Chronic myeloid leukemia (CML), a hematopoietic stem-cell disorder, cannot be eradicated by conventional chemotherapy or the tyrosine kinase inhibitor imatinib mesylate (IM). To target CML stem/progenitor cells, we investigated BMS-214662, a cytotoxic farnesyltransferase inhibitor, previously reported to kill nonproliferating tumor cells. IM or dasatinib alone reversibly arrested proliferation of CML stem/progenitor cells without inducing apoptosis. In contrast, BMS-214662, alone or in combination with IM or dasatinib, potently induced apoptosis of both proliferating and quiescent CML stem/progenitor cells with less than 1% recovery of Philadelphia-positive long-term culture-initiating cells. Normal stem/progenitor cells were relatively spared by BMS-214662, suggesting selectivity for leukemic stem/progenitor cells. The ability to induce selective apoptosis of leukemic stem/progenitor cells was unique to BMS-214662 and not seen with a structurally similar agent BMS-225975. BMS-214662 was cytotoxic against CML blast crisis stem/progenitor cells, particularly in combination with a tyrosine kinase inhibitor and equally effective in cell lines harboring wild-type vs mutant BCR-ABL, including the T315I mutation. This is the first report of an agent with activity in resistant and blast crisis CML that selectively kills CML stem/progenitor cells through apoptosis and offers potential for eradication of chronic phase CML.
Introduction
Chronic myeloid leukemia (CML) is a clonal myeloproliferative disorder originating in a hematopoietic stem cell. It is characterized by the Philadelphia (Ph) chromosome,1 arising from a reciprocal translocation between the long arms of chromosomes 9 and 22, resulting in fusion of the BCR gene on chromosome 22 with the ABL oncogene on chromosome 9, with expression of its fusion gene product, BCR-ABL, a constitutively active tyrosine kinase.2 The deregulated BCR-ABL tyrosine kinase activity is essential for its transforming ability,3 resulting in phosphorylation of cellular substrates and activation of signal transduction pathways, including the RAS-ERK cascade, JAK-STAT, PI3-kinase, c-Myc, c-CBL, and CrKL, affecting cell growth, stromal interaction, and apoptosis.4,–6
Imatinib mesylate (IM; Novartis Pharma, Basel, Switzerland) is a tyrosine kinase inhibitor (TKI) active against ABL, c-KIT, and PDGFR, acting by competitive inhibition of adenosine triphosphate binding to the tyrosine kinase.7 Despite an impressive rate of durable complete cytogenetic response in chronic phase CML patients treated with IM,8 only a minority of patients achieve complete molecular remission.9 At least 2 mechanisms of resistance appear to account for residual disease in these patients: the innate insensitivity of primitive quiescent CML stem/progenitor cells, which greatly overexpress BCR-ABL, to IM10,11 and BCR-ABL kinase mutations,12 which are present before IM therapy in a subgroup of patients and result in IM resistance.13,14 However, there is currently no direct evidence that these resistance mechanisms, observed in vitro, are responsible for residual disease in IM-treated patients.
Two main strategies to overcome IM resistance have emerged. These are the development of second generation TKIs15,16 and the use of IM in drug combinations.17 Dasatinib (Sprycel, formerly BMS-354825; Bristol-Myers Squibb, Stamford, CT) is an oral, multitargeted inhibitor of BCR-ABL and SRC kinases, with greatly improved potency against wild-type (WT) BCR-ABL, capable of binding all known BCR-ABL kinase mutants resistant to IM except T315I.15 In our previous work, although dasatinib induced durable inhibition of BCR-ABL in primitive progenitor cells from CML patients compared with either IM or nilotinib, which were ineffective,11,18 none of these TKIs targeted the most primitive, quiescent CML stem/progenitor cells. Of a wide range of rational drug combinations,17 the only agent to synergize with IM against these cells was the cytostatic farnesyltransferase inhibitor (FTI) lonafarnib (Schering-Plough).17
FTIs inhibit oncogenic RAS and have entered clinical trials in solid tumors and acute leukemias.19,–21 However, the observed antitumor effects of FTIs are not solely the result of RAS inhibition22,23 ; they may also act by inhibiting farnesylation of other proteins.24,25 BMS-214662 is a cytotoxic FTI26 that produces potent tumor regression and curative responses in human tumor xenografts and transgenic tumor models and differs from other, cytostatic FTIs, including lonafarnib and tipifarnib, which have noncurative activity.22,27 In addition, BMS-214662 has been shown to preferentially kill nonproliferating cells28 and has antileukemic activity in acute myeloid leukemia (AML).20
We hypothesized that BMS-214662 might therefore target quiescent CML stem/progenitor cells and synergize with TKIs, which induce potent antiproliferative effects on CML stem/progenitor cells. We show that BMS-214662 selectively induces apoptosis of CML stem/progenitor cells, both in vitro and in vivo, and synergizes with IM or dasatinib to kill stem/progenitor cells reversibly arrested in G1.
Methods
Reagents
BMS-214662, BMS-225975 and dasatinib were obtained from Bristol-Myers Squibb. Stock solutions of 10 mg/mL in dimethyl sulfoxide (Sigma-Aldrich, St Louis, MO) were stored at −20°C. IM was obtained from Novartis Pharma. A 100-mM stock solution in sterile distilled water was stored at 4°C. Dilutions of these drugs in phosphate-buffered saline (PBS) were freshly prepared for each experiment.
Patient samples and isolation of CD34+ and CD34+38− cells
Fresh leukapheresis or peripheral blood samples were obtained with written informed consent and approval of North Glasgow University Hospital Division of NHS Greater Glasgow Institution Review Board from patients with newly diagnosed chronic phase CML (n = 11), blast crisis CML (n = 4), and normal donors of peripheral blood stem cells (n = 6). Samples were enriched for CD34+ cells using CliniMACS (Miltenyi Biotec, Auburn, CA) according to the manufacturer's instructions and cryopreserved in 10% (v/v) dimethyl sulfoxide in ALBA (4% [w/v] Human Albumin Solution, Scottish National Blood Transfusion Service). CD34+ CML and normal cells were simultaneously stained with CD34-APC and CD38-FITC (BD Biosciences, San Jose, CA) and sorted to isolate the CD34+38− subpopulation using a FACSAria (BD Biosciences).
Primary cell culture
CD34+ cells were cultured in serum-free medium (SFM) consisting of Iscove Modified Dulbecco Medium (Sigma-Aldrich) containing a serum substitute (bovine serum albumin, insulin, transferrin [BIT]; Stem Cell Technologies, Vancouver, BC), 0.1 μM 2-mercaptoethanol (Sigma-Aldrich), plus or minus a high concentration 5 growth factor (5GF) cocktail comprising 100 ng/mL Flt3-ligand, 100 ng/mL stem cell factor, and 20 ng/mL each of interleukin-3 (IL-3), IL-6 (all from Stem Cell Technologies) and granulocyte-colony stimulating factor (Chugai Pharma Europe, London, United Kingdom). Drug synergy for BMS-214662 with IM or dasatinib was assessed after 48 hours culture using total viable cell counts and the median-effect method of Chou and Talalay29 and analyzed using CalcuSyn software (Biosoft, Cambridge, United Kingdom).
Tracking of cell division using carboxyfluorescein diacetate succinimidyl diester staining
CD34+ cells were stained with 1 μM carboxyfluorescein diacetate succinimidyl diester (CFSE, Invitrogen, Carlsbad, CA) as described previously.30,–32 CFSE is an intracellular fluorescent stain, the intensity of which halves with each cell division. The CFSE+ CD34+ cells were cultured in the presence of different drug combinations. Total cell viability was assessed using trypan blue dye exclusion. Cells cultured in Colcemid (Invitrogen, 100 ng/mL), which arrests cell-cycle progression, were used to establish the CFSEmax quiescent cell population at all time points studied. Flow cytometric analysis was performed using the FACSCaliber (BD Biosciences). CFSE+ cells from each test condition were stained with anti-CD34-PE (BD PharMingen, San Diego, CA) and propidium iodide (PI, Sigma-Aldrich), which allows exclusion of dead cells. To assess the efficacy of each drug alone or in combination against primitive CML progenitor cells, the number of quiescent cells remaining at each time point was determined by measuring the percentage recovery of the starting number of viable (PI−) CD34+ cells in the CFSEmax quiescent subpopulation as described previously.10
Long-term culture-initiating cell assay
After culture for 72 hours in the presence of different drug treatments, CD34+ cells were set up in long-term culture-initiating cell (LTC-IC) assays as previously described.33 M2–10B4 cells and S1/S1 fibroblasts were established as feeder layers and then irradiated at 80 Gy. The cells remaining after culture were washed 3 times to remove all drug and then plated in duplicate on the irradiated feeder layers in Myelocult medium (Stem Cell Technologies). Cultures were maintained for 5 weeks with weekly half medium changes. After 5 weeks, cell counts were performed and 2.5 × 104 cells were transferred to colony forming cell assays and maintained in culture for an additional 2 weeks in Methocult medium (Stem Cell Technologies) before the colonies were counted.
Fluorescence in situ hybridization
Fluorescence in situ hybridization was performed with the LS1 BCR-ABL Dual Color, Dual Fusion translocation probe according to the manufacturer's instructions (Abbott Diagnostics, Abbott Park, IL) to determine the percentage of Ph+ cells before and after drug treatment.11
Assessment of apoptosis using caspase-3, TdT-mediated dUTP nick end labeling, and tetramethylrhodamine ethyl ester assays
To assess apoptosis, after 24, 48, 72, and 96 hours in each drug condition, an aliquot (2-3 × 105) of cells was removed for assessment of caspase-3 activity as described by Jorgensen et al.18 Cells were cultured in SFM plus or minus 5GF as indicated. For the TdT-mediated dUTP nick end labeling (TUNEL) assay, after 24 hours of treatment with BMS-214662, 50 μL reaction mixture (Cell Death Detection Kit; Roche Diagnostics, Indianapolis, IN) was added and the cells incubated at room temperature for 60 minutes. The cells were then washed twice in PBS and analyzed by fluorescent-activated cell sorter (FACS). Loss of membrane potential was measured after 24 hours of drug treatment. The cells were incubated with 50 μL tetramethylrhodamine ethyl ester (TMRE, Invitrogen) for 15 minutes and then analyzed by FACS.
Culture of Ba/F3 cell lines and cell proliferation assays
Parental Ba/F3 cells and Ba/F3 cells containing WT or kinase domain mutated BCR-ABL were maintained in RPMI (Sigma-Aldrich) containing 2% fetal calf serum, 1% glutamine (100 mM), and 1% penicillin-streptomycin (100 mM; all from Invitrogen), and supplemented with 10% conditioned medium from WEHI-3B cells. Five replicates of 2 × 104 Ba/F3 cells containing WT or kinase domain-mutated BCR-ABL were set up for each concentration of BMS-214662 and incubated for 48 hours. After 42 hours of culture, 0.2 μCi 3H-thymidine (Amersham Pharmacia Biotec GE Healthcare, Little Chalfont, United Kingdom) was added to each well. The cells were then harvested for beta counting using the MicroBeta TriLux (PerkinElmer Life and Analytical Sciences, Waltham, MA) according to the manufacturer's instructions.
Western blotting
A total of 2.5 × 106 cells/well were plated in 6-well plates. After 16 and 72 hours of drug treatment, the cells were lysed in Laemmli 2× sample buffer (Bio-Rad, Hercules, CA) and analyzed on SDS-PAGE. The proteins transferred to Hybond ECL nitrocellulose membranes (GE Healthcare) were blocked with 10% bovine serum albumin in TBS-T (20 mM Tris, pH 7.6, 13.7 mM NaCl, 0.1% Tween 20) for 2 hours. Incubation at 1:1000 dilution of primary antibodies (antirabbit actin, Bcl-2, Mcl-1, and Bim; all from Cell Signaling Technology, Danvers, MA) was carried out at 4°C overnight, and with secondary antibody (1:3000 antirabbit HRP, Cell Signaling) for 1 hour at room temperature and then developed with the ECL plus kit according to the manufacturers' instructions.
Statistical analysis
Statistical analyses were performed using the Student t test. A level of P less than or equal to .05 was taken to be statistically significant.
Results
BMS-214662 is more effective against Ph+ leukemic cells compared with normal cells, including primary CD34+ cells, and synergizes with TKIs
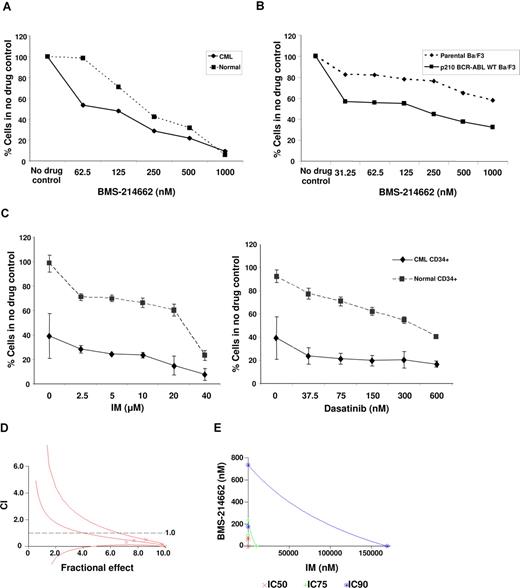
Primary human CD34+ normal and CML cells, parental Ba/F3 and Ba/F3 cells expressing WT p210BCR-ABL, were cultured for 48 hours with increasing concentrations of BMS-214662. The IC50 for BMS-214662 against CD34+ CML cells was approximately 62.5 nM (Figure 1A; assessed by total viable cell counts), which compared favorably with the IC50 against normal CD34+ cells, which was approaching 250 nM (Figure 1A). BMS-214662 at a concentration of 62.5 nM had minimal effect on normal CD34+ cells. In the murine Ba/F3 WT p210BCR-ABL cell line, BMS-214662 had an IC50 of approximately 125 nM (Figure 1B), whereas in parental Ba/F3 cells, the IC50 was not reached at a concentration of 1000 nM.
Efficacy of BMS-214662 against Ph+ leukemic cells versus Ph− non-leukemic cells. (A) Concentration response curve for BMS-214662 against CD34+ CML (n = 3) and normal cells (n = 3). The IC50 was approximately 62.5 nM in CD34+ CML cells and 250 nM in normal CD34+ cells as assessed by total viable cell counts. (B) Concentration response curve for BMS-214662 against parental and WT p210BCR-ABL Ba/F3 cell lines as assessed by total viable cell counts. The IC50 was approximately 125 nM against WT p210BCR-ABL Ba/F3 cells and not reached at a concentration of 1000 nM in parental Ba/F3 cells. Data represent the mean of 3 independent experiments. (C) Line graphs showing the results of synergism experiments with BMS-214662 62.5 nM in combination with IM (dose range 0-20 μM) or dasatinib (dose range 0-600 nM) in CD34+ normal and CML cells. The graph illustrates the cytotoxic effect of BMS-214662 62.5 nM as a single agent in CD34+ CML cells compared with normal CD34+ cells as assessed by total viable cell counts and also the added cytotoxicity of using BMS-214662 in combination with either IM or dasatinib. (D) CI plots calculated using CalcuSyn software for BMS-214662 and IM in an algebraic estimate. Combination of BMS-214662 plus IM indicated synergistic activity (CI values < 1) in CD34+ CML cells. CI values are represented by points below the dotted line. (E) A conservative isobologram for CD34+ CML cells indicated synergism between the 2 drugs.
Efficacy of BMS-214662 against Ph+ leukemic cells versus Ph− non-leukemic cells. (A) Concentration response curve for BMS-214662 against CD34+ CML (n = 3) and normal cells (n = 3). The IC50 was approximately 62.5 nM in CD34+ CML cells and 250 nM in normal CD34+ cells as assessed by total viable cell counts. (B) Concentration response curve for BMS-214662 against parental and WT p210BCR-ABL Ba/F3 cell lines as assessed by total viable cell counts. The IC50 was approximately 125 nM against WT p210BCR-ABL Ba/F3 cells and not reached at a concentration of 1000 nM in parental Ba/F3 cells. Data represent the mean of 3 independent experiments. (C) Line graphs showing the results of synergism experiments with BMS-214662 62.5 nM in combination with IM (dose range 0-20 μM) or dasatinib (dose range 0-600 nM) in CD34+ normal and CML cells. The graph illustrates the cytotoxic effect of BMS-214662 62.5 nM as a single agent in CD34+ CML cells compared with normal CD34+ cells as assessed by total viable cell counts and also the added cytotoxicity of using BMS-214662 in combination with either IM or dasatinib. (D) CI plots calculated using CalcuSyn software for BMS-214662 and IM in an algebraic estimate. Combination of BMS-214662 plus IM indicated synergistic activity (CI values < 1) in CD34+ CML cells. CI values are represented by points below the dotted line. (E) A conservative isobologram for CD34+ CML cells indicated synergism between the 2 drugs.
Synergy experiments were performed with BMS-214662 in combination with IM or dasatinib against CD34+ normal versus CML cells to determine whether there were synergistic or additive effects between BMS-214662 and the TKIs. CD34+ cells derived from CML patients and normal donors were treated with combinations of BMS-214662 and IM or dasatinib for 72 hours at the concentrations indicated in Figure S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article). When BMS-214662 was combined with the TKIs in CD34+ CML cells, we observed an increased concentration-dependent lethality, indicating synergistic activity between BMS-214662 and TKIs. Figure 1C shows results with BMS-214662 62.5 nM in combination with various concentrations of either IM or dasatinib in both normal and CML CD34+ cells. The combination of BMS-214662 (62.5 nM) with IM (2.5-20 μM) had a minimal effect on normal CD34+ cells (all > 60% survival). Similar results were obtained with dasatinib (37.5-150 nM). To confirm that BMS-214662 in combination with TKIs had a synergistic effect on CML CD34+ cells, the interaction between the drugs was analyzed using the CalcuSyn software program. Based on the Chou-Talalay method to calculate the Combination Index (CI),29 we generated an algebraic estimate and a conservative isobologram of various concentrations BMS-214662 and IM at the ratio 40:1 (drugs concentrations at the IC50, IC75, and IC90; Figure 1D,E). At doses ranging from 62.5 to 1000 nM of BMS-214662 and from 2.5 to 40 μM of IM, CI ranged from 0.8 to 0.2 (Figure 1D), indicating that this combination was highly synergistic. In the conservative isobologram, data points below the curve also indicated synergism (Figure 1E). Similar analyses were carried out for the combination of BMS-214662 and dasatinib, but synergism was only detected at higher drug concentrations. This may be because dasatinib is a stronger TKI than IM; therefore, higher concentrations of BMS-214662 are required to show synergism.
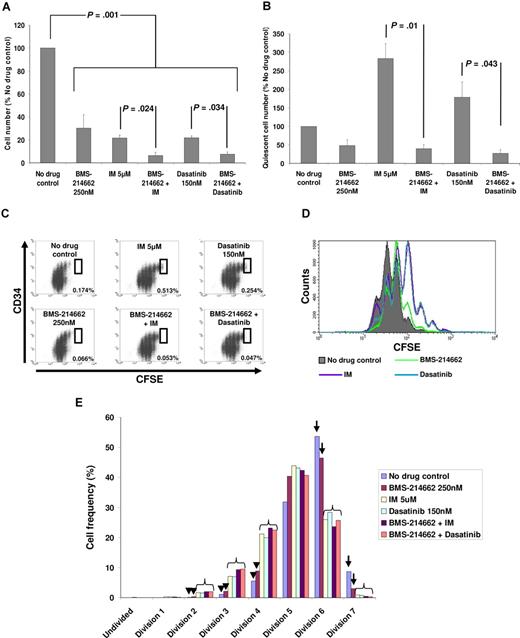
BMS-214662 enhances the cytotoxic effect of IM or dasatinib against the total CD34+ CML cell population
To assess the cytotoxic effect of BMS-214662 alone and in combination with IM or dasatinib, primary CD34+ CML cells were cultured in SFM supplemented with 5GF as follows: no drug control; BMS-214662; IM; BMS-214662 + IM; dasatinib and BMS-214662 + dasatinib. The concentration of BMS-214662 (250 nM) was chosen to be clinically achievable,21 and the concentrations of IM (5 μM) and dasatinib (150 nM) have been used in previous in vitro studies using a high concentration 5GF cocktail10,11 and are also clinically achievable at higher drug dose levels.34,35 After 3 and 6 days, there were significant reductions in total viable cells in the treatment arms compared with the no drug control (3 days, P = .04, data not shown; and 6 days, P = .001, Figure 2A). Importantly, by 6 days the combinations of BMS-214662 + IM and BMS-214662 + dasatinib showed increased cytotoxicity over either IM or dasatinib alone (P = .024 and P = .034, respectively).
Survival of total and quiescent CML cells in culture in the presence of drug combinations. Cells were cultured in SFM supplemented with growth factors. (A) Total viable cells (n = 4) after 6 days culture in the different treatment arms. Data are expressed as a percentage of the no drug control and data are represented as mean plus or minus SEM. (B) Total undivided CD34+ CFSEmax cells (n = 4) present after 6 days culture. In addition to P values shown, P = .023 and P = .005 for no drug control versus BMS-214662 + IM and BMS-214662 + dasatinib, respectively. Data are expressed as a percentage of the no drug control, and data are represented as mean plus or minus SEM. (C) Representative FACS dot plots showing the presence of a large quiescent CML stem/progenitor cell population (boxed region) in the IM and dasatinib arms, but not the BMS-214662-containing arms. The percentage value in the lower right corner of each plot represents the number of quiescent CML cells remaining at the end of the culture period expressed as a percentage of the starting CD34+ cell number. (D) Representative FACS histogram plot demonstrating the antiproliferative effect of dasatinib and IM compared with no drug control and BMS-214662. (E) Histogram highlighting the cell frequency for each cell division in each treatment arm. In the no drug control and BMS-214662 arms, there is a relative lack of cells in the early divisions (arrowhead ≤ 4 divisions) with increased numbers of cells in the later divisions ( arrow ≥ 6 divisions), compared with the TKI-containing arms, which tended to group together (bracket), with increased cells in the early divisions and fewer cells in later divisions. Data represent mean of 4 experiments.
Survival of total and quiescent CML cells in culture in the presence of drug combinations. Cells were cultured in SFM supplemented with growth factors. (A) Total viable cells (n = 4) after 6 days culture in the different treatment arms. Data are expressed as a percentage of the no drug control and data are represented as mean plus or minus SEM. (B) Total undivided CD34+ CFSEmax cells (n = 4) present after 6 days culture. In addition to P values shown, P = .023 and P = .005 for no drug control versus BMS-214662 + IM and BMS-214662 + dasatinib, respectively. Data are expressed as a percentage of the no drug control, and data are represented as mean plus or minus SEM. (C) Representative FACS dot plots showing the presence of a large quiescent CML stem/progenitor cell population (boxed region) in the IM and dasatinib arms, but not the BMS-214662-containing arms. The percentage value in the lower right corner of each plot represents the number of quiescent CML cells remaining at the end of the culture period expressed as a percentage of the starting CD34+ cell number. (D) Representative FACS histogram plot demonstrating the antiproliferative effect of dasatinib and IM compared with no drug control and BMS-214662. (E) Histogram highlighting the cell frequency for each cell division in each treatment arm. In the no drug control and BMS-214662 arms, there is a relative lack of cells in the early divisions (arrowhead ≤ 4 divisions) with increased numbers of cells in the later divisions ( arrow ≥ 6 divisions), compared with the TKI-containing arms, which tended to group together (bracket), with increased cells in the early divisions and fewer cells in later divisions. Data represent mean of 4 experiments.
BMS-214662 is highly effective against primitive quiescent CML stem/progenitor cells, whereas IM or dasatinib induces cytostasis
CML stem/progenitor cells share properties with their normal counterparts being primitive, transplantable, and quiescent.3,31 To follow these cells in culture, we combined CD34 as a primitive marker, with CFSE to enable high resolution tracking of cell division.10,30 A high concentration 5GF cocktail was used to stimulate cell division.10 Previous studies demonstrated that either IM or dasatinib led to increased numbers of undivided (CFSEmax) CD34+ CML cells remaining after culture,10,11,36 in part because of failure to induce apoptosis and as a result of potent antiproliferative effects leading to reversible G1 arrest. Here, BMS-214662 was assessed alone and in combination with IM or dasatinib. By 6 days, the IM and dasatinib arms showed significant accumulation of CFSEmax CD34+ CML cells over control (P = .04 and P = .023, respectively), whereas the arms containing BMS-214662 with either IM or dasatinib showed a significant reduction in these primitive cells to less than 50% of control (Figure 2B; P = .023 and P = .005, respectively). In addition, the reduction in CFSEmax CD34+ CML cells was significantly lower when either IM or dasatinib alone was compared with the combination with BMS-214662 (P = .01 and P = .043, respectively). There were no significant differences in residual CFSEmax CD34+ CML cells between the BMS-214662-containing arms (Figure 2B). IM and dasatinib exerted marked antiproliferative effects as demonstrated in Figure 2C-E, whereas BMS-214662 had minimal antiproliferative effect (Figure 2C-E) and did not overcome the antiproliferative effect of either IM or dasatinib (Figure 2E), indicating that BMS-214662 is able to exert its cytotoxic effect on quiescent cells. Critically, these are the first drug combinations we have tested, using the CFSE assay, which show a significant reduction in quiescent stem/progenitor cells.
BMS-214662 selectively targets Ph+ LTC-IC
LTC-IC is recognized as the most stringent assay to detect very primitive human hematopoietic stem cells in vitro. For successful read-out, stem cells must be fully functional, survive for 5 weeks in the presence of a stromal layer, and then give rise to colonies after a further 2 weeks in colony forming cell assay. We performed LTC-IC assays with both chronic phase CML and normal CD34+ cells after treatment for 72 hours under the same conditions as described in this section above. Compared with control, LTC-IC recoveries were increased in the IM and dasatinib arms (191% and 175%, respectively; P = .033; Figure 3A), indicating that these drugs exert a protective effect on CML stem/progenitor cells in these culture conditions via their antiproliferative effects.10,11 It is possible that the marked antiproliferative and hence protective effect of TKIs on LTC-IC in these experiments are related to the high growth factor concentrations used in the initial 72-hour culture period in the presence of drug. This differs from conditions used by other groups, which have used low growth factor concentration culture conditions and a slightly different LTC-IC method.37 The use of high-concentration growth factors means that, in the no drug control, a large number of stem/progenitor cells enter cell division and proceed toward terminal differentiation. However, in the TKI-containing arms, this proliferative effect is overcome, resulting in increased numbers of cells remaining capable of colony formation after LTC-IC.
Efficacy of BMS-214662 against Ph+ versus Ph− LTC-IC. (A) Results of LTC-IC assay in CML (n = 3). The addition of BMS-214662 to either IM or dasatinib significantly reduced the number of colonies compared with either drug alone (P = .032 and P = .027, respectively). BMS-214662 also significantly reduced the number of colonies compared with the no drug control (P = .028 for BMS-214662 and BMS-214662 + IM arm and P = .031 for BMS-214662 + dasatinib arm). (B) Results of LTC-IC assay in normal donors (n = 3). There was a nonsignificant increase in LTC-IC in the IM and dasatinib only arms. In the BMS-214662-containing arms, there was a nonsignificant reduction in LTC-IC compared with control (P = .079-.29).
Efficacy of BMS-214662 against Ph+ versus Ph− LTC-IC. (A) Results of LTC-IC assay in CML (n = 3). The addition of BMS-214662 to either IM or dasatinib significantly reduced the number of colonies compared with either drug alone (P = .032 and P = .027, respectively). BMS-214662 also significantly reduced the number of colonies compared with the no drug control (P = .028 for BMS-214662 and BMS-214662 + IM arm and P = .031 for BMS-214662 + dasatinib arm). (B) Results of LTC-IC assay in normal donors (n = 3). There was a nonsignificant increase in LTC-IC in the IM and dasatinib only arms. In the BMS-214662-containing arms, there was a nonsignificant reduction in LTC-IC compared with control (P = .079-.29).
The addition of BMS-214662 significantly reduced LTC-IC compared with either IM or dasatinib alone (P = .032 and P = .027, respectively). Furthermore, BMS-214662 alone significantly reduced LTC-IC compared with either IM or dasatinib alone (P = .032 and P = .028, respectively). All 3 BMS-214662–containing arms showed a virtual elimination of colonies to less than 1% of control (P = .033), with no significant difference between the arms. For normal Ph− CD34+ cells (n = 3), there was an effect against LTC-IC in the BMS-214662-containing arms compared with control that did not reach statistical significance after 3 independent experiments (Figure 3B; P = .079-.29, lack of significance thought to be related to small sample size). However, LTC-IC survival was significantly higher for normal compared with Ph+ CD34+ cells (P = .001), with a more than 20-fold reduction in LTC-IC from Ph+ CD34+ cells compared with normal CD34+ cells. Some effect against normal LTC-IC is not unexpected as, in clinical trials, myelosuppression has been a recognized but manageable side effect of treatment with BMS-214662.21,38 These results confirm that BMS-214662 is targeting primitive CML stem/progenitor cells and provide further evidence of selectivity for CML over normal cells.
To further evaluate the Ph status of LTC-IC after treatment, fluorescence in situ hybridization was performed at baseline and on the colonies produced after LTC-IC experiments. All samples were more than 90% Ph+ at baseline (Table 1). However, after LTC-IC, only 1 of 3 patient samples (CML 166) remained Ph+ in residual colonies in the BMS-214662-containing arms. This case illustrates the 10% to 15% of chronic phase CML patients at diagnosis in whom LTC-IC are already exclusively Ph+ (ie, no residual normal hematopoiesis). In the other samples (CML 189 and 215), after treatment with BMS-214662, more than 90% of colonies were Ph−, indicating that these patients had Ph− stem/progenitor cell reserves,39 which selectively survived exposure to BMS-214662 compared with their Ph+ counterparts, which were eradicated. This further illustrates the degree of Ph+ versus Ph− selectivity for BMS-214662.
BMS-214662 is cytotoxic by inducing apoptosis in CD34+ CML stem/progenitor cells
To determine the mechanism of CML stem/progenitor cell elimination under BMS-214662 treatment, we assessed active caspase-3, an irreversible apoptosis step, at 48, 72, and 96 hours culture of CD34+ CML cells. The greatest number of cells with caspase activation was seen at 72 hours in the BMS-214662-containing arms (BMS-214662, 14.6%; BMS-214662 + IM, 18.4%; and BMS-214662 + dasatinib, 12.4%) compared with control (5.5%), IM, or dasatinib (both 7.9%; Figure 4A). At 48 and 72 hours, there was an increase in caspase-3+ cells in the quiescent CFSEmax population. With IM or dasatinib alone, a modest increase in apoptosis was seen (10.9 and 12.2%, respectively) compared with control (8.3%); however, the apoptotic effect was significantly increased by the addition of BMS-214662 (Figure 4B) with 22.0%, 30.8%, and 24.0% apoptotic cells in the BMS-214662, BMS-214662 + IM, and BMS-214662 + dasatinib arms, respectively (P = .045 for BMS-214662-containing vs noncontaining arms). To further confirm induction of apoptosis by BMS-214662 in CD34+ CML cells cultured in SFM only, TUNEL assay and assessment of TMRE were also performed. Exposure to 250 nM BMS-214662 for 24 hours doubled the amount of DNA fragmentation (TUNEL-positive cells; Figure 4C) and decreased the membrane potential (Figure 4D).
Assessment of apoptosis in total CML cells and the quiescent fraction by measurement of caspase-3 activity (n = 4). Percentage of (A) total and (B) quiescent (CD34+ CFSEmax) caspase-3+ CML cells in the different treatment arms after 72 hours of culture. In the quiescent fraction, P = .045 for BMS-214662-containing versus noncontaining arms. Data are represented as mean plus or minus SEM. Illustrative FACS histograms demonstrate (C) increased TUNEL activity (FL-1 channel) in CD34+ CML cells, cultured in SFM only, treated with BMS-214662 compared with no drug control or treatment with BMS-225975, and (D) BMS-214662-induced decrease in the membrane potential, as indicated by a decrease in TMRE signal (FL-2 channel). (E) Percentage of caspase-3+ cells in both CML CD34+38− and CD34+38+ cells after 24 and 48 hours of treatment with BMS-214662 in SFM alone. (F) Percentage of caspase-3+ cells in normal CD34+38− cells after 24 and 48 hours of treatment with BMS-214662. (C-F) Representative results for 3 independent experiments. FSC indicates forward scatter.
Assessment of apoptosis in total CML cells and the quiescent fraction by measurement of caspase-3 activity (n = 4). Percentage of (A) total and (B) quiescent (CD34+ CFSEmax) caspase-3+ CML cells in the different treatment arms after 72 hours of culture. In the quiescent fraction, P = .045 for BMS-214662-containing versus noncontaining arms. Data are represented as mean plus or minus SEM. Illustrative FACS histograms demonstrate (C) increased TUNEL activity (FL-1 channel) in CD34+ CML cells, cultured in SFM only, treated with BMS-214662 compared with no drug control or treatment with BMS-225975, and (D) BMS-214662-induced decrease in the membrane potential, as indicated by a decrease in TMRE signal (FL-2 channel). (E) Percentage of caspase-3+ cells in both CML CD34+38− and CD34+38+ cells after 24 and 48 hours of treatment with BMS-214662 in SFM alone. (F) Percentage of caspase-3+ cells in normal CD34+38− cells after 24 and 48 hours of treatment with BMS-214662. (C-F) Representative results for 3 independent experiments. FSC indicates forward scatter.
To illustrate the effect of BMS-214662 on both mature and primitive CML progenitor cells, total CD34+ cells were sorted into CD34+38+ and the more primitive CD34+38− (< 5% of total CD34+ cells; Figure 4E) fractions and were analyzed for caspase-3 activity after culture in SFM only. BMS-214662 increased caspase-3 activity in both CD34+38+ and CD34+38− fractions (31.5% and 27.7%, respectively, after 48 hours of treatment), highlighting the activity of this drug in both quiescent and cycling cell populations. Interestingly, caspase-3 activity was increased earlier in the more mature CD34+38+ progenitors compared with the CD34+38− fraction (36.6% vs 7.2%, respectively, after 24 hours of treatment). In normal CD34+38− cells, after 48 hours of drug exposure, there was only a modest increase in caspase-3 activity to 9.7% by 48 hours (Figure 4F), indicating the specificity of the drug for leukemia stem/progenitor cells. Importantly, because CD34+38− cells are almost exclusively quiescent, these results highlight the effectiveness of BMS-214662 in the more quiescent leukemia stem/progenitor cell population, which has proved resistant to therapy in the past.
The effect of BMS-214662 on CML stem/progenitor cells is novel and does not occur with other FTIs
Our group has previously shown that the FTI lonafarnib did not significantly reduce survival of quiescent CML stem/progenitor cells.17 BMS-225975 is another FTI, which is structurally very similar to BMS-214662, the only difference being π N methylation on the imidazole ring. These compounds have similar inhibitory effects on FT with IC50s of 0.7 nM and 0.8 nM on the purified enzyme and in cells, for BMS-214662 and BMS-225975, respectively, but differ dramatically in their apoptotic and xenograft antitumor activity.26 To determine whether the apoptotic effect of BMS-214662 in CML was due to more potent inhibition of FT in primary CML, we directly compared its activity with that of BMS-225975. The treatment conditions were: no drug control; BMS-214662; BMS-225975 250 nM; dasatinib; BMS-214662 + dasatinib; BMS-225975 + dasatinib. By 6 days, BMS-214662 had significantly reduced the number of quiescent CFSEmax CD34+ CML cells compared with control (P = .018) and to BMS-225975 containing arms (P = .024). There was no significant difference between control and BMS-225975 arms (Figure 5A). BMS-225975 did not increase caspase-3 activity in either the BMS-225975 or BMS-225975 + dasatinib arms. To determine whether 5GF protected primitive CML cells from apoptosis in response to FTIs, CD34+ cells (Figure 5B) were cultured in the absence of growth factors. On BMS-214662 treatment, a 3- to 5-fold increase over control in caspase-3 activation was observed at 24 hours, similar to 5GF-containing cultures. Increased caspase-3 activation did not occur with BMS-225975.
Comparison of the effects of BMS-214662 with the cytostatic FTI BMS-225975 on quiescent CML stem/progenitor cells (n = 4). (A) The effect of BMS-225975 (250 nM) was not significantly different from the no drug control. Data are expressed as a percentage of the no drug control, and data are represented as mean plus or minus SEM. (B) Percentage of caspase-3+ cells in CD34+ CML cells (n = 6) cultured in the absence of growth factors after 24 hours of treatment with BMS-214662 or BMS-225975.
Comparison of the effects of BMS-214662 with the cytostatic FTI BMS-225975 on quiescent CML stem/progenitor cells (n = 4). (A) The effect of BMS-225975 (250 nM) was not significantly different from the no drug control. Data are expressed as a percentage of the no drug control, and data are represented as mean plus or minus SEM. (B) Percentage of caspase-3+ cells in CD34+ CML cells (n = 6) cultured in the absence of growth factors after 24 hours of treatment with BMS-214662 or BMS-225975.
Previous investigations of BMS-214662 in apoptosis induction in B-cell chronic lymphocytic leukemia40 and myeloma41 have identified inhibition of Mcl-1 and Bax or Bak activation. For CML cell lines and primary CD34+ cells, Bcl-2 family member expression levels were unchanged after treatment with BMS-214662 (data not shown).
BMS-214662 is active in blast crisis CML when combined with a TKI and in cells expressing BCR-ABL kinase domain mutations
In preliminary experiments, we next assessed BMS-214662 alone and in combination with IM or dasatinib in blast crisis CML. BMS-214662 alone showed a trend toward reducing total viable cells (Figure 6A) compared with no drug control. In combination with either IM or dasatinib, it significantly reduced total viable cells compared with either agent alone (P = .04 for both). Not all blast crisis samples assessed were CD34+; however, in those that were, BMS-214662 alone showed a trend toward reducing the number of CFSEmax CD34+ CML cells (Figure 6B). Interestingly, BMS-214662 was much more effective against the CFSEmax CD34+ CML population when combined with either IM or dasatinib, although results failed to reach statistical significance due to the small sample size. This suggests that, although BMS-214662 alone may be sufficient to eliminate CML stem/progenitor cells in chronic phase CML, the combination of BMS-214662 with a TKI is probably to be superior in blast crisis CML.
Effect of BMS-214662 in blast crisis CML (n = 4) and IM-resistant Ba/F3 cell lines. (A) Total viable cells in blast crisis CML after 6 days culture in the different treatment arms. The addition of BMS-214662 to either IM or dasatinib significantly reduced the number of total viable cells compared with either agent alone (P = .04 for both). (B) Total quiescent CD34+ CFSEmax cells present after 6 days of culture. Data are expressed as a percentage of the no drug control, and data are represented as mean plus or minus SEM. (C) Forty-eight–hour proliferation assays for Ba/F3 cell lines with different BCR-ABL kinase mutations after treatment with BMS-214662. Data are the mean of 3 experiments with 5 replicates in each experiment.
Effect of BMS-214662 in blast crisis CML (n = 4) and IM-resistant Ba/F3 cell lines. (A) Total viable cells in blast crisis CML after 6 days culture in the different treatment arms. The addition of BMS-214662 to either IM or dasatinib significantly reduced the number of total viable cells compared with either agent alone (P = .04 for both). (B) Total quiescent CD34+ CFSEmax cells present after 6 days of culture. Data are expressed as a percentage of the no drug control, and data are represented as mean plus or minus SEM. (C) Forty-eight–hour proliferation assays for Ba/F3 cell lines with different BCR-ABL kinase mutations after treatment with BMS-214662. Data are the mean of 3 experiments with 5 replicates in each experiment.
None of the currently available BCR-ABL-specific TKIs inhibits the BCR-ABL kinase mutation T315I. Furthermore, CML stem/progenitor cells may express a variety of BCR-ABL mutations at low levels.42 We therefore determined the efficacy of BMS-214662 in Ba/F3 cells expressing p210 WT BCR-ABL and kinase mutations (WT BCR-ABL, T315I, M351T, and H396P). BMS-214662 was equipotent against WT BCR-ABL and mutant BCR-ABL kinase expressing cells, including T315I (Figure 6C).
Discussion
CML was the first malignancy recognized to be caused by a single genetic abnormality, leading to intensive investigation of its molecular pathogenesis. The concept that CML arises in a pluripotent stem cell was first developed in 195143 with later studies proving clonal expansion in multiple lineages, self-renewal, and transplantation capability.44 Our efforts to characterize this population have focused on identification of CML cells that are primitive, quiescent, and remain cytokine nonresponsive for several days in culture, thereby exhibiting critical stem cell characteristics.10,31,32 The consistent presence of these candidate stem cells in chronic-phase patients provides a possible explanation for the historic failure of intensive chemotherapy to eradicate CML and for the occasional late relapse after transplantation. CML is also an excellent paradigm for hematologic malignancies and solid tumors in which cancer stem cells have been identified and isolated, including breast cancer and tumors of the nervous system.45
There have been major advances in the treatment of CML in recent years with the development of IM,7,8 dasatinib,35 and nilotinib.46 The newer compounds target IM-resistant mutations and, in the case of dasatinib, show enhanced efficacy against primitive cells.11 However, despite moderate inhibition of BCR-ABL, quiescent CML stem/progenitor cells remain insensitive to these compounds.
Here we showed that BMS-214662 was selectively cytotoxic by inducing apoptosis in progenitor (CD34+CD38+) and more primitive (CD34+CD38−) CML cells, including the quiescent fraction, in chronic phase CML. Synergism was demonstrated with TKIs, which represent the most probable combination agents for clinical trials with BMS-214662. Although BMS-214662 exhibited little or no antiproliferative activity as a single agent, it was capable of killing cells arrested in a nonproliferating state by TKIs. This was best demonstrated in Figure 2E in which the BMS-214662 profile matched that of the PBS control across all divisions, whereas all treatment arms that included a TKI showed equivalent antiproliferative effects. The effect of BMS-214662 was shown to include very primitive stem/progenitor cells, such as GF-resistant, quiescent, CD34+CFSEmax cells, and LTC-IC. BMS-214662 dramatically reduced survival and propagation (to < 1%) of the key stem-cell population that is maintained in long-term culture. BMS-214662 also demonstrated preferential cytotoxicity for leukemic stem/progenitor cells as evidenced by superior recovery of normal vs CML LTC-IC and enrichment of Ph− hematopoiesis during LTC-IC assay in 2 of 3 CML samples. In the third sample, in which colonies were BCR-ABL positive at the end of LTC-IC, the patient required growth factor support and a reduced dose of IM to manage the cytopenias resulting from IM therapy consistent with inadequate normal hematopoietic stem cell reserve.
These results demonstrate that BMS-214662 has novel and potent activity in eliminating quiescent CML stem/progenitor cells, which separates it from cytostatic FTIs, such as lonafarnib17 and BMS-225975. BMS-214662 was equally effective at inducing apoptosis in the presence or absence of added GFs. The concentration of BMS-214662 used in these experiments (250 nM) is clinically achievable.21 Our preliminary experiments show that, in vitro, intermittent exposure to BMS-214662, in combination with either IM or dasatinib, enhances the efficacy of these TKIs in CML (data not shown). Although BMS-214662 has yet to enter clinical trial in CML, phase 1 trials in AML have shown promising activity.20 In a future clinical trial under development with Bristol-Myers Squibb and the New Agents Committee, Cancer Research UK, we propose that BMS-214662 be given intermittently in combination with continuous oral dasatinib. In clinical trials in advanced solid tumors, intermittent infusions of BMS-214662 have been successfully combined with cisplatin, carboplatin, and paclitaxel.47,48
Although BMS-214662 had single-agent activity against chronic phase CML CD34+ populations, it appeared most effective when used in combination with a TKI for more advanced phase, as demonstrated by the blast crisis data. The activity of BMS-214662 in blast crisis CML and cell lines expressing BCR-ABL kinase mutations is also important. Patients with blast crisis CML initially respond to IM but then relapse.49 A proportion of these IM-resistant patients will respond to dasatinib or nilotinib, but nearly all relapse within 6 months.35,46 Therefore, BMS-214662 in combination with a TKI may increase the number of patients who respond and the length of remission. For those patients with BCR-ABL kinase mutations, the majority will respond to either dasatinib or nilotinib35,46 ; however, patients with the T315I mutation are resistant to these drugs. These patients may benefit from therapy with BMS-214662, which appears equipotent in WT and mutant BCR-ABL expressing cell lines, including T315I. Because BCR-ABL mutations have been detected in CD34+ cells from IM-treated cases of CML, it is reassuring to find that BMS-214662 not only induces apoptosis of CML stem/progenitor cells but is equally effective in cells harboring mutations.
The effect of BMS-214662 on nonproliferating cells was first identified in solid tumors.28 However, despite extensive investigation, to date, the exact mode(s) of action of BMS-214662 has remained elusive.23,26 Recent in vitro studies of BMS-214662 in B-cell chronic lymphocytic leukemia40 and myeloma41 have identified inhibition of Mcl-1 and Bax or Bak activation in association with apoptosis; however, this was not confirmed here for CML. What was very clear was that BMS-214662 caused cytotoxicity through apoptosis; this was confirmed using 3 alternative assays: expression of active caspase-3, TUNEL, and TMRE staining.
The importance of cancer stem cells is a rapidly emerging area of research, and the ability of BMS-214662 to selectively target quiescent leukemia stem/progenitor cells is a very unusual and important property that is shared by very few anticancer agents.50,,–53 Studies are ongoing to determine whether this property extends to other leukemias and malignancies in which quiescent stem/progenitor cells appear to sustain the disease.
Because BMS-214662 appears to induce selective apoptosis of leukemic stem/progenitor cells, it should prove a useful tool for developing novel approaches for targeting cancer stem cells and in future drug discovery.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank Dr Elisabeth Buchdunger (Novartis Pharma, Basel, Switzerland) for providing imatinib; Professor Junia Melo (Hammersmith Hospital, London) and Dr Brian Druker (Portland, Oregon) for kindly providing the Ba/F3 cell lines; Dr Graham Templeton for CD34+ cell selection; Dr Heather Jorgensen for assistance with FACS sorting; and the healthy donors, CML patients, and United Kingdom hematologists who provided leukapheresis samples.
This work was supported by grants from the Medical Research Council, United Kingdom (G84/6317; M.C.), the Leukemia Research Fund UK (03/20; A.H), the Leukemia Research Trust for Scotland (M.C., F.P.), the Scottish National Blood Transfusion Service (E.K.A.), and the Richard Rockefeller Foundation. F.Y.L. and R.W. are employees of Bristol-Myers Squibb.
Authorship
Contribution: M.C., F.Y.L., R.W., and T.L.H. participated in designing the research; M.C., F.P., L.R., A.H., and E.K.A. performed the research; M.C. and F.P. analyzed the data; M.C., F.P., and T.L.H. wrote the paper; and all authors checked the final version of the manuscript.
Conflict-of-interest disclosure: F.Y.L and R.W are employees of Bristol-Myers Squibb. M.C. and T.L.H have undertaken consultancy work for Bristol-Myers Squibb and received honoraria. T.L.H. has received limited research funding from Bristol-Myers Squibb. All other authors declare no competing financial interests.
Correspondence: Tessa L. Holyoake, Section of Experimental Haematology, Division of Cancer Sciences and Molecular Pathology, 3rd Floor, Queen Elizabeth Building, Glasgow Royal Infirmary, 10 Alexandra Parade, Glasgow G31 2ER, United Kingdom; e-mail: tlh1g@clinmed.gla.ac.uk.