Abstract
Inpatient length of stay (LOS) has been studied with respect to its influence on treatment costs in patients (pts) undergoing high dose chemotherapy (HDC) followed by autologous stem cell transplantation (ASCT). We conducted a retrospective study to identify associations between pretransplantation patient characteristics and LOS, and to assess the prognostic effect of LOS in pts undergoing HDC followed by ASCT for lymphoma.
630 pts who received a busulfan-based HDC preparative regimen followed by ASCT at the Cleveland Clinic between 1997 and 2006 form the study cohort. 510 pts (81%) had non- Hodgkin’s lymphoma and 120 pts (19%) had Hodgkin’s lymphoma. Pts were admitted to the hospital for administration of the preparative regimen followed by infusion of autologous stem cells and were discharged after granulocyte recovery (neutrophils >500/ μL) unless complications prolonged hospitalization. The median age at transplant was 50 years (range, 18–77) and median time from diagnosis to transplant was 17 months (range, 2–372). The median length of stay was 21 days (range, 16–77).
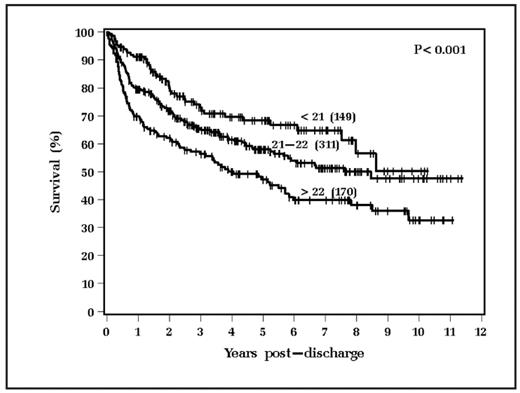
Recursive portioning analysis with a log rank splitting method identified three LOS groups predictive of overall survival: <21 days (149 patients), 21–22 days (311 patients) and >22 days (170 patients). LOS was analyzed with this categorization and also as a continuous variable.
Longer LOS was associated with older age (p<0.001), higher number of days of apheresis required to achieve the target stem cell collection (p<0.001) and lower CD 34+ cell dose (p<0.001);pts with non-Hodgkin lymphoma had a longer LOS than pts with Hodgkin lymphoma (p=0.018).Other pre-transplant parameters including gender, race, Karnofsky performance status, number of prior chemotherapy regimens, prior radiation therapy, months from diagnosis to transplant, disease status at transplant, LDH and preparative regimen were not associated with LOS.
370 pts (59%) are alive with a median follow up of 51 months (range, 3–137). The median relapse-free survival was 2.2 years for pts with LOS>22 days, 3.6 years for pts with LOS 21–22 days and 6.1 years for pts with LOS <21 days (p=0.041). The median overall survival was 4 years for pts with LOS >22 days, 8.5 years for LOS 21–22 days and the median has not been observed in pts with LOS less than 21 days ( p<0.001), as shown in figure below. Non-relapse mortality was the highest in the group with the longest LOS (p=0.008).
On multivariate analysis, the significant adverse prognostic factors for overall survival were longer length of stay (p<0.001), older age at transplant (p<0.001), relapsed disease at transplant (p<0.001) and oral compared to IV busulfan in the preparative regimen (p=0.003).
These data indicate that we can segregate pts into distinct prognostic groups based on LOS. Pts with longer LOS should be targeted for more intensive follow-up.
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author