Abstract
Background: Deletion of 17p in chronic lymphocytic leukaemia (CLL) is associated with resistance to conventional therapy and a poor clinical outcome. Though TP53 mutations have been described in some of these cases, the extent to which they occur in CLL patients and their clinical implications remain unclear. We investigated the prognostic value of TP53 mutations in the clinical course of CLL patients.
Methods: We analysed 529 CLL samples from the UK LRF CLL4 clinical trial (Chlorambucil vs Fludarabine±Cyclophosphamide) for the presence of TP53 mutations and their association with response to treatment, progression-free survival (PFS) and overall survival (OS). We also investigated the correlation between TP53 mutations and other well-known prognostic indicators in CLL including stage, chromosomal aberrations, VH mutational status and CD38 and ZAP-70 expression.
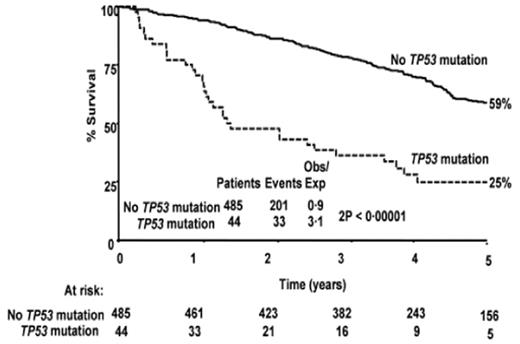
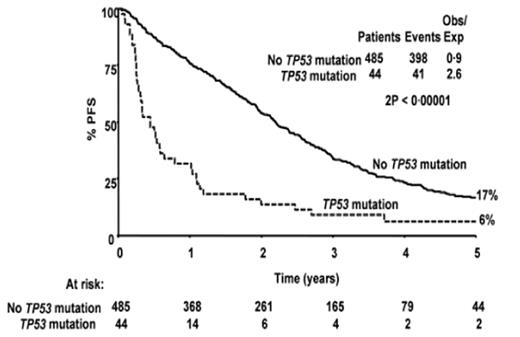
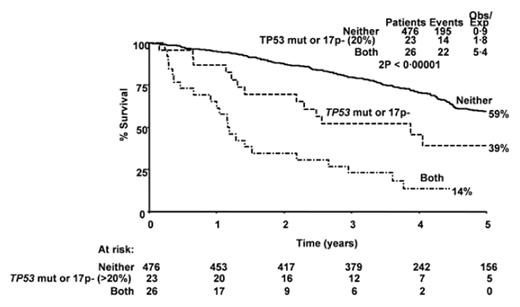
Results: Mutations of TP53 were found in 44 of 529 patients overall (8.3%). TP53 mutations were present in 26 out of 32 (81%) patients with 17p deletion in >20% of cells (p<0.0001). TP53 mutations were also present at lower frequencies in samples with no 17p deletion (13/446; 2.9%) or with <20% of cells with 17p deletion (4/47; 8.5%). Overall response rates were significantly better in patients without TP53 mutations compared to those with mutations (82% vs 34%; p<0.0001), including complete or nodular partial responses in 42% of patients without TP53 patients compared to only 10% of patients with mutations (p<0.0001). TP53 mutations were associated with significantly poorer OS; 36% (95% CI 22–51) at 3 years versus 79% (95% CI 75–83) for patients without mutations, p<0.00001 (Figure 1a). Similarly, PFS was significantly shorter for patients with TP53 mutations (3 year PFS: 9% [95% CI: 1–18]) compared to those without (34% [95% CI 30–38], p<0.00001; Figure 1b). CLL patients with TP53 haploinsufficiency -either TP53 mutation or >20% of 17p deletion- define a subgroup with intermediate prognosis (3 year OS: 52% [95% CI 32–73]) compared to those with neither (80% [95% CI 76–83]) or both (23% [95% CI 7–39]) (p(trend)<0.00001, Figure 2). There was no significant association between TP53 mutations and age, stage, VH mutations, CD38 expression, ZAP-70 expression or any other chromosomal abnormality other than 17p deletion.
Conclusions: Our data shows that TP53 mutations are associated with a poor outcome in CLL patients regardless of the deletion of 17p. Furthermore, the clinical significance of 17p deletion seems to be tightly linked to the presence of mutations in the remaining TP53 allele, and these patients with no wild-type TP53 genes have the lowest OS and PFS rates. Finally, the group of CLL patients with TP53 haploinsufficiency (either by mutation or deletion in >20% of the cells) presents an intermediate prognosis and will be further investigated.
OS by TP53 mutational status
PFS by TP53 mutational status
OS by TP53 mutational status and/or 17p deletion
Disclosures: No relevant conflicts of interest to declare.
Author notes
Corresponding author