Abstract
Donor dendritic cells (DCs) play a pivotal role in the induction of immunity and tolerance after peripheral blood stem cell transplantation (PBSCT). Treatment of healthy donors with granulocyte-colony stimulating factor (G-CSF) increases the numbers of tolerogenic DCs and T cells among mobilized blood leukocytes in the graft. SlanDCs (6-sulfo LacNAc+ DCs), a major source of IL-12 and TNF-α in blood, have not been studied in this respect. Here, we demonstrate that slanDCs (14.9 × 106/L to 64.0 × 106/L) are efficiently mobilized by G-CSF and retain their capacity to produce IL-12 and TNF-α at high levels. Furthermore, G-CSF–mobilized slanDCs programmed the differentiation of Th1 cells and displayed a particularly strong capacity to stimulate the proliferation of naive allogeneic T cells. Thus, slanDCs transfused into recipients of allogeneic peripheral blood stem cell (PBSC) transplants are functionally fully capable and may be critical in supporting graft-versus-host disease as well as graft-versus-leukemia effects.
Introduction
Granulocyte-colony stimulating factor (G-CSF) is widely used to mobilize hematopoietic stem cells for allogeneic peripheral blood stem cell transplantation (PBSCT).1,2 Graft-versus-host disease (GVHD) leads to significant morbidity and mortality,3,4 and therefore remains a major complication of PBSCT. Several studies have indicated a tolerogenic effect of G-CSF. In T cells, G-CSF has been shown to directly inhibit interferon-γ (IFN-γ) production, to increase interleukin-4 (IL-4) production,5,6 and to induce regulatory T cells.7 G-CSF also mobilizes tolerogenic CD14+ cells expressing cell surface IL-10.8,9 So far, G-CSF has been shown to selectively mobilize plasmacytoid dendritic cells (pDCs) that induce T cells to produce high levels of IL-4 and IL-10, but low levels of IFN-γ.10,11
The in vivo effects of G-CSF on the large population (1.2% of peripheral blood mononuclear cells [PBMCs]) of proinflammatory 6-sulfoLacNAc expressing DCs, now called slanDCs, have not been studied so far. SlanDCs are potent inducers of primary T-cell responses in vitro12 and have recently been described as the main producers of tumor-necrosis factor α (TNF-α)12 and notably of IL-12 after stimulation with lipopolysaccharide (LPS), R848, or CD40 ligand.13 Given their high proinflammatory potential, these cells might play a crucial role in the immune balance after allogeneic PBSCT.
Materials and methods
This study was approved by the institutional review board of Technische Universität Dresden. Peripheral blood mononuclear cells (PBMCs) were prepared from paired blood samples obtained with the informed consent (in accordance with the Declaration of Helsinki) of healthy peripheral blood stem cell (PBSC) donors before and after receiving G-CSF (5 days, 7.5 μg/kg per day kenograstim; Chugai, Tokyo, Japan). The percentage of DC subsets was determined by flow cytometry as described previously,12 and in parallel the white blood cell count was determined (Sysmex XE 2100; Sysmex, Hamburg, Germany). The absolute numbers of the DC subtypes were calculated from the absolute PBMC count, multiplied by the percentage of each subpopulation determined by flow cytometry.
Cell surface staining, flow cytometry, and gating for phenotypic analysis were conducted as formerly described.12
SlanDCs and naive CD4+CD45RA+ cord blood T cells (purity > 95% and > 98%, respectively) were isolated by magnetic cell sorting (Miltenyi Biotech, Bergisch-Gladbach, Germany) as previously described.12 T cells were cryopreserved in human AB serum (C.C. Pro Neustadt, Germany) containing dimethyl sulfoxide in 2 vials. At the time of thawing, they were washed with PBS twice and resuspended in RPMI media. This allowed coculture of T cells from the same cord blood donor with slanDCs obtained before and after treatment with G-CSF.
The cell culture, the stimulation with LPS or LPS and IFN-γ, the intracellular cytokine staining, as well as the determination of T-cell stimulatory capacity of slanDCs were done exactly as described recently.12,13
For T-cell programming,13 cocultures of slanDCs and T cells (1:10) were stimulated with 100 ng/mL LPS after 6 hours and restimulated with PMA and ionomycin on day 10 of coculture, and levels of IFN-γ and IL-4 were measured by enzyme-linked immunosorbent assay (ELISA) in cell-free supernatants harvested after 24 hours.
Statistical analysis was performed using paired t tests.
Results and discussion
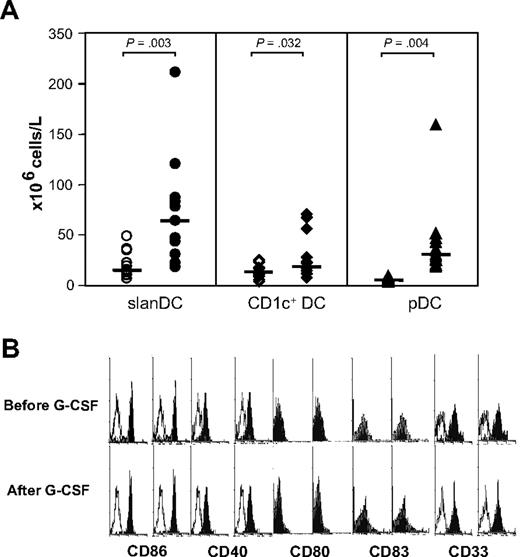
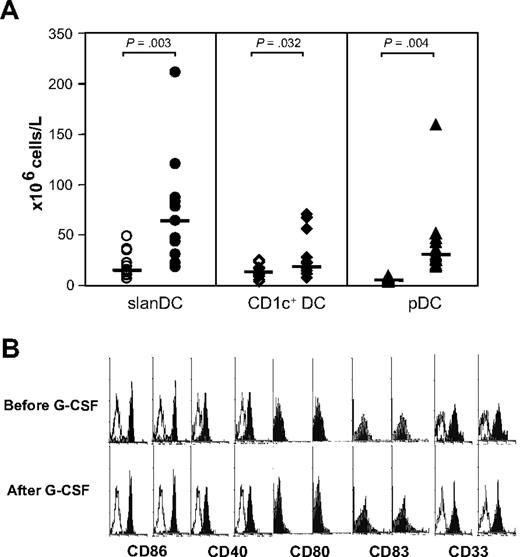
To determine the mobilizing effect of G-CSF on slanDCs, we studied PBMCs from healthy donors prior to and on day 5 of receiving G-CSF (n = 13). The flow cytometric analysis revealed a significant increase in the absolute number of slanDCs from 14.9 × 106/L (range, 7.4-49.2 × 106/L) to 64.0 × 106/L (range, 19.0-212.1 × 106/L) (P = .003) after treatment. Median CD1c+ DC counts amounted to 12.1 × 106/L (range, 3.3-23.3 × 106/L) before G-CSF and to 17.4 × 106/L (range, 6.4-69.9 × 106/L) (P = .032) after G-CSF. As reported by others, pDCs showed a strong increase.10 They increased 8.4-fold, from 3.4 × 106/L (range, 1.5-7.7 × 106/L) to 28.6 × 106/L (range, 16.4-157.2 × 106/L) (P = .004) (Figure 1A). In absolute numbers, the frequency of pDCs and CD1c+ DCs in the blood remained low. After G-CSF, slanDC counts were 2.2-fold higher than pDCs and 3.7-fold higher than CD1c+ DCs. The expression of costimulatory molecules (CD86, CD40, CD80), the maturation marker CD83, and the myeloid marker CD33 remained unchanged when comparing slanDCs before and after G-CSF administration (Figure 1B).
SlanDCs are mobilized by G-CSF and display an unaltered phenotype. Peripheral blood samples were collected from the same donors before and after G-CSF treatment. (A) Absolute cell counts of slanDCs (M-DC8+), CD1c+ DCs (lin−, HLA-DR+, CD11c+), and pDCs (lin−, HLA-DR+, CD11c−) were determined as described in “Materials and methods” (n = 13). Individual values and the median are shown. P values were determined using paired t tests. (B) The phenotypic analysis of slanDCs before and after G-CSF administration is compared. Results of one representative donor are shown (n = 5). Staining of PBMCs and gating were performed as described.12,13
SlanDCs are mobilized by G-CSF and display an unaltered phenotype. Peripheral blood samples were collected from the same donors before and after G-CSF treatment. (A) Absolute cell counts of slanDCs (M-DC8+), CD1c+ DCs (lin−, HLA-DR+, CD11c+), and pDCs (lin−, HLA-DR+, CD11c−) were determined as described in “Materials and methods” (n = 13). Individual values and the median are shown. P values were determined using paired t tests. (B) The phenotypic analysis of slanDCs before and after G-CSF administration is compared. Results of one representative donor are shown (n = 5). Staining of PBMCs and gating were performed as described.12,13
We have shown recently that slanDCs stand out by their high-level TNF-α and IL-12 production, leading to a strong capacity to program Th1 cells.12,13 In addition, we demonstrated a high frequency of slanDCs in areas of Th1-dominated inflammatory reactions, such as rheumatoid arthritis.13 Given the increased number of slanDCs in PBSC grafts, we asked whether G-CSF–mobilized slanDCs retained their proinflammatory capacity or were programmed for the induction of tolerance as described for monocytes.9
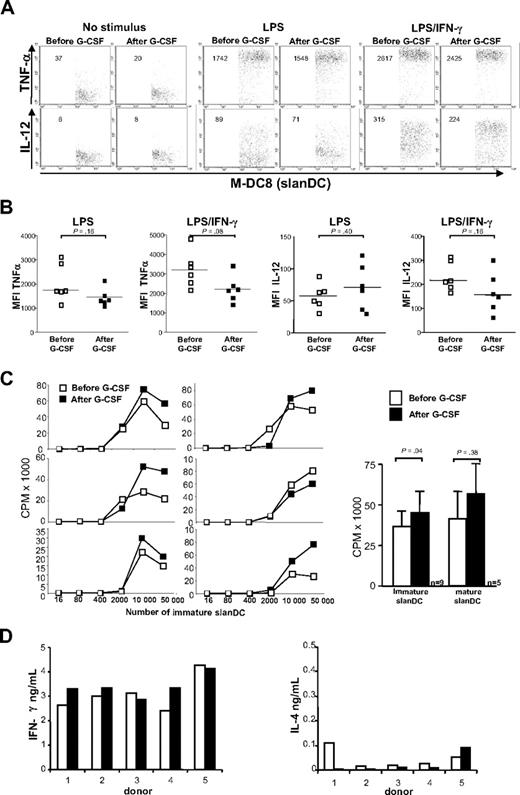
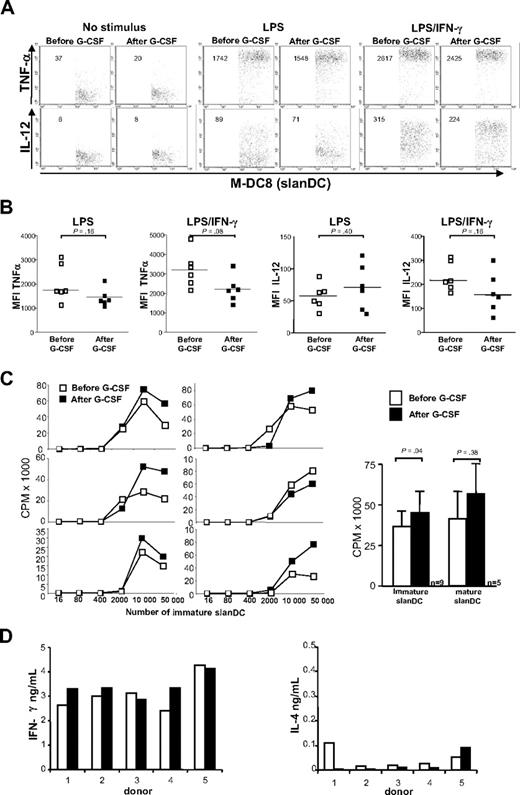
We therefore studied the production of TNF-α and IL-12p40/p70 on the single cell level by intracellular cytokine staining of PBMCs stimulated with the TLR-4 ligand LPS alone or with LPS and IFN-γ. The paired analysis of 6 donors before and after G-CSF treatment revealed small but not statistically relevant changes in the production of TNF-α and IL-12 (Figure 2A,B).
G-CSF–mobilized slanDCs retain their proinflammatory capacity. (A) Freshly purified PBMCs before and on day 5 of G-CSF treatment were stimulated as indicated. Intracellular cytokine staining was performed 18 hours after culture in the presence of brefeldin A.12,13 One representative donor is shown. The mean fluorescence intensity (MFI) is indicated for each dot plot. (B) MFI results of 6 donors. Each symbol represents a single sample. Horizontal lines in each series represent median values (n = 6). (C) SlanDCs were isolated from PBSC donors before and after G-CSF treatment, using immunomagnetic beads. SlanDCs of each donor were incubated with identical naive CD4+CD45RA+ cord blood cells at both time points. Graded numbers of slanDCs were cocultured with 105 naive T cells in triplicate for 5 days, and cultures were pulsed with 3H-thymidine for the last 16 hours. SlanDCs were added to the culture, either freshly isolated (immature) or after 6 hours of preculture (mature). In the left panel, results of 6 donors are shown. The right panel shows the T-cell stimulatory capacity of immature and mature slanDCs cultured at a ratio of 1:10 with cord blood T cells. Data are presented as mean counts per minute (cpm ± SEM). (D) Blood was drawn from 5 PBSC donors prior to and on day 5 of G-CSF therapy. SlanDCs were isolated and cocultured with allogeneic naive T cells again at a ratio of 1:10. Cells were incubated in the presence of LPS for 10 days. T cells were restimulated with PMA and ionomycin on day 10 of coculture. Supernatants were harvested after 24 hours and levels of secreted IFN-γ and IL-4 were measured by ELISA. Values are indicated for each individual donor before and after G-CSF (n = 5).
G-CSF–mobilized slanDCs retain their proinflammatory capacity. (A) Freshly purified PBMCs before and on day 5 of G-CSF treatment were stimulated as indicated. Intracellular cytokine staining was performed 18 hours after culture in the presence of brefeldin A.12,13 One representative donor is shown. The mean fluorescence intensity (MFI) is indicated for each dot plot. (B) MFI results of 6 donors. Each symbol represents a single sample. Horizontal lines in each series represent median values (n = 6). (C) SlanDCs were isolated from PBSC donors before and after G-CSF treatment, using immunomagnetic beads. SlanDCs of each donor were incubated with identical naive CD4+CD45RA+ cord blood cells at both time points. Graded numbers of slanDCs were cocultured with 105 naive T cells in triplicate for 5 days, and cultures were pulsed with 3H-thymidine for the last 16 hours. SlanDCs were added to the culture, either freshly isolated (immature) or after 6 hours of preculture (mature). In the left panel, results of 6 donors are shown. The right panel shows the T-cell stimulatory capacity of immature and mature slanDCs cultured at a ratio of 1:10 with cord blood T cells. Data are presented as mean counts per minute (cpm ± SEM). (D) Blood was drawn from 5 PBSC donors prior to and on day 5 of G-CSF therapy. SlanDCs were isolated and cocultured with allogeneic naive T cells again at a ratio of 1:10. Cells were incubated in the presence of LPS for 10 days. T cells were restimulated with PMA and ionomycin on day 10 of coculture. Supernatants were harvested after 24 hours and levels of secreted IFN-γ and IL-4 were measured by ELISA. Values are indicated for each individual donor before and after G-CSF (n = 5).
Notably, we observed that after G-CSF treatment of the donors, immature slanDCs have a slightly enhanced capacity to stimulate the proliferation of allogeneic naive CD4+CD45RA+ cord blood T cells (Figure 2C). Furthermore, we documented that G-CSF–mobilized slanDCs continued to program naive cord blood T cells for a strong Th1-dominated immune response in the presence of LPS as evidenced by high levels of IFN-γ and low levels of IL-4 in cell-free supernatants (Figure 2D).
The high frequency and unaltered proinflammatory capacity of slanDCs in PBSC grafts shed new light on the immune balance after allogeneic PBSCT. Myeloid DCs are regarded as key players in the initiation of GVHD as well as in maintaining the graft-versus-leukemia reaction (GVL). In contrast, pDCs have been shown to induce T-cell tolerance, and therefore increased numbers of pDCs in PBSC grafts were thought to account10 for the unexpectedly low incidence of acute GVHD (aGVHD) observed in initial studies.14,15 However, a recently performed meta-analysis revealed a significant increase of grades 3 to 4 aGVHD after PBSCT compared with bone marrow transplantation (BMT).16 In addition, chronic GVHD is known to be significantly increased in PBSCT compared with BMT.16-18
According to current thinking, GVHD is triggered by the conditioning regimen. Mucosal damage induced by chemotherapy and irradiation allows microbial products such as LPS to enter the systemic circulation and to trigger the production of inflammatory cytokines such as TNF-α and IL-12, both of which are important mediators of GVHD.19-21 This early and high-level IL-12 production was shown to be crucial, as elevated IL-12p70 serum levels in the first month after PBSCT turned out to be a strong predictive factor for aGVHD development.22 However, elevated serum IL-12 levels may also enhance the GVL reaction, because they were shown to be associated with an improved relapse-free survival.23
Our findings provide evidence that, in addition to the tolerogenic effects of G-CSF described by others,5-11 proinflammatory slanDCs in PBSC grafts are increased in numbers and are functionally competent. Thus, grafts containing slanDCs that are infused directly after conditioning therapy can be important for the immediate inflammatory response and for stimulating indirect T-cell immune responses against host tissues resulting in GVHD. This adverse function of slanDCs may be directly addressed by purging slanDCs from PBSC grafts. In this case GVHD may be reduced, however, slanDCs originating from donor stem cells after successful engraftment may well be able to contribute to the GVL immune responses as our previous studies demonstrated effective priming of tumor-specific cytotoxic T cells in vitro and enhancement of the tumoricidal activity of natural killer (NK) cells by high-level IL-12–producing slanDCs.24
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Livia Schulze and Maria Böhme for expert technical assistance.
Authorship
Contribution: S.H.C.B. performed the experiments and drafted the paper (this work is part of S.H.C.B.'s doctoral thesis); K.H. coordinated the blood sampling and the recruitment of donors; M.B. and E.P.R. contributed to the design and the writing of the paper; M.M. contributed to the writing of the paper; K.S. designed the project, finalized the paper, and served as the thesis supervisor of S.H.C.B.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Knut Schäkel, Institute of Immunology and Department of Dermatology, Medical Faculty, Technische Universität Dresden, Fiedlerstr. 42, 01307 Dresden, Germany; e-mail: knut.schaekel@tu-dresden.de.