation of NFκB.46 Consequently, proteasome inhibition would be predicted to prevent bone resorption. In accordance with this hypothesis, Zavrski et al47 showed that treatment of osteoclast precursors with the proteasome inhibitors MG-132 and MG-262 inhibited RANKL-mediated osteoclast formation at nanomolar, subapoptotic concentrations. This reduction was accompanied by a reduction of the resorption capacity of osteoclasts. Furthermore, osteoclasts treated with proteasome inhibitors exhibited a dose-dependent reduction of NFκB activation, which strongly correlated with the diminished osteoclast differentiation.47 Thus, proteasome inhibition may inhibit osteoclastic bone resorption directly.
In addition to modifying bone resorption, Garrett et al48 found that the ubiquitin-proteasome pathway is also involved in the regulation of osteoblast differentiation and bone formation. Proteasome inhibitors, such as epoxomicin, proteasome inhibitor-1 (PS-1), and lactacystin, at low nanomolar concentrations, were shown to promote bone formation and increase osteoblast numbers in a dose-dependent manner in bone organ culture systems. In that study, only proteasome inhibitors and not inhibitors of nonproteasomal proteases or other inhibitors of NF-κB showed this beneficial effect on bone formation in vitro. But, more importantly, 5 days of treatment with the proteasome inhibitors epoxomicin or PS-1 promoted an increase in bone formation rate and new bone formation in vivo. The effect of proteasome inhibitors on bone formation was reported to be mediated by increased bone morphogenetic protein-2 (BMP-2) expression in osteoblasts. BMPs act predominantly on osteoblasts and promote their differentiation in an autocrine manner.48
These data strongly suggest that the proteasome system may play a key role in regulating bone remodeling by inhibiting osteoclast formation and stimulating new bone formation, and therefore proteasome inhibitors have been tested in both preclinical and clinical settings for their potential effect on bone metabolism in myeloma-related bone disease.
Proteasome inhibition and myeloma-related bone disease
Bortezomib is the first-in-class potent and reversible inhibitor of the proteasome that has demonstrated efficacy in the treatment of both relapsed/refractory and newly diagnosed MM.49–51 In multiple myeloma, bortezomib has been approved for the treatment of patients who have received 1 prior therapy and is being investigated in the front-line setting as a single agent or in combination with other agents. Since proteasome inhibition has been shown to regulate bone turnover, an increasing number of studies have examined the effect of bortezomib in myeloma-related bone disease. These data are discussed in “Preclinical studies” and “Clinical studies.”
Preclinical studies
Effect of bortezomib on bone formation
Oyajobi et al52 first reported that bortezomib could stimulate new bone formation in neonatal mouse calvariae organ culture. The increased bone formation was associated with an inhibition of the Wnt signaling antagonist Dkk1 in both stromal cell lines and in the organ culture system.52 Giuliani et al53 reported that bortezomib could induce osteoblast differentiation in human mesenchymal cells and this was associated with increased Runx2/cbfa1 expression but not Wnt signaling. In contrast, bortezomib was shown not to effect the proliferation of more mature osteoblast-like cells or alter levels of apoptosis. Furthermore, expression of Runx2/Cba1 was not affected in these cells.53 Mukherjee et al54 demonstrated that bortezomib promoted an increase in the size of osteoblastic colony-forming units but had no effect on their number. These cells were CD45−/CD51+, expressed collagen type I and alkaline phosphatase (ALP), and formed bone nodules, suggesting that they were of osteoblastic lineage. Mice treated with bortezomib also had increased numbers of bone marrow CD45−/CD51+ cells.54 These data suggest that bortezomib may promote bone formation by stimulating progenitor proliferation and osteoblast differentiation rather than mature cell activity.
The effect of bortezomib has also been examined in vivo in the SCID-rab model of myeloma.55 Treatment of nonmyeloma-bearing mice with bortezomib (0.5 mg/kg twice a week) resulted in an increase in bone mineral density (BMD). In myeloma-bearing mice that were responsive to treatment, there was also an increase in BMD (20% ± 14%); however, this was not seen in nonresponsive mice, and BMD decreased (13% ± 12%). The increase in BMD was not seen in dexamethasone-responsive mice and was associated with increased numbers of osteocalcin (OC)-expressing osteoblasts and reduced numbers of tartrate-resistant acid phosphatase (TRACP)–expressing osteoclasts.55 Separating the direct effect of bortezomib on osteoblast differentiation and indirect effects via the inhibition of tumor growth in vivo is difficult; however, it does highlight a potential interdependence between myeloma growth and osteoblasts.
Effect of bortezomib on bone resorption
In addition to promoting bone formation, bortezomib has been reported to affect osteoclast differentiation and function. Oyajobi et al52 reported that bortezomib could prevent IL-1-stimulated bone resorption in a murine system. Furthermore, Kawanabe et al56 demonstrated that bortezomib could inhibit osteoclast formation in murine bone marrow cultures in a dose-dependent manner. In addition, bortezomib was shown to reduce resorption pit formation, which suggests it was able to inhibit both osteoclast formation as well as bone resorption.56 These data are supported by recent studies showing that bortezomib also inhibits the formation of human osteoclasts derived from either peripheral blood mononuclear cells or purified CD14+ precursors,57,58 and this was associated with a down-regulation of NFκB activity and an inhibition of the p38 mitogen-activated protein kinase pathway.55,57 Furthermore, bortezomib has been shown to inhibit osteoclast formation synergistically with the histone deacetylase (HDAC) inhibitor PXD101.59 This followed a previous observation that HDAC inhibitors block osteoclastogenesis60 and was based on the hypothesis that simultaneous targeting of different pathways may constitute a more effective approach for the suppression of osteoclast formation and the reduction of subsequent bone resorption.
In vivo, bortezomib treatment of SCID-rab mice bearing myeloma was associated with a reduction in osteoclast number.55 In a number of these studies, bortezomib treatment reduced the resorptive activity of mature human osteoclasts,57,58,61 although these effects were reported to be transient.61 However, separating the direct effect of bortezomib on osteoclast numbers and indirect effects via the inhibition of myeloma cells in vivo is difficult. In this point, we have to mention that the concentrations of bortezomib used in these studies were typically less than that required to induce tumor cell apoptosis.
Clinical studies
Bortezomib increases osteoblast activity
An increasing number of studies are reporting the effects of bortezomib on bone formation in the clinical setting, confirming preclinical observations.
One of the first indications that bortezomib may have a positive effect on bone formation came from Zangari et al,62 who observed a significant increase in serum ALP levels in a patient who responded to treatment with bortezomib. Another case report was published by Shimazaki et al,63 who treated a patient with refractory MM with bortezomib, dexamethasone, and incadronate. The response to treatment was accompanied by increases in serum ALP level as well as bone-specific ALP (bALP), suggesting that bortezomib may have a direct effect on osteoblastic activity.
Elevations in ALP levels were also noted in patients responding to the combination of bortezomib, thalidomide, and dexamethasone but not in nonresponders to this treatment.64 These observations prompted the analysis of ALP levels in 2 large bortezomib trials, Study of Uncontrolled Multiple Myeloma managed with Proteasome Inhibition Therapy (SUMMIT) and Assessment of Proteasome Inhibition for Extending Remissions (APEX).62 A significant increase in ALP levels from baseline was observed in patients responding to bortezomib (complete responses [CRs] and partial responses [PRs]) within 3 cycles of therapy. A parallel increase in bALP and parathyroid hormone levels was noted and suggested that the response to bortezomib was associated with osteoblast activation. On the other hand, in patients responding to dexamethasone, no increase in ALP level was observed, possibly due to the toxic effect of dexamethasone on osteoblasts.
A more detailed analysis of data from the phase-3 APEX trial assessed the relationship between quantitative total ALP changes and response, and with time to progression during therapy with bortezomib. The analysis found that a 25% increase in total ALP levels at 6 weeks was strongly associated with patients achieving a response (CR + PR) and longer time to myeloma progression.65,66 The investigators concluded that markers of osteoblast activation may be useful in predicting response to bortezomib and duration of response. The results also suggest that bone anabolism may affect myeloma growth. Interestingly, the antimyeloma effect of osteoblasts was recently demonstrated in vitro and in vivo by Yaccoby et al, 67 who concluded that treatment with bone anabolic agents may benefit patients with MM.
Osteoblast stimulation with bortezomib was also observed by Heider et al,68 who measured changes in serum bALP and OC levels in patients receiving bortezomib ± dexamethasone (n = 25) and in a control group of patients who received adriamycin/dexamethasone-, melphalan/prednisone-, or thalidomide-containing regimens (n = 58). Significant increases in bALP and OC levels following bortezomib treatment were observed (Table 1). Interestingly, increases in markers of osteoblast activity were seen in responders and nonresponders, irrespective of whether dexamethasone was included in the treatment regimen. Conversely, in the control group of patients who did not receive bortezomib, no increase in osteoblast markers was seen, suggesting that the effect on osteoblasts is mainly due to the proteasome inhibitor.
Terpos et al69 also showed that bortezomib significantly increased serum levels of bALP and OC in 34 patients with relapsed MM (Table 2). Patients who achieved a CR or very good PR (VGPR) after 4 cycles of bortezomib had greater elevations of bALP levels than those not achieving a CR or VGPR. Interestingly, 75% of nonresponders also had an increase in bALP levels following 4 cycles of bortezomib treatment. The increase in bone formation markers was accompanied by a reduction in Dkk1 serum levels, which was similar among responders and nonresponders after bortezomib therapy.69 Although no healing of lytic bone lesions was observed, even in patients who achieved a CR, longer follow-up or prolonged bortezomib therapy may be needed to demonstrate a radiographic improvement after increased bone formation.69 Finally, Giuliani et al53 have recently reported clinical evidence for the role of bortezomib in increasing osteoblast differentiation. These investigators treated 21 patients with relapsed/refractory MM with single-agent bortezomib and analyzed bone marrow biopsies. Significant increases in the number of osteoblastic cells/mm2 of bone tissue and Runx2/Cbfa1-positive osteoblastic cells were found in responding patients but not in those who did not respond. Although it cannot be excluded that the increase in osteoblast differentiation and numbers and the subsequent increase in bone formation could be due to the reduction in myeloma burden, it should be noted that this beneficial effect has not previously been observed with other antimyeloma regimens that effectively reduce tumor burden. It is likely that bortezomib stimulates bone formation by both directly inducing osteoblast function and indirectly reducing myeloma cell burden. However, when bortezomib is combined with other antimyeloma agents such as thalidomide and melphalan, it appears to lose its beneficial effect on osteoblasts. Terpos et al70 have recently reported that the VMDT regimen (combination of bortezomib with melphalan, dexamethasone, and intermittent thalidomide) produces no increase in bone formation markers (bALP and OC) although it reduces Dkk1 levels and tumor burden. The reason for the lack of effect is unclear and the study is difficult to interpret due to the presence of 4 agents. However, dexamethasone, an important component of MM therapy, is known to induce osteoporosis by reducing the lifespan of osteoblasts.71 Recent studies have shown that exposing osteoblasts to dexamethasone results in increased Dkk1 expression,72 indicating that the agent may inhibit osteoblast differentiation through a mechanism involving up-regulation of Dkk1, thereby blocking bone formation. Dexamethasone may thus inhibit the positive effect of bortezomib on osteoblasts in MM. Indeed, Heider et al68 found a lower increase in bALP levels in patients who received the combination of bortezomib with dexamethasone compared with patients who received bortezomib alone. Such studies highlight the requirement for single-agent studies investigating the effect of proteasome inhibition on bone.
Bortezomib inhibits osteoclast activity
Results from a prospective study on markers of bone resorption by Peles et al73 suggest an inhibitory effect of bortezomib on osteoclastic bone resorption in patients receiving the agent as consolidation treatment following transplantation. Patients (n = 33) were treated with bortezomib 1.3 mg/m2 once weekly for 4 of every 5 weeks, 90 to 120 days after transplantation, for 6 cycles. Patients did not receive bisphosphonates from 42 days prior to stem cell collection until cycle 3 of bortezomib therapy. Following 2 cycles of consolidation therapy, a 32% reduction in urinary N-terminal cross-linking telopeptide of collagen type-I (NTX) excretion, a highly specific marker of bone resorption, was observed. This reduction suggests that bortezomib has an inhibitory effect on osteoclast activity and bone resorption, which was seen even in patients at a plateau phase of their disease. Interestingly, the only patient with an increase in NTX of more than 30% was also the only patient with evidence of disease progression. However, contrary to recent reports on the positive effect of bortezomib on osteoblastic bone formation, a decline in OC levels was observed in this study.73
Furthermore, Terpos et al69 have recently reported in 34 patients with relapsed myeloma that bortezomib administration, at the standard dosage, resulted in a significant reduction in serum RANKL levels, after 4 and 8 cycles of therapy, with concomitant reduction in osteoclast function and bone resorption, as assessed by the serum levels of TRACP type-5b (TRACP-5b) and C-terminal cross-linking telopeptide of collagen type-I (CTX), respectively (Table 2). The reduction in osteoclast function and bone resorption occurred irrespective of response to therapy in this study.69
At this point, it is crucial to mention that different effective antimyeloma regimens in combination with bisphosphonates can also reduce bone resorption through the reduction of tumor burden and the inhibition of osteoclast function in MM.74–77 Randomized trials are needed to explore if bortezomib alone or in combination with other agents, including bisphosphonates, can inhibit bone resorption more effectively.
Conclusions
With approximately 70% to 80% of patients with MM developing skeletal complications, bone disease is a major problem in the management of this malignancy. Increased understanding of the pathophysiology of bone disease is helping to identify new therapeutic targets for this debilitating complication of MM. The ubiquitin-proteasome pathway is one system that has been implicated in bone remodeling and may play a key role in regulating both the growth and survival of myeloma cells, as well as modulating the development of myeloma bone disease.
Bortezomib, the first-in-class proteasome inhibitor, has multiple targets in MM. The agent is effective against myeloma cells and is now being investigated for its positive effect on myeloma bone disease. The data available to date strongly suggest that bortezomib is able to regulate bone remodeling by inhibiting osteoclast differentiation and resorption and promoting bone formation. Separating the potential direct effect of bortezomib on bone metabolism from an indirect effect on bones due to the reduction of tumor burden is very difficult. However, the effect of bortezomib on bone formation is notable and distinguishes this agent from bisphosphonates and other myeloma treatments that act only to inhibit bone resorption. Increased bone formation will not only reduce skeletal complications but may also help to control MM progression. Therefore, bortezomib may be the first agent that combines potent antimyeloma activity with potential beneficial effects on bone. However, to date, evidence of the effect of bortezomib on clinical end points specific to bone, such as skeletal-related events (SREs) and BMD, is limited, possibly as a result of relatively short follow-up periods. It is therefore essential to design prospective trials that investigate end points related to bone formation. Initially, it would be important to focus on studies with single-agent bortezomib to clearly establish the effect of the agent by itself on BMD and SREs. Maintenance therapy would be a useful setting to investigate this single-agent activity. An increase in BMD in patients receiving bortezomib maintenance treatment would suggest that the effect of bortezomib on bone is mainly via a direct effect on bone and not only due to a reduction in tumor burden. The results of such studies are eagerly anticipated.
Note added in proof.
After completion of this review, von Metzler et al78 published the first study showing that bortezomib inhibits human osteoclast differentiation, activation, and resorptional activity in a dose- and time-dependent manner.
Acknowledgments
O.S. was supported by the Deutsche Forschungsgemeinschaft (DFG; Klinische Forschergruppe KFO 105).
Authorship
Contribution: All authors have participated in the acquisition of data; E.T. and O.S. participated in the analysis and interpretation of preclinical and clinical data; E.T. and M.-A.D. wrote the clinical part of this review; and E.T., P.C., and O.S. wrote the section on preclinical studies. All authors have given final approval of the version to be published.
Conflict-of-interest disclosure: All authors have participated in Advisory Boards of Janssen-Cilag with honoraria. E.T. has been supported with an unrestricted educational grant by Janssen-Cilag.
Correspondence: Evangelos Terpos, Department of Hematology and Medical Research, 251 General Airforce Hospital, 3 Kanellopoulou Street, GR-11525, Athens, Greece; e-mail: e.terpos@imperial.ac.uk; eterpos@hotmail.com.