Abstract
Background: BK virus infection has been associated with development of HC after HSCT, but most studies detected the virus at the time of bleeding, therefore not allowing estimation of the risk imposed by asymptomatic infection. We hypothesized that viruria prior to HSCT increased the risk of HC, and sought to investigate this hypothesis in a cohort of consecutive patients receiving HSCT from donors other than HLA-identical siblings in our institution from 09/2005 and 08/2007.
Patients and Methods: We prospectively performed a quantitative PCR on urine samples collected before admission to transplant and on day 30 after transplant. The quantitative BK virus assay was performed at Focus Diagnostics, Inc., Cyprus, CA with a commercially available kit. A set of quantitative standards are run in parallel and assay is linear through 39 million copies/mL. Risk factors for the development of HC were evaluated on univariate and multivariate analysis using Cox’s regression model. The cumulative incidence (CI) of HC was estimated considering death without HC as a competing event.
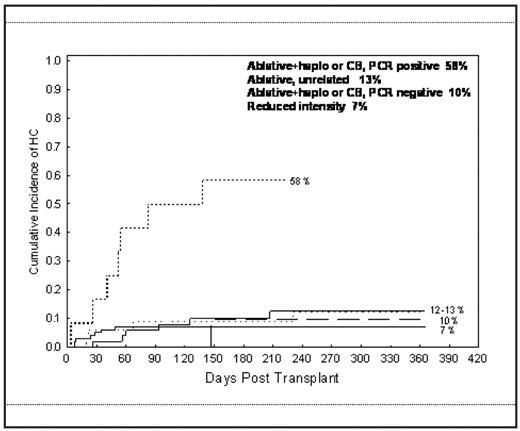
Results: 209 pts were studied (132 males). Median age was 49 years (range, 19–71). Diagnoses included leukemias (n=161, 77%), lymphoma and myeloma (n=46, 22%) and others (n=2, 1%). Donors were unrelated (n=178), haploidentical (n=8) and unrelated cord blood (CB) (n=23). Stem cell source was bone marrow (BM, n=78), peripheral blood (PB; n=108), and CB (n=23). . Conditioning regimen was myeloablative in 110 pts and reduced intensity (RIC) in 99 pts; 38 pts (18%) received cyclophosphamide-containing regimens. GVHD prophylaxis was tacrolimus and mini-methotrexate. Median time to platelet engraftment was 20 days (range, 0–164). Pre transplant BK viruria was detected in 96 patients (46%). The number of viral copies ranged from 300 to > 200 million copies. Twenty five patients (11%) developed HC within one year after HSCT at a median of 59 days (range, 8–225). In 6 pts, HC was diagnosed before platelet engraftment. The severity of HC was grade 1 in 3 pts, grade 2 in 11, grade 3 in 8, an grade 4 in 3. On univariate analysis, donor type was the most significant predictor of the incidence of HC within a year of HSCT, with recipients of haploidentical or CB transplant having the highest incidence rate (HR=3.1, p=0.009). There was also a trend for higher HC incidence in patients who received a myeloablative conditioning (HR=2.3, p=0.06), and in those who had a positive PCR before transplant (HR=2, p =0.095). Because of the small number of HC cases in pts who received a RIC (n=7/99, CI of HC 7%) we could not perform a multivariate analysis adjusting for the type of conditioning. In patients who received a myeloablative conditioning multivariate analysis showed a significantly higher incidence of HC in pts who received a haploidentical or CB transplant (HR=3.8, p=0.006); and in pts with a positive PCR before transplant (HR=2.9, p=0.03). The cumulative incidence of HC in pts who had both adverse factors was 58%, compared with 11% and 13% in those who had either one or none of these factors, respectively. There was no significant association between the incidence of HC and grade II-IV acute GVHD, considered as a time dependent variable, patient age, stem cell type (BM vs. PB), use of cyclophosphamide in conditioning, BK viral load, or PCR positivity on day 30 post HSCT. With a median follow-up among survivors of 11 months (range 4–32), HC, considered as time dependent variable, did not have a significant impact on survival.
Conclusion: BK viruria pre-HSCT may be a predict factor for development of HC, especially for those receiving haploidentical or CB transplants using a myeloablative regimen.
Cumulative incidence of HC as a function of preparative regimen intensity and BK virus PCR status pre transplant
Incidence of HC
| Variable (n) . | No patients with HC (%) . |
|---|---|
| Total (209) | 25 (12%) |
| Age | |
| ≤ 50 years (99) | 12 (12%) |
| > 50 years (110) | 13 (12%) |
| Sex | |
| M/F 132/77 | 16(12%)/9(12%) |
| Diagnosis | |
| Leukemia (161) | 18 (11%) |
| Lymphoma (40) | 7 (17.5%) |
| Conditioning | |
| Ablative (110) | 18 (16%) |
| Non-ablative (99) | 7 (7%) |
| Donor Type | |
| MUD(169) | 17 (10%) |
| Haplo/cords (31) | 8 (25%) |
| acute GVHD | |
| I – II (88) | 10 (12%) |
| III – IV (26) | 4 (15%) |
| Pre SCT PCR | |
| Positive (96) | 16 (17%) |
| Negative (111) | 9 (8%) |
| Variable (n) . | No patients with HC (%) . |
|---|---|
| Total (209) | 25 (12%) |
| Age | |
| ≤ 50 years (99) | 12 (12%) |
| > 50 years (110) | 13 (12%) |
| Sex | |
| M/F 132/77 | 16(12%)/9(12%) |
| Diagnosis | |
| Leukemia (161) | 18 (11%) |
| Lymphoma (40) | 7 (17.5%) |
| Conditioning | |
| Ablative (110) | 18 (16%) |
| Non-ablative (99) | 7 (7%) |
| Donor Type | |
| MUD(169) | 17 (10%) |
| Haplo/cords (31) | 8 (25%) |
| acute GVHD | |
| I – II (88) | 10 (12%) |
| III – IV (26) | 4 (15%) |
| Pre SCT PCR | |
| Positive (96) | 16 (17%) |
| Negative (111) | 9 (8%) |
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author