Abstract
The kinase inhibitors imatinib mesylate and dasatinib are the preferred treatment for Philadelphia chromosome–positive (Ph+) leukemias, and they are highly successful in the chronic phase of chronic myeloid leukemia (CML). However, they are not efficient in Ph+ B-cell acute lymphoblastic leukemia (B-ALL). Ph+ leukemia cells are highly resistant to apoptosis, and evidence from cell lines and primary cells suggest Bcl-xL as a critical mediator of resistance to apoptosis: however, this concept has never been rigorously tested in an animal model. To clarify the role of Bcl-xL in Ph+ B-ALL, we generated 2 mouse models. In the first model, Ph+ B-ALL and loss of Bcl-xL expression are coinduced; in the second model, leukemia is induced with expression of Bcl-xL protein well above the levels found in wild-type lymphoblasts. Deletion of Bcl-xL did not inhibit leukemogenesis or affect apoptosis, but increased cellular proliferation. Consistent with this result, overexpression of Bcl-xL led to decreased cellular proliferation. These models reveal an unexpected role for Bcl-xL in cell-cycle entry and the proliferation of tumor cells.
Introduction
The Philadelphia chromosome (Ph) arises from a translocation between chromosomes 9 and 22 and results in formation of a chimeric and constitutively activated tyrosine kinase known as BCR-ABL, which is the cause of chronic myeloid leukemia (CML) and is also expressed in cases of acute B-cell lymphoblastic leukemia (B-ALL). CML initiates as a chronic disease that is followed by an accelerated phase which eventually progresses to a rapidly fatal blast crisis stage. Together, lymphoid blast crisis of CML and Ph+ B-ALL account for 20% of adult patients and 5% of pediatric patients with ALL.1,2 The abl-specific kinase inhibitor imatinib mesylate is the first-line treatment for patients with CML, and it is successful in patients in the chronic phase of the disease. However, it does not provide lasting remission for patients in blast crisis and patients with Ph+ B-ALL,2,3 which was also recently demonstrated for the multitargeted kinase inhibitor dasatinib.4,5 Drugs that target signaling molecules downstream of BCR/ABL may help to overcome this resistance. BCR/ABL is a potent inhibitor of apoptosis, and cells expressing the oncogene are stubbornly resistant to the induction of cell death by a variety of apoptosis-inducing agents.6 Both the archetypical inhibitor of apoptosis, Bcl-2, as well as a second member of this family of antiapoptotic proteins, Bcl-xL, have been suggested as BCR/ABL-regulated effector molecules. Transfection of the pro–B-cell line BaF3 and of the myeloid 32D3 cell line with the oncogene rendered them growth factor independent and led to increased levels of Bcl-2, suggesting a role for this protein in circumvention of cell death.7,8 These results were corroborated by another study, which found a correlation between the amount BCR/ABL expression with the level of Bcl-2 induction and resistance to apoptosis.9 However, different investigators using the same pro–B-cell line to express BCR/ABL reported an increase in the expression levels of the antiapoptotic protein Bcl-xL.9 The relevance of this result is strengthened by the fact that Bcl-xL is a target of the signal transducer and activator of transcription STAT5, and it was previously shown that BCR/ABL leads to constitutive activation of STAT5.10,11 Furthermore, transfection of Ph+ K562 cells with a dominant-negative isoform of STAT5 led to a decrease in Bcl-xL expression and subsequent apoptosis of the cells, suggesting Bcl-xL as an important factor in the prevention of programmed cell death in the context of Ph+ leukemias.11
Given the well-characterized role of Bcl-xL in prevention of apoptosis, cells that express high levels of this protein should have an advantage under the growth-limiting conditions that are present in the tumor microenvironment, thereby contributing to tumorigenesis. Evidence originating from studies with tyrosine kinase inhibitors suggests that decreasing the expression level of Bcl-xL will induce apoptosis. K562 cells express high levels of Bcl-xL, while Bcl-2 is not detectable, and blocking of the tyrosine kinase activity in this cell line as well as in cells isolated from patients with CML in the chronic phase of the disease led to a decrease in Bcl-xL followed by apoptosis.12,13 In agreement with these observations, it is a common finding that cancer cells expressing a constitutively active tyrosine kinase are highly resistant to conventional antineoplastic drugs and concomitantly have high levels of Bcl-xL.14 Thus, it is conceivable that inhibition of Bcl-xL could be an effective treatment for patients with CML who have a resistance to imatinib mesylate by suppressing the consequences of BCR/ABL expression, as well as for patients with Ph+ acute B-cell leukemia.
In the present study, we used an inducible transgenic model of acute B-ALL dependent on BCR/ABL to examine the role of the Bcl-x gene. Several proteins are generated from the Bcl-x gene by alternative splicing, with antiapoptotic Bcl-xL being the most abundant,15 while the shorter Bcl-xs that is not expressed in mice15 exerts proapoptotic signals opposing Bcl-2 and Bcl-xL.16 Using an animal model that allowed us to combine cre/lox-mediated recombination with the tetracycline-inducible expression system, we show that deletion of the Bcl-x gene, resulting in loss of expression of all protein isoforms, does not impair initiation and progression of the B-ALL–like phenotype but rather affects the cell cycle. Bcl-x–deficient lymphoblasts progress faster through the cell cycle than wild-type lymphoblasts, and we did not observe increased apoptosis. Alternatively, we show that expression of Bcl-xL at levels well above the amounts found in BCR/ABL-transformed cells led to a significant decrease in cycling, thus confirming a role for Bcl-xL in manipulating the cell cycle.
Methods
Generation of transgenic mice and genotyping
The human Bcl-xL cDNA17 was subcloned into the multiple cloning site of pTRE2 (Clontech, Mountain View, CA), and the 2.9-kb transgenic construct was injected into the pronucleus of FVBN mice. A total of 3 founder lines were established. Expression of the transgene was tested for by polymerase chain reaction (PCR) and Western blot analysis.
The TRE-p210BCR/ABL transgenic construct and mouse line as well as the Tet-O-cre mice and MMTVtTA transgenic mice were described previously.18-20 Mice that carry loxP sites flanking the Bcl-x gene21,22 were bred with TRE-BCR/ABL animals to generate BCR/ABL-Bcl-x f/f mice. Tet-O-cre mice were bred with MMTVtTA-BCR/ABL mice as well as with BCR/ABL-Bcl-x f/f animals. Cross breeding over several generations produced MMTVtTA-BCR/ABL-cre-Bcl-x f/f animals. All breeding was performed by continuous supplementation of the drinking water.18
Induction of transgenic expression and monitoring of disease
Induction of transgenic expression for p210BCR/ABL and cre recombinase was performed by withdrawal of tetracycline from the drinking water of mice. All animals described in this study were induced at an age of 6 to 8 weeks.
Peripheral blood was collected from the retro-orbital plexus, and total white blood cell (WBC) and differential counts were performed starting on day 10 after induction, followed by a biweekly schedule to monitor development of the phenotype.
Tissue processing and histology
Mice were killed by CO2 inhalation, and cells from bone marrow, lymph nodes, pleural effusion, and the spleen were isolated. All samples were stained with Wright-Giemsa as indicated. Light microscopy was performed with a Nikon Eclipse E600 microscope (Nikon, Melville, NY) using a 40× Plan-Neofluar 0.80 or 100× Plan-Neofluar 1.30 oil lens. Images were captured with a Spot Insight FireWire 11.2 color mosaic camera and SPOT software, version 4.1 (Diagnostic Instruments, Sterling Heights, MI), and Adobe Photoshop version 7.0 (Adobe Systems, San Jose, CA) and Microsoft Powerpoint 2003 (Microsoft, Redmond, WA).
Determination of efficiency of recombination
The efficiency of recombination leading to excision of the Bcl-x gene was determined using a 3-primer PCR strategy.22 DNA was isolated using the protocol also used to isolate DNA from tail snips. The recombined allele generated an amplification product of 280 bp by amplification with primers A and C, while the unrecombined allele gave rise to a product of 300 bp by amplification with primers A and B. Primers A and C could not form an amplification product of the unrecombined allele.
Isolation of proteins and Western blot analysis
Proteins were isolated using 10% trichloracetate (TCA) as described.23 Primary antibodies used in this study were anti–Bcl-x (BD PharMingen, San Diego, CA), anti–Bcl-2 (C-2), anti–c-abl (C- 24-11), anti-actin (C-11; all Santa Cruz Biotechnology, Santa Cruz, CA), and anti–Mcl-1 (Rockland Immunochemical, Gilbertsville, PA).
Isolation of RNA, first-strand cDNA synthesis, and real-time PCR
Total RNA was isolated with Trizol reagent (Invitrogen, Carlsbad, CA) following the manufacturer's guidelines. Each sample was subjected to DNAse treatment (Turbo DNAse; Ambion, Austin, TX), and first-strand synthesis was performed with random hexamer primers and Moloney murine leukemia virus (M-MLV) reverse transcriptase (Invitrogen).
The expression of BCR/ABL, A1, Pim-1, and Bcl-x was measured as a percentage of L19 expression using a SYBR Green assay (Power SYBR Green PCR Master Mix; Applied Biosystems, Foster City, CA) with gene-specific primers (Table 1). All reactions were performed in duplicate.
Flow cytometry analysis and staining for Annexin
Bone marrow cells were isolated as described,23 and cells were incubated with the appropriate antibodies. All analyses were performed on a dual-laser fluorescence-activated cell sorter (FACS; Becton Dickinson, Franklin Lakes, NJ). The following anti-murine antibodies were used: B220, CD34, CD41, Ter119, CD71, Gr-1, Mac-1, c-kit, Sca-1, and BP-1 (BD Pharmingen), CD43, immunoglobulin M (IgM), light chain, and IL7Rα (all from eBioscience, San Diego, CA). For detection of apoptosis, cells were stained with APC-annexin-V and 7-AAD (BD Biosciences, San Jose, CA) following manufacturer's directions.
Multicolor FACS sorting and analysis of developmental B-cell stages
Bone marrow cells were isolated from MMTVtTA-cre mice and T cells, myeloid cells, and erythroid cells were removed by staining with antibodies against CD3, Gr-1, and Ter119, followed by removal of positive cells with magnetic beads to enrich for the B-cell fraction. The remaining cells were stained with antibodies against B220, CD19, CD43, BP-1, and IgM. Sorting was performed according to the staging for mouse bone marrow B lymphopoiesis suggested by Hardy.24,25 Fraction A, also described as pre-pro–B-cell, was sorted as AA4.1+/B220+/CD19−/BP-1−; pro–B cells corresponding to fraction B/C were sorted as B220dim/c-kit+/CD19+/BP-1−. Pre–B cells corresponding to stage C′ were isolated as B220+/CD43+/BP-1+; fraction D was sorted as B220+/CD43−/BP-1+; and fraction E/F was sorted as CD19+/B220high/IgM+. Total RNA was isolated with Trizol followed by DNAse treatment (Turbo DNAse; Ambion). Real-time PCR was performed with primers specific for cre recombinase19 and L19 as internal control. All experiments were performed in duplicates.
BrdU labeling and cell-cycle analysis
Animals were injected 16 hours prior to euthanization with 5 mg BrdU. A total of 106 cells were stained with fluorescently tagged antibodies (eBioscience) specific for B220 and CD19. Staining for BrdU was performed according to the manufacturer's suggestions provided with the BrdU flow kit (BD PharMingen).
In vivo cytotoxicity assay
Animals received one intraperitoneal injection with 100 mg/kg body weight cyclophosphamide (obtained from the Pharmacy of Children's Hospital, Milwaukee, WI). Animals were euthanized after 24 hours, and the percentage of annexin-V+ cells in bone marrow and blood was determined by FACS analysis.
Statistical analysis
Data are expressed as means plus or minus SEM unless otherwise indicated and were compared using a paired Student t test, as described in “Results.” P values less than .05 are considered significant.
Results
Bcl-xL is highly expressed in P210 BCR/ABL–B-ALL transgenic mice
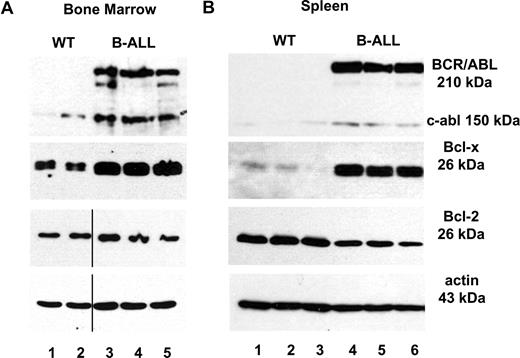
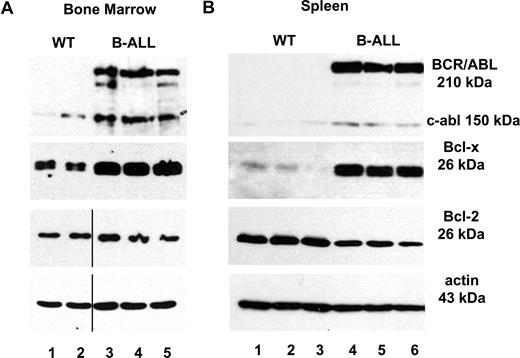
To explore if expression of Bcl-xL is required for development and maintenance of acute B-cell leukemia caused by BCR/ABL, we made use of a p210 BCR/ABL-inducible transgenic expression system18 and combined it with cre/lox-mediated recombination to delete the Bcl-x gene in mice that carry loxP sites framing the gene (Bcl-x f/f).22 We had previously shown that the MMTV–long terminal repeat (LTR) driving the expression of the tetracycline-regulatable transactivator protein tTA targets the B-cell lineage within the murine bone marrow.18,26 MMTVtTA-BCR/ABL transgenic mice succumb to acute pre–B-cell leukemia within 4 to 5 weeks after induction of BCR/ABL expression.18 Analysis of bone marrow cells, lymph node cells, and splenocytes of diseased animals by Western blot analysis demonstrated increased levels of Bcl-xL protein when compared with wild-type control animals, with highest levels found in bone marrow and spleen (Figure 1A,B) and in cells isolated from pleural effusion, which represents an almost homogenous population of cells as determined by staining for cell-surface markers (CD19+/B220+/CD43+/BP-1+/IgM−).
Expression levels of Bcl-xL protein in mice suffering from B-ALL. Protein lysates from (A) bone marrow (wild-type, lanes 1 and 2; B-ALL, lanes 3-5) and (B) spleen (wild-type, lanes 1-3; B-ALL mice, 4-6) from B-ALL mice were compared with wild-type littermate controls after immunoblotting with Bcl-x–, Bcl-2–, and actin-specific antibodies. Expression of p210 BCR/ABL was detected with an antibody against c-abl that also recognizes the fusion protein. Vertical bars indicate repositioned lanes.
Expression levels of Bcl-xL protein in mice suffering from B-ALL. Protein lysates from (A) bone marrow (wild-type, lanes 1 and 2; B-ALL, lanes 3-5) and (B) spleen (wild-type, lanes 1-3; B-ALL mice, 4-6) from B-ALL mice were compared with wild-type littermate controls after immunoblotting with Bcl-x–, Bcl-2–, and actin-specific antibodies. Expression of p210 BCR/ABL was detected with an antibody against c-abl that also recognizes the fusion protein. Vertical bars indicate repositioned lanes.
Crossbreeding of transgenic lines generated the MMTVtTA-BCR/ABL-Cre-Bcl-x f/f genotype that allows for expression of the BCR/ABL oncogene and recombination of the Bcl-x allele within the same target cell.
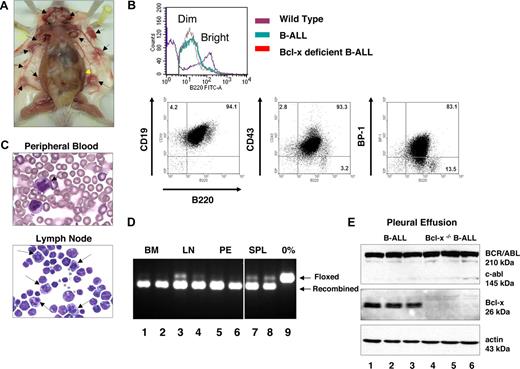
Ph+ B-ALL is initiated and maintained in the absence of Bcl-x expression
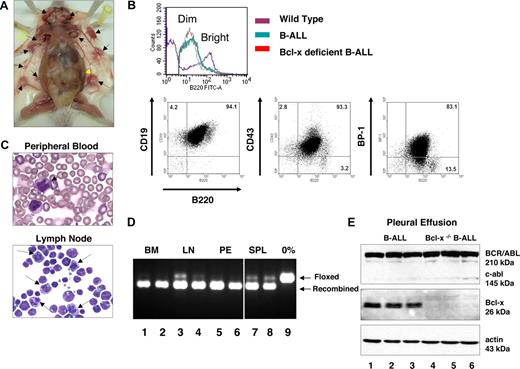
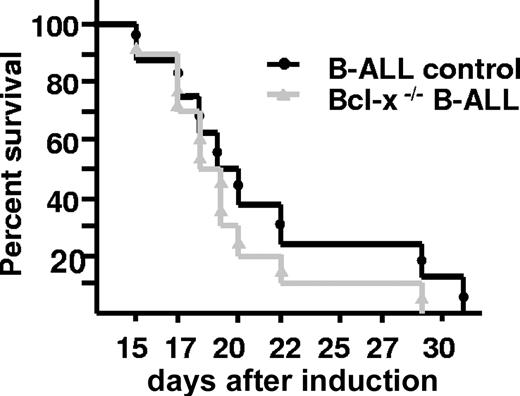
At 6 to 8 weeks of age, tetracycline was withdrawn from the drinking water of experimental MMTVtTA-BCR/ABL-cre-Bcl-x f/f animals (which shall be referred to as Bcl-x–deficient BCR/ABL transgenic mice for brevity), MMTV-BCR/ABL mice that were carried along as control for the development of the B-ALL–like phenotype in the presence of wild-type Bcl-x alleles, and single-transgenic and wild-type animals (Table 2). The disease progressed rapidly, with animals being moribund as early as day 14. By day 29, all mice with the Bcl-x–deficient BCR/ABL genotype had died or had to be killed due to moribund condition. Necropsy of these mice demonstrated massive splenomegaly (up to 10-fold of the size of control animals), pleural effusion filling almost the entire thoracic cavity, and enlargement of the majority of lymph nodes (Figure 2A). FACS analysis demonstrated the transformed cells to be arrested at the pre–B-cell stage of development,24,25 with cells identified as B220dim/CD19+/CD43+/BP-1+, similar to the cell-surface markers identified in Ph+ B-ALL patient samples and MMTV-BCR/ABL transgenic animals (Figure 2B). Although the severity of the disease appeared to be exaggerated in Bcl-x–deficient animals with massive lymph node involvement and rapid onset of pleural effusion, no statistically significant reduction of the survival time was found when littermates were compared (Figure 3). The most prominent difference between the 2 groups of animals was the presence of mitotic figures in the peripheral blood and other tissues isolated from Bcl-x–deficient BCR/ABL transgenic mice (Figure 2C).
Development of B-ALL–like disease in the absence of Bcl-xL. (A) Macroscopic phenotype of Bcl-x–deficient B-ALL mouse 17 days after induction. Enlarged lymph nodes are denoted by black arrows and spleen by the yellow arrow. (B) Top panel: lymphoblasts from diseased mice are B220dim. Bone marrow cells were isolated from wild-type (purple), B-ALL (green), and Bcl-x–deficient B-ALL (red) and stained for expression of B220. Bottom panels: lymphoblasts from Bcl-x–deficient B-ALL mice are arrested at a pre–B-cell stage of development. Bone marrow cells stained for coexpression of B220 and CD19, CD43, and BP-1. (C) Wright-Giemsa staining of peripheral blood (PB; top panel) 14 days after induction and lymph node (LN) cells (bottom panel). Mitotic figures are denoted by black arrows. (D) DNA isolated from tissues of tissues from Bcl-x–deficient B-ALL mice was subjected to 3-primer PCR to determine efficiency of recombination of Bcl-x f/f alleles. DNA was isolated from bone marrow (BM; lanes 1 and 2), lymph node (LN; lanes 3 and 4), pleural effusion (PE; lanes 5 and 6), and spleen (SPL; lanes 7 and 8). Arrows indicate floxed and recombined alleles. Lane 9 represents no recombination. Vertical bars indicate repositioned lanes. (E) Result of Western blot analysis from pleural effusion of B-ALL (lanes 1-3) and Bcl-x–deficient B-ALL (lanes 4-6) mice. Lysates were immunoblotted against c-abl– (loading control, also recognizes BCR/ABL oncoproteins), Bcl-x–, and actin-specific antibodies.
Development of B-ALL–like disease in the absence of Bcl-xL. (A) Macroscopic phenotype of Bcl-x–deficient B-ALL mouse 17 days after induction. Enlarged lymph nodes are denoted by black arrows and spleen by the yellow arrow. (B) Top panel: lymphoblasts from diseased mice are B220dim. Bone marrow cells were isolated from wild-type (purple), B-ALL (green), and Bcl-x–deficient B-ALL (red) and stained for expression of B220. Bottom panels: lymphoblasts from Bcl-x–deficient B-ALL mice are arrested at a pre–B-cell stage of development. Bone marrow cells stained for coexpression of B220 and CD19, CD43, and BP-1. (C) Wright-Giemsa staining of peripheral blood (PB; top panel) 14 days after induction and lymph node (LN) cells (bottom panel). Mitotic figures are denoted by black arrows. (D) DNA isolated from tissues of tissues from Bcl-x–deficient B-ALL mice was subjected to 3-primer PCR to determine efficiency of recombination of Bcl-x f/f alleles. DNA was isolated from bone marrow (BM; lanes 1 and 2), lymph node (LN; lanes 3 and 4), pleural effusion (PE; lanes 5 and 6), and spleen (SPL; lanes 7 and 8). Arrows indicate floxed and recombined alleles. Lane 9 represents no recombination. Vertical bars indicate repositioned lanes. (E) Result of Western blot analysis from pleural effusion of B-ALL (lanes 1-3) and Bcl-x–deficient B-ALL (lanes 4-6) mice. Lysates were immunoblotted against c-abl– (loading control, also recognizes BCR/ABL oncoproteins), Bcl-x–, and actin-specific antibodies.
Survival time of mice suffering from B-ALL and Bcl-x–deficient B-ALL after induction of p210 BCR/ABL expression. Kaplan-Meier plot showing survival time of mice suffering from B-ALL and Bcl-x–deficient B-ALL. Individual mice in each arm are indicated by symbols.
Survival time of mice suffering from B-ALL and Bcl-x–deficient B-ALL after induction of p210 BCR/ABL expression. Kaplan-Meier plot showing survival time of mice suffering from B-ALL and Bcl-x–deficient B-ALL. Individual mice in each arm are indicated by symbols.
Blast cells have undergone complete recombination of the Bcl-x alleles
To ensure that B220dim/CD19+/CD43+/BP-1+ lymphoblasts had undergone complete recombination of both Bcl-x alleles, we performed 3-primer PCR and found almost complete recombination in cells from bone marrow and pleural effusion, while incomplete recombination was observed in the spleen (Figure 2D). Incomplete recombination can be accounted for by the presence of cell lineages, which are not targeted by the MMTVtTA. Even a grossly enlarged spleen consisting mostly of B220dim/CD19+ B cells still contained some mature cells demonstrated by FACS analysis as B220high/CD19+ as well as T lymphocytes, which are not targeted by the MMTVtTA transactivator strain.18 We performed real-time PCR to test for Bcl-xL mRNA as a more sensitive means to validate successful recombination resulting in absence of Bcl-xL expression. Bcl-xL mRNA was not detectable or significantly reduced in cells isolated from Bcl-x–deficient BCR/ABL mice (data not shown), while high levels were found in MMTV-BCR/ABL control mice consistent with the protein data presented in Figure 1. Furthermore, we verified our data by Western blot analysis for expression of p210 BCR/ABL and lack of Bcl-xL in tissues of diseased mice (n = 10; Figure 2E). We conclude that loss of Bcl-xL in the context of BCR/ABL leukemia is not sufficient to either halt the development or reduce the severity of the disease.
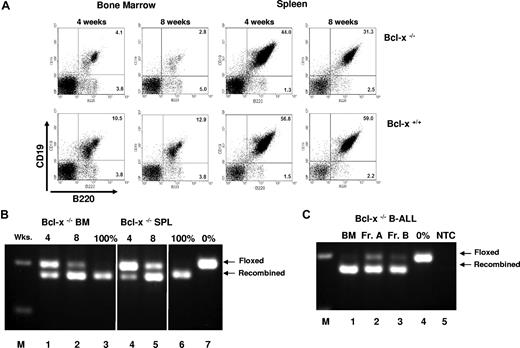
MMTVtTA-cre–mediated recombination occurs in early B-cell progenitor cells
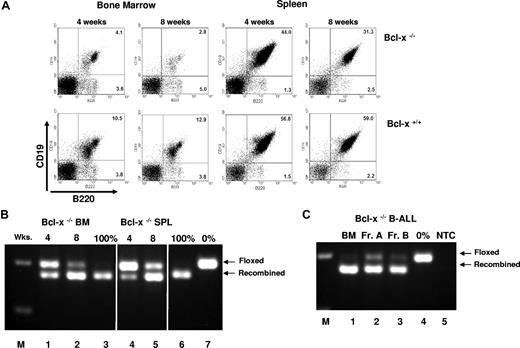
The development of the B-ALL phenotype is all the more surprising in light of the role of Bcl-xL during B-cell development. Expression of the Bcl-x gene is tightly regulated from the pre-pro–B-cell stage (fraction A as defined by Hardy25 ) throughout B-cell development,27 and germ-line deletion of Bcl-x resulted in greatly reduced numbers of cells that were defined as small B220dim/IgM− pre–B cells.22,28 In our model, deletion of Bcl-x targeted by the MMTVtTa transactivator strain in the absence of BCR/ABL resulted in a 60% reduction of the CD19+/B220+ bone marrow cell population compared with controls after 4 weeks, and 80% fewer CD19+/B220+ cells after 8 weeks (Figure 4A). Consistent with these data, we detected recombination by 3-primer PCR in DNA isolated from whole bone marrow and spleen cells (Figure 4B). Based on these observations, we concluded that the pool of cells available for transformation by the BCR/ABL oncogene should be diminished if recombination occurs at the stage of pre-pro–B cell or pro–B cell, when differentiation is more dependent on survival signals mediated by Bcl-xL than in mature populations that are known to express lower amounts of the protein,27 making them perhaps more tolerant to complete deficiency.
Consequences of recombination of Bcl-x alleles on B lymphocytes in the bone marrow and spleen. (A) FACS analysis of bone marrow and spleen cells isolated from MMTVtTA cre bcl-x f/f (Bcl-x−/−), and littermate controls (Bcl-x+/+) 4 or 8 weeks after induction. Cells were stained with antibodies against B220 and CD19. (B) 3-primer PCR performed on DNA isolated from bone marrow (BM; lanes 1 and 2) and spleen (SPL; lanes 4 and 5) of MMTVtTA cre bcl-x f/f mice 4 weeks (lanes 1 and 4) or 8 weeks (lanes 2 and 5) after induction. Arrows indicate floxed and recombined alleles. Lanes 3 and 6 are examples of complete recombination, lane 7 is an example of no recombination, and M denotes 100-bp ladder. Vertical bars indicate repositioned lanes. (C) Recombination of Bcl-x f/f alleles in B-cell development. DNA prepared from whole bone marrow (lane 1), fraction A B lymphocytes (lane 2), and fraction B lymphocytes (lane 3) was subjected to 3-primer PCR. Lane 4 demonstrates no recombination; lane 5, nontemplate control; M, 100-bp ladder.
Consequences of recombination of Bcl-x alleles on B lymphocytes in the bone marrow and spleen. (A) FACS analysis of bone marrow and spleen cells isolated from MMTVtTA cre bcl-x f/f (Bcl-x−/−), and littermate controls (Bcl-x+/+) 4 or 8 weeks after induction. Cells were stained with antibodies against B220 and CD19. (B) 3-primer PCR performed on DNA isolated from bone marrow (BM; lanes 1 and 2) and spleen (SPL; lanes 4 and 5) of MMTVtTA cre bcl-x f/f mice 4 weeks (lanes 1 and 4) or 8 weeks (lanes 2 and 5) after induction. Arrows indicate floxed and recombined alleles. Lanes 3 and 6 are examples of complete recombination, lane 7 is an example of no recombination, and M denotes 100-bp ladder. Vertical bars indicate repositioned lanes. (C) Recombination of Bcl-x f/f alleles in B-cell development. DNA prepared from whole bone marrow (lane 1), fraction A B lymphocytes (lane 2), and fraction B lymphocytes (lane 3) was subjected to 3-primer PCR. Lane 4 demonstrates no recombination; lane 5, nontemplate control; M, 100-bp ladder.
In the following experiment, we sough to determine the developmental stage at which recombination occurs in this model. We isolated pre-pro–B cells (fraction A), pro–B cells (fraction B), and early pre–B cells (fraction C) from the bone marrow of MMTV-Tet-O-cre mice and determined mRNA expression of the cre recombinase gene by real-time PCR. Expression was detected in fraction A, followed by a 5-fold increase of expression in fraction B and subsequent decrease in fraction C cells, comparable with the level observed in fraction A (data not shown). To verify that expression of cre resulted in successful deletion of Bcl-x, we isolated fraction A and fraction B cells from Bcl-x–deficient B-ALL mice 3 and 4 weeks after induction and tested for recombination by 3-primer PCR. Again, we found a high level of recombination in fraction A and a further increase in fraction B (Figure 4C).
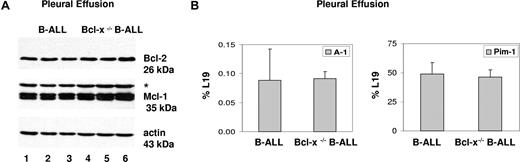
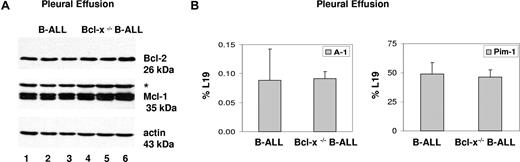
Expression of antiapoptotic proteins and target genes of STAT5 is not affected by deletion of Bcl-x in B-cell lymphoblasts
The presence of recombined alleles in fractions A and B taken together with reduction of CD19+/B220+ cells in the absence of BCR/ABL expression should compromise the pool of cells available for transformation by the oncogene. Following this line of reasoning, an increase in the latency period or complete lack of the B-ALL phenotype would have been the expected result of loss of Bcl-xL expression, as was recently described for STAT5 deficiency.29 This raises the question of whether a compensatory mechanism provides a survival signal otherwise mediated by Bcl-xL. We concentrated on expression of Bcl-2, mcl-1, A1, and pim1 because they either belong to the Bcl-2 family of antiapoptotic genes or are directly downstream of the STAT5 signaling pathway. In addition, they have been linked to BCR/ABL leukemogenesis in in vitro studies using cell lines or primary patient samples.30-32 We determined protein expression levels of Mcl-1 and Bcl-2 by Western blot analysis and mRNA expression by real-time PCR for A1 and Pim-1. Cells from pleural effusion were chosen for this experiment, as they represent an almost homogenous cell population with very few contaminating cells (Figure 2B). Both assays did not show changes in expression of any of these genes in BCR/ABL+ B lymphoblasts (Figure 5A,B).
Expression of Bcl-2, Mcl-1, A1, and Pin-1 kinase in Bcl-x–deficient B-ALL. (A) Western blot analysis of protein lysates from pleural effusion isolated from B-ALL (lanes 1-3) and Bcl-x–deficient B-ALL mice (lanes 4-6). *Actin response from previous stain. (B) mRNA expression levels of A1 and pim1 in cells isolated from pleural effusion were determined by real-time PCR (results are given as mean ± SEM; n = 4).
Expression of Bcl-2, Mcl-1, A1, and Pin-1 kinase in Bcl-x–deficient B-ALL. (A) Western blot analysis of protein lysates from pleural effusion isolated from B-ALL (lanes 1-3) and Bcl-x–deficient B-ALL mice (lanes 4-6). *Actin response from previous stain. (B) mRNA expression levels of A1 and pim1 in cells isolated from pleural effusion were determined by real-time PCR (results are given as mean ± SEM; n = 4).
Cell-cycle analysis of Bcl-x–deficient BCR/ABL+ B lymphoblasts
Microscopic evaluation of blast cells from tissues and peripheral blood of Bcl-x–deficient BCR/ABL mice revealed a high number of mitotic figures (Figure 2C). Increased mitosis is indicative of rapid proliferation; in light of the rapid progression of the phenotype, we wondered if loss of Bcl-xL might have an effect on the cell cycle. Previous studies using overexpression of Bcl-2 or of Bcl-xL in fibroblasts and lymphocytes had suggested that these genes can affect the cell cycle in vitro in addition to their biological roles as inhibitors of apoptosis.33,34
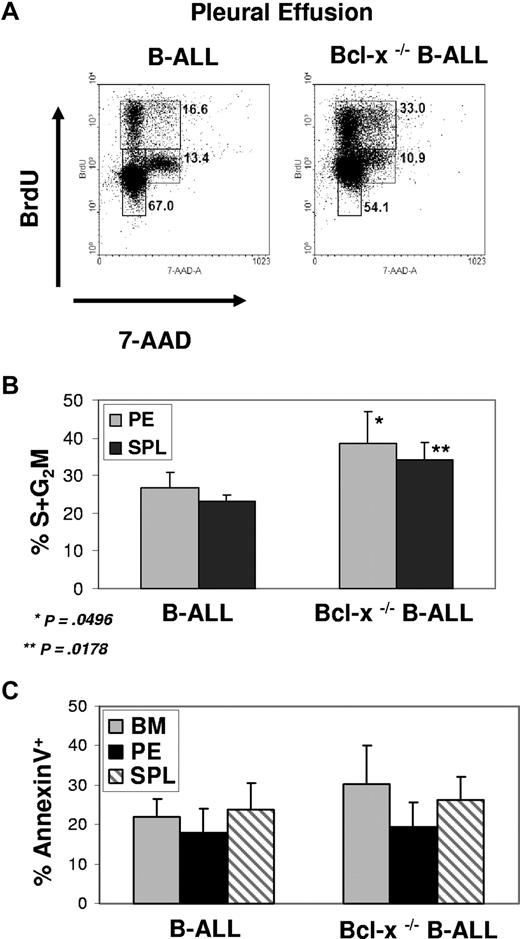
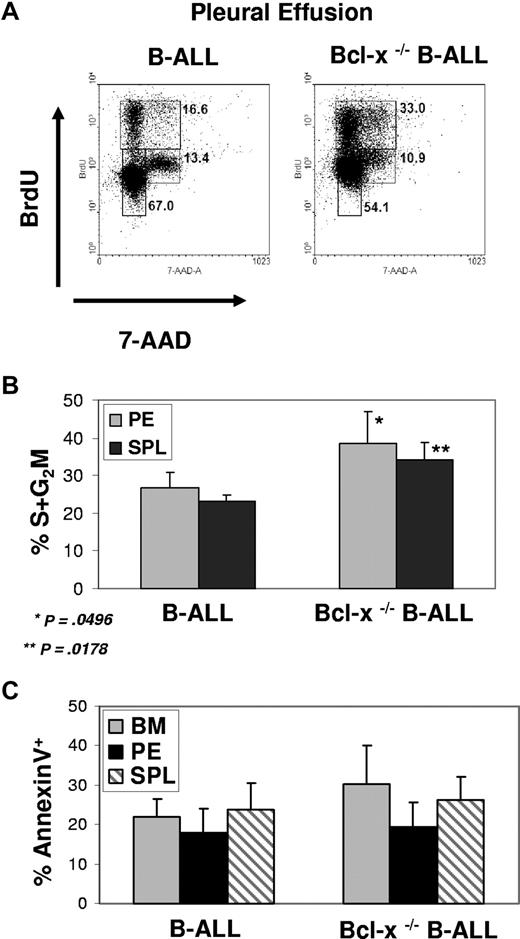
We sought to determine if proliferation and cell-cycle status of cells in mice with the Bcl-x–deficient phenotype was different from MMTVtTA-BCR/ABL control animals. Using BrdU incorporation to perform analysis of the cell cycle, we found a consistent increase in the percentage of cells in S/G2/M phases of the cell cycle in both pleural effusion (29.1% ± 6.5%) and spleen (31.9% ± 4.0%) in Bcl-x–deficient B-ALL cells compared with B-ALL control cells. The difference was significant in both tissues (Student t test, P < .05; Figure 6A,B). These results suggest that although Bcl-xL is dispensable for BCR/ABL-dependent B-ALL development, the protein plays a role in regulating the proliferation rate of lymphoblasts.
Effect of Loss of Bcl-x on cycle entry and apoptosis in BCR/ABL+ lymphoblasts. (A) Pleural effusion isolated from B-ALL and Bcl-x–deficient B-ALL mice 16 hours after BrdU injection. Cells were stained with fluorescently labeled antibodies against B220, CD19, and BrdU. Cell-cycle analysis, BrdU versus 7-AAD, is shown for the gated B220dim, CD19+ population. Shown are representative results of 4 experiments. (B) Graph displaying difference in B220dim, CD19+ S + G2M status in either pleural effusion (PE) or spleen (SPL) cells isolated from B-ALL and Bcl-x–deficient B-ALL diseased mice (average ± SEM; n = 4 for PE and n = 3 for SPL). (C) Bone marrow, pleural effusion, and splenocytes isolated from B-ALL and Bcl-x–deficient B-ALL mice were stained with fluorescently labeled anti-B220, anti-CD19, and anti–annexin-V. Percentage of annexin+ cells are reported for B220dim, CD19+ population only (results are given as means ± SEM; n = 4).
Effect of Loss of Bcl-x on cycle entry and apoptosis in BCR/ABL+ lymphoblasts. (A) Pleural effusion isolated from B-ALL and Bcl-x–deficient B-ALL mice 16 hours after BrdU injection. Cells were stained with fluorescently labeled antibodies against B220, CD19, and BrdU. Cell-cycle analysis, BrdU versus 7-AAD, is shown for the gated B220dim, CD19+ population. Shown are representative results of 4 experiments. (B) Graph displaying difference in B220dim, CD19+ S + G2M status in either pleural effusion (PE) or spleen (SPL) cells isolated from B-ALL and Bcl-x–deficient B-ALL diseased mice (average ± SEM; n = 4 for PE and n = 3 for SPL). (C) Bone marrow, pleural effusion, and splenocytes isolated from B-ALL and Bcl-x–deficient B-ALL mice were stained with fluorescently labeled anti-B220, anti-CD19, and anti–annexin-V. Percentage of annexin+ cells are reported for B220dim, CD19+ population only (results are given as means ± SEM; n = 4).
Loss of Bcl-x expression does not increase apoptosis in Bcl-x–deficient B-ALL
Bcl-xL is a potent inhibitor of apoptosis; loss of this gene might result in higher numbers of cells undergoing cell death, which is negated by increased cycling and proliferation. Cells from the bone marrow, spleen, and pleural effusion of Bcl-x–deficient BCR/ABL transgenic mice were labeled with Annexin, and the number of APC-Annexin+ cells in the B220dim/CD19+ cell population was compared with the same cell population isolated from MMTV-BCR/ABL control mice. There was no difference in Annexin+ cells isolated from spleens and pleural effusion, but we observed a slight increase of cell death in the bone marrow of Bcl-x–deficient B-ALL (1.4-fold) over that of control cells; however, this difference was statistically not significant (Figure 5C).
Overexpression of Bcl-xL in BCR/ABL disease delays progression through the cell cycle
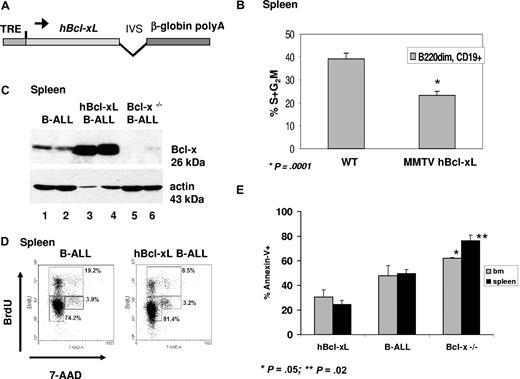
As a corollary study, we tested the effect of overexpression of Bcl-xL on the development of BCR/ABL+ B-ALL by generating mice which carry the cDNA for human Bcl-xL under the control of a tetracycline-responsive element (Figure 7A). Of 3 founder lines that were obtained, one expressed the transgene in bone marrow, lymph nodes, and spleen after withdrawal of tetracycline (data not shown). Analysis of the bone marrow demonstrated that expression of hBcl-xL resulted in a 2-fold increase of cells corresponding to fraction B (CD19+/B220dim/c-kit+/BP1−), while other fractions were not significantly affected (data not shown), as it was reported using an Eμ-Bcl-x transgene.27,35 Cell-cycle analysis of bone marrow cells from double-transgenic animals compared with littermate controls showed reduced cycling of cells in S phase and reduced number of cells in G2 and M phases of the cell cycle (Figure 7B). This difference was highly significant (Student t test, P < .001).
Effect of overexpression of Bcl-xL on cell-cycle entry and response to antineoplastic treatment. (A) Schematic of hBcl-xL transgene. TRE is the responsive element with minimal promoter upstream of the human Bcl-xL cDNA followed by intervening sequence (IVS) and poly A site. (B) Graph displaying difference in B220dim/CD+ S + G2M status in splenocytes isolated from MMTV hbcl-xL and littermate controls (WT; mean ± SEM). For wild-type, n = 5; MMTV hbcl-xL, n = 3. * indicates statistically significant; and **, statistically highly significant. (C) Splenocytes from B-ALL and hbcl-xL B-ALL mice were isolated 16 hours after BrdU injection. Cells were stained with fluorescently labeled antibodies to B220, CD19, and BrdU. Cell-cycle analysis, BrdU versus 7-AAD, is shown for the B220dim/CD19+ population. (D) Western blot analysis of protein lysates from the spleen of B-ALL (lanes 1 and 2), hbcl-xL B-ALL (lanes 3 and 4), and Bcl-x–deficient B-ALL diseased mice. (E) Percentage of cells undergoing apoptosis in bone marrow and spleen after treatment with cyclophosphamide. Animals were killed after a single administration of the drug (results are given as mean ± SEM; n = 3).
Effect of overexpression of Bcl-xL on cell-cycle entry and response to antineoplastic treatment. (A) Schematic of hBcl-xL transgene. TRE is the responsive element with minimal promoter upstream of the human Bcl-xL cDNA followed by intervening sequence (IVS) and poly A site. (B) Graph displaying difference in B220dim/CD+ S + G2M status in splenocytes isolated from MMTV hbcl-xL and littermate controls (WT; mean ± SEM). For wild-type, n = 5; MMTV hbcl-xL, n = 3. * indicates statistically significant; and **, statistically highly significant. (C) Splenocytes from B-ALL and hbcl-xL B-ALL mice were isolated 16 hours after BrdU injection. Cells were stained with fluorescently labeled antibodies to B220, CD19, and BrdU. Cell-cycle analysis, BrdU versus 7-AAD, is shown for the B220dim/CD19+ population. (D) Western blot analysis of protein lysates from the spleen of B-ALL (lanes 1 and 2), hbcl-xL B-ALL (lanes 3 and 4), and Bcl-x–deficient B-ALL diseased mice. (E) Percentage of cells undergoing apoptosis in bone marrow and spleen after treatment with cyclophosphamide. Animals were killed after a single administration of the drug (results are given as mean ± SEM; n = 3).
In order to test the effect of high levels of Bcl-xL in the context of BCR/ABL leukemogenesis, we generated mice with the MMTVtTA-BCR/ABL-hBcl-xL genotype. Development of an aggressive lymphoproliferative disease of the B-cell lineage was detected as measured by the number of white blood cells in the peripheral blood and the appearance of the B220dim/CD19+ population, which was detected at day 10 (WBC ≥ 15 000 cells/μL). Overall, the development and progression of the phenotype between MMTV-BCR/ABL control and MMTVtTA-BCR/ABL-hBcl-xL mice was not significantly different, and all animals were killed due to moribund condition within 4 weeks of induction. Expression of the hBcl-x transgene was readily detected by Western blot analysis (Figure 7C) in triple-transgenic mice. Based on our data that suggest that Bcl-xL affects the proliferation of BCR/ABL+ lymphoblasts, we performed cell-cycle analysis of B220dim/CD19+ B lymphoblasts isolated from the spleen of MMTVtTA-BCR/ABL-hBcl-xL and control mice. We found a significant reduction in the number of cells in S/G2/M phases in triple-transgenic mice compared with controls, which is in agreement with our hypothesis that Bcl-xL does affect the proliferation of cells transformed by BCR/ABL (Figure 7D).
Similar to what we observed in the MMTV-hBcl-xL model without BCR/ABL, we found an increase in fraction B, while fraction A was not affected (data not shown). The effect on the cell cycle underlines our observation made in the Bcl-x–deficient B-ALL mice and suggests that expression of Bcl-xL in the context of BCR/ABL expression in the B-cell lineage rather affects the cell cycle then providing an essential prosurvival signal. Overexpression of the Bcl-x gene leads to reduced cycling of cells, while reduction in the number of B-cell progenitors due to loss of Bcl-x in deficient animals is overcome by the oncogene, leading to an increase in lymphoproliferation.
Apoptotic response after antineoplastic treatment
The number of lymphoblasts undergoing apoptosis did not differ between Bcl-x–deficient B-ALL and control B-ALL, indicating that expression levels of Bcl-xL do not affect apoptosis in Ph+ B-ALL progenitors. However, it is conceivable that Bcl-xL does provide a level of protection apparent only after exposure to potent apoptotic stimuli, such as antineoplastic treatment. To test this hypothesis, we evaluated the apoptotic response after a single administration of cyclophosphamide, a drug that is also used for the treatment of patients with Ph+ B-ALL.36 To assess the number of apoptotic cells, mice were killed 24 hours after administration of the drug, and B220dim/CD19+ cells from bone marrow and spleen and the percentages of annexin-V+ cells were determined by FACS analysis. There was a statistically significant increase in the number of apoptotic cells in both tissues from Bcl-x–deficient B-ALL mice compared with B-ALL controls, while less apoptotic cells were detected in the hBcl-xL B-ALL model (Figure 7E), indicating a direct correlation between Bcl-xL protein levels and susceptibility to apoptosis following a potent stimulus.
Discussion
Disruption or dysregulation of genes that control apoptosis cannot only initiate tumor progression but also enhance resistance to cancer treatment. Previous studies suggest that BCR/ABL+ cells express high levels of Bcl-xL, making them resistant to the induction of apoptosis by a variety of agents.37 Here, we demonstrate that expression of Bcl-xL is not required for leukemogenesis by the BCR/ABL oncogene, and that the disease progresses unimpeded in the absence of this protein. This result is surprising given the fact that expression of Bcl-xL is tightly regulated during B-cell development, and deficiency of this protein leads to a decrease in the number of pro–B cells as shown previously22,28 and substantiated in this study. Our data demonstrate that the MMTVtTA transactivator targets expression of transgenes to the pre-pro–B-cell developmental stage. We did observe a decline in the number of early pro–B cells when deleting the Bcl-x gene in the absence of BCR/ABL, which suggests that the pool available for transformation by the oncogene was diminished (J.G.H., B.I.C., C.S.H., unpublished data, March 2007). Nevertheless, the phenotype developed within the same time frame. Several scenarios can explain this phenomenon. Bcl-xL may not be required for the survival of lymphoblasts, and BCR/ABL provides an alternative survival signal sufficient for early progenitors to progress to the pre–B-cell stage. We have tested this theory and determined the expression levels of Bcl-2, mcl-1, Pim-1 kinase, and A1 in lymphoblasts from Bcl-xL–deficient B-ALL mice and B-ALL control mice. These genes were selected because they either belong to the same family of antiapoptotic proteins as Bcl-xL or are known targets of STAT5. While we did not find changes in expression, it is possible that the expression levels are already sufficient for survival independent of Bcl-xL. Alternatively, an entirely different signaling pathway may be used, and BCR/ABL has been demonstrated to target myriad signaling pathways.38
Last, we cannot exclude the possibility that expression of BCR/ABL and deletion of Bcl-x occurs at different time points. This allows for a sequence of events in which cells first express the oncogene, allowing them to proceed in development before deletion of Bcl-xL expression takes place. Alternatively, recombination of Bcl-xL is the first event leading to reduction of B cells, and the phenotype develops from a small pool of cells. Retroviral transduction of bone marrow cells with BCR/ABL can establish B-ALL as a monoclonal disease suggestive of transformation of a single cell.39
STAT5 is a major activator of Bcl-xL transcription and a regulator of cellular growth and differentiation in a wide variety of tissues.40-43 It was recently shown that complete deletion of STAT5 renders bone marrow cells resistant to transformation and leukemia development induced by BCR/ABL.29 The lack of transformation in this model also raises the question about the role of Bcl-xL. STAT5 is required for a plethora of signaling pathways, including but not limited to immunoglobulin heavy chain variable gene rearrangement,44 which is absolutely necessary for B cells to avoid elimination by apoptosis. Thus, BCR/ABL is either entirely deprived of the B-cell population in the absence of STAT5, or it does not provide a strong enough survival signal to overcome this impediment in the absence of STAT5. However, this STAT5-mediated effect is upstream of Bcl-xL, as we have confirmed in our model system that rearrangement of IgH variable genes is not affected by loss of Bcl-xL (data not shown).
Regardless, these considerations are only important from a developmental point of view; they are not relevant with respect to maintenance of BCR/ABL+ leukemia, as B lymphoblasts in our model have undergone complete recombination and targeting expression of the Bcl-x gene appears to exacerbate development of the leukemia phenotype with significantly more cells in S and G2/M phases of the cell cycle than lymphoblasts from control animals. In contrast to this result and consistent with the ability of Bcl-xL to manipulate the cell cycle, we found G1 arrest and reduced cycling in lymphoblasts that express amounts of the protein well above the levels of wild-type cells transformed by the BCR/ABL oncogene in our model (Figure 7C; J.G.H., B.I.C., C.S.H., unpublished results, June 2007). The difference in cell-cycle progression and generation time between control lymphoblasts and deficient cells becomes all the more apparent by theoretic calculation of the number of tumor cells that can arise from one single cell within 1 week: we report a difference in cell cycle of 29.1% plus or minus 6.5%; by taking a difference of 23% into calculation, 256 cells will arise as progeny from a wild-type tumor cell compared with 1024 cells from a Bcl-x−/− cell.
Known for its survival promoting function, our results suggest an additional function for Bcl-xL, an antiapoptotic protein as a regulator of the cell cycle; this concept has support in the literature. Transgenic expression of Bcl-2 in normal fibroblasts and lymphocytes delayed entry into the cell cycle,33,45,46 while Bcl-2–deficient T lymphocytes exhibited accelerated cell-cycle progression.34 One molecular mechanism by which loss of Bcl-xL might affect cycling in our model system could be through degradation of the cyclin-dependent kinase inhibitor p27. A previous study using transgenic expression of Bcl-xL in NIH-3T3 cells revealed a delay in cell-cycle entry through elevation of p27,46 and cell lines transfected with BCR/ABL have shown that the oncogene targets p27 protein leading to its proteasomal degradation, thereby enhancing proliferation of cells.47,48
There is also evidence that support the idea that antiapoptotic proteins manipulate the cell cycle in the context of neoplastic disease. Transgenic expression of Bcl-2 delayed tumor development and reduced proliferation in a murine model of breast tumors.49 In hematologic malignancies, high levels of Bcl-2 were found to correlate with lower proliferative capacity in non-Hodgkin lymphoma,50,51 and the majority of follicular lymphoma carry a chromosomal translocation t(14;18) that places Bcl-2 under control of the immunoglobulin heavy chain enhancer, leading to high expression of the protein.52-55 Nevertheless, these tumors are indolent and have a low proliferative index and clinical aggressivity. Another classic example is chronic lymphoid leukemia (CLL). The hallmark of this disease are nondividing cells with increased expression of Bcl-2 in almost all patients and of another antiapoptotic protein, Mcl-1, in approximately 50% of patients.56-59
Here, we report a novel role for Bcl-xL in the context of BCR/ABL-associated leukemia as a regulator of the cell cycle that tempers disease progression. In contrast to the prevailing concept that suggests that levels of Bcl-xL are important for BCR/ABL-transformed cells to evade apoptosis, we found that Bcl-x–deficient cells proliferate at a greater rate, while high levels of this protein correlated with slower growth rate. Taken together, we conclude that Bcl-x is not essential for Ph+ B-ALL, but its expression limits tumor burden.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Lothar Hennighausen (National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health [NIH], Bethesda, MD) for providing Bcl-x f/f mice, Dr Ulrich Steidl (Beth Israel Deaconess Medical Center, Boston, MA) for critically reading the manuscript, the Transgenic Facility of the Medical College of Wisconsin for performing microinjections, and Hope Albertz and Corbett Reinbold from the FACS Core Facility at the Blood Research Institute for assistance with cell sorting.
This work was supported by grants from the Blood Center Research Foundation and the Lauri Strauss Leukemia Foundation to C.S.H. J.G.H. was supported by NIH training grant HL-07209.
National Institutes of Health
Authorship
Contribution: J.G.H. designed and performed experiments; B.I.C. performed experiments; and C.S.H. designed the study, supervised J.G.H. and B.I.C., and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Claudia S. Huettner, The Blood Research Institute, Rm 210, 8727 Watertown Plank Rd, Milwaukee, WI 53226; e-mail: claudia.huettner@bcw.edu.