Abstract
c-MYC inhibits differentiation and regulates the process by which cells acquire biomass, cell growth. Down-regulation of c-MYC, reduced cell growth, and decreased activity of the PI3K/AKT/mTORC1 signal transduction pathway are features of the terminal differentiation of committed myeloid precursors to polymorphonuclear neutrophils. Since mTORC1 regulates growth, we hypothesized that pharmacological inhibition of mTORC1 by rapamycin may reverse the phenotypic effects of c-MYC. Here we show that granulocytes blocked in their ability to differentiate by enforced expression of c-MYC can be induced to differentiate by reducing exogenous c-MYC expression through rapamycin treatment. Rapamycin also reduced expression of endogenous c-MYC and resulted in enhanced retinoid-induced differentiation. Total cellular c-Myc mRNA and c-MYC protein stability were unchanged by rapamycin, however the amount of c-Myc mRNA associated with polysomes was reduced. Therefore rapamycin limited expression of c-MYC by inhibiting c-Myc mRNA translation. These findings suggest that mTORC1 could be targeted to promote terminal differentiation in myeloid malignancies characterized by dysregulated expression of c-MYC.
Introduction
The bHLH-LZ transcription factor c-MYC acts in a gene-specific manner by binding consensus E-box motifs in target genes to activate transcription1-6 and generally to influence chromatin structure,7-9 resulting in master regulation of key biologic processes including differentiation, proliferation, and apoptosis. Unsurprisingly, the consequences of dysregulated c-MYC expression are profound: loss of c-MYC expression in knockout mice is embryonically lethal10 and overexpression of c-MYC in mouse models results in malignant transformation.11-16 In addition, overexpression of c-MYC is observed in many forms of human cancer as a result of chromosomal translocations, gene amplification, altered protein stability, or other ill-defined mechanisms.17-19
An increasingly recognized function of MYC is the ability to drive cell growth by regulating a subset of genes critical for cellular metabolism, macromolecular (RNA and protein) synthesis, and protein turnover.20-23 c-MYC has been shown to regulate RNA polymerase II–dependent synthesis of ribosomal proteins20,23,24 and RNA polymerase III–dependent synthesis of 5S rRNA and tRNAs,25 and more recently we and others have linked it to RNA polymerase I–dependent transcription,26-29 resulting in the coordinate up-regulation of ribosome biogenesis that is required for growth. A key feature of the growth-promoting role of c-MYC is its ability to act in concert with the PI3K/AKT/mTORC1 signal transduction pathway not only to coordinate ribosome biogenesis but also via modulation of ribosome function to promote its own expression.
The mTORC1 complex represents a vital downstream node in the PI3K/AKT signal transduction pathway for matching rates of protein synthesis to nutrient availability.30,31 Under favorable energy conditions, signaling through mTORC1 contributes to ribosome biogenesis by improving the efficiency with which mRNAs containing a 5′ TOP (terminal oligopyrimidine tract) are translated.32-34 mTORC1 also drives rDNA transcription via phosphorylation of S6 kinase 1 and subsequent downstream signaling to UBF.35 In addition, phosphorylation of another mTORC1 substrate, 4EBP1, releases eIF4E from inhibitory binding by 4EBP1 allowing eIF4E to participate in a fully competent translation initiation complex. In turn, this permits the cap-dependent translation of a subset of mRNAs containing a complex secondary structure in the 5′ UTR region that is weakly translated when the activity of the PI3K pathway is suboptimal.36 This subset of mRNAs with a complex 5′ UTR includes c-Myc and other growth- and cell cycle–related transcripts such as ornithine decarboxylase (Odc) and cyclin D1.37 The macrolide antibiotic rapamycin is a potent mTORC1 inhibitor. Rapamycin and its analogues act in complex with the immunophilin FK506-binding protein 12 (FKB12), to bind and selectively inhibit mTORC1 activity and therefore limit ribosome numbers and function.38-41
Terminal myeloid differentiation (TMD) is the process by which committed myeloid precursors mature into polymorphonuclear neutrophils. In addition to the acquisition of specialized effector functions such as synthesis of antimicrobial molecules that are stored in cytoplasmic granules, TMD is characterized by cell-cycle exit and profound reductions in mRNA translation and protein synthesis. Repression of c-MYC expression is required for TMD and enforced expression of c-MYC prevents differentiation,18,42-44 and induces myeloid leukemia in mice.14,45 Furthermore, impaired TMD is a hallmark of acute myeloid leukemia (AML),46,47 a disease in which c-MYC is frequently dysregulated via the generation of upstream fusion oncoproteins, constitutive tyrosine kinase activity, or gene amplification.17,48-51 Therefore measures to target c-MYC expression at a posttranscriptional level in AML represent a valid therapeutic strategy. However, at present, posttranscriptional mechanisms that regulate c-MYC expression in normal and malignant granulocytes are not well understood.
In this study, we used a retinoid-dependent in vitro model of TMD, the MPRO (mouse promyelocyte)52 model to investigate interactions between mTORC1 and c-MYC. We show that mTORC1 activity is required for c-MYC expression and inhibition of TMD by c-MYC. Rapamycin treatment of granulocytes impaired in their ability to differentiate by enforced c-MYC expression led to reduced expression of exogenous c-MYC, restored differentiation, and decreased cell growth and resulted in G1 cell-cycle arrest. In cells undergoing retinoid-induced differentiation, rapamycin further reduced endogenous c-MYC protein expression and resulted in more rapid differentiation. Levels of total cellular c-Myc mRNA and c-MYC protein stability in granulocytes were unchanged after rapamycin treatment; however, the amount of polysomal c-Myc mRNA was reduced, indicating that mTORC1 inhibition reduced c-MYC expression by repressing mRNA translation.
Methods
Cell culture and cell analyses
The MPRO cell line52 was maintained in DMEM containing 20% fetal bovine serum (FBS; Gibco, Carlsbad, CA), BHK-HM5 conditioned media equivalent to 1000 units/mL granulocyte-macrophage colony-stimulating factor (GM-CSF), and penicillin-streptomycin-glutamine (PSG; Gibco). For differentiation, cells were plated into DMEM containing 10% FBS, BHK-HM5 conditioned media equivalent to 1000 units/mL GM-CSF, and PSG 12 hours prior to the addition of the retinoid X receptor (RXR)–specific agonist AGN194204 (Allergan, Irvine, CA). pBabe-MYC-ER retroviruses were used to infect MPRO cell lines as previously described.43 Infected cells were selected with 2 μg/mL puromycin (Sigma-Aldrich, St Louis, MO). For cell morphology, 25 000 cells were cytospun onto glass slides, air dried, methanol fixed, and stained with May-Grünwald Giemsa (MGG). Cell volume was determined using a Sysmex CDA 500 instrument (Kobe, Japan).
Cell surface marker expression
Harvested cells were incubated at 4°C with PE-conjugated anti-CD11b antibody (Pharmingen, San Diego, CA) in the presence of 24.2G conditioned media, washed, and resuspended in the 7AAD prior to analysis using the fluorescence-activated cell sorting (FACS) Calibur instrument interfaced with Cellquest software (Becton Dickinson, San Jose, CA).
SDS-PAGE Western blotting
Immunoblotting was performed using 50 μg total protein extracts lysed in sodium dodecyl sulfate (SDS) lysis buffer (50 mM Tris, pH 6.8, 1% SDS, 10% glycerol, 1 mM DTT, protease inhibitors), separated by SDS–polyacrylamide gel electrophoresis (PAGE), transferred to PVDF membranes, probed with rabbit anti–c-MYC (sc-764; Santa Cruz Biotechnology, Santa Cruz, CA) and mouse anti–α-tubulin (Sigma-Aldrich), then visualized using enhanced chemiluminescence. Band quantitation was performed using ImageJ software (National Institutes of Health, Bethesda, MD; http://rsbweb.nih.gov.ij/download.html).
Cell-cycle analysis
Cells (500 000) were treated with bromodeoxyuridine (BrdU) for 30 minutes at 37°C prior to fixation in 95% ethanol. Subsequently, cells were permeabilized (1 M HCl, 0.5% Triton X-100), incubated with mouse IgG anti-BrdU (Becton Dickinson) followed by FITC-conjugated sheep anti–mouse-IgG (Cappel; MP Biomedicals, Aurora, OH), and resuspended in Propidium Iodide prior to analysis using a FACS Calibur flow cytometer (Becton Dickinson).
35S methionine labeling
Cells were incubated in methionine-free DMEM for 30 minutes followed by the addition of 50 μCi/mL trans-35S-labeled methionine for 60 minutes at 37°C. After termination of labeling, protein from lysed cells was subject to TCA precipitation and determination of 35S incorporation by scintillation counting.
RNA isolation, cDNA synthesis, and quantitative real-time polymerase chain reaction
Total RNA was isolated from cells using Trizol (Invitrogen, Carlsbad, CA) and reverse transcribed by Superscript III (Invitrogen) using random hexamers (Promega, Madison, WI). Real-time PCR was performed using the ABI prism 7000 thermocyler and SYBR Green dye detection method (Applied Biosystems, Warrington, United Kingdom) then quantitated using the delta-delta CT (ΔΔCT) method. Primers were designed using the Primer Express program (Applied Biosystems), and the sequences are listed in Table S1 (available on the Blood website; see the Supplemental Materials link at the top of the online article).
Polysome analysis
Cells were treated with 100 μg/mL cycloheximide (Sigma-Aldrich) for 5 minutes prior to harvest, then lysed in hypotonic lysis buffer (50 mM Tris pH 7.5, 15 mM KCl, 25 mM MgCl, 0.5% Triton X-100, 0.5% sodium deoxycholate, 3 mM DTT, and 0.12 U/μL RNasin), separated on 17% to 50% sucrose gradients then fractionated using a UA-6 detector (Teledyne Isco, Lincoln, NE) to allow continuous monitoring of RNA content per fraction. RNA was obtained by phenol-chloroform extraction then generation of cDNA and quantitative real-time (qRT)–PCR was performed as described in the previous paragraph.
Results
Rapamycin restores terminal myeloid differentiation in granulocytes with enforced c-MYC expression
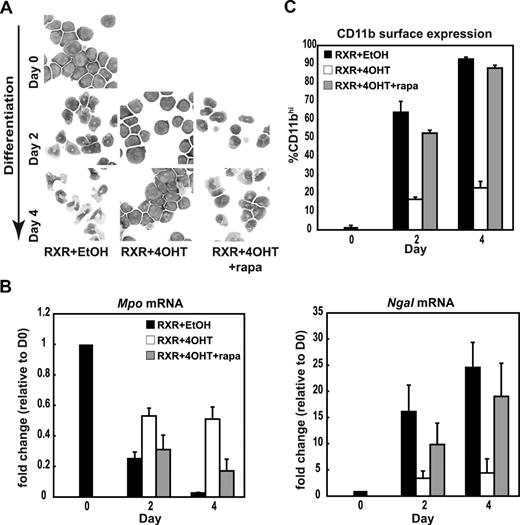
To test for functional interactions between c-MYC and mTORC1 during granulocytic differentiation, we transduced MPRO cells with a retrovirus encoding c-MYC-ER (pBabe-MYC-ER).53,54 Cells were treated with the retinoid X receptor–specific agonist AGN194204 (RXR) and underwent TMD over 4 days. In the pBabe-MYC-ER system, addition of 4-hydroxytamoxifen (4OHT) results in the generation of a functional MYC-ER fusion protein capable of transactivating c-MYC target genes.53,54 In MPRO cells expressing the c-MYC-ER construct, activation of c-MYC by the addition of 4OHT rendered cells resistant to differentiation by RXR (Figure 1A and McArthur et al43 ). As c-MYC and the PI3K/AKT/mTORC1 pathway have complementary functions in the regulation of cell growth, we hypothesized that mTORC1 activity is required for the c-MYC–mediated differentiation block. We therefore examined whether rapamycin could restore retinoid sensitivity to promyelocytes made refractory to RXR by c-MYC-ER overexpression. Strikingly, examination of cell morphology in cytospins from c-MYC-ER–expressing promyelocytes treated with RXR and rapamycin in combination revealed cells with the characteristic ring-shaped nucleus, condensed chromatin, and pale cytoplasm of differentiated murine granulocytes (Figure 1A; Table S2). In addition to cell morphology, we characterized further the response of granulocytes to rapamycin by examining transcriptional markers of differentiation. In MPROs, the transcriptional differentiation program initiated by RXR results in a shift from transcription of the gene encoding the primary granule–associated protein myeloperoxidase (Mpo), to the gene encoding the secondary granule–associated protein neutrophil gelatinase–associated lipocalcin (Ngal). We therefore measured Mpo and Ngal mRNA levels by qRT-PCR in c-MYC-ER–expressing cells treated with rapamycin. Both Mpo down-regulation and Ngal up-regulation in response to RXR were significantly attenuated by expression of c-MYC-ER, whereas rapamycin restored the temporal pattern of expression such that Mpo and Ngal levels in MPRO c-MYC-ER cells treated with 4OHT and rapamycin were not statistically different from differentiated controls at day 4 (Figure 1B). Rapamycin also restored the impairment of up-regulation of the myeloid cell surface marker CD11b that resulted from activation of c-MYC-ER (Figure 1C). Interestingly, for most differentiation parameters, the trend was toward incomplete rescue of the phenotype with rapamycin that persisted at a day-6 time point (data not shown). Overall, these data demonstrate that rapamycin can restore the characteristic cell morphology, gene transcription, and protein expression patterns associated with TMD to MPRO cells expressing the c-MYC-ER fusion protein. Thus, mTORC1 inhibition can over-come the block in TMD conferred on granulocytes by enforced expression of c-MYC.
Rapamycin restores differentiation in granulocytes with enforced expression of c-MYC. (A) Representative morphology of MGG-stained MPRO c-MYC-ER cells induced to differentiate prior to induction (day 0) and after induction of differentiation (day 2 and day 4) by 10−6 M AGN194204 in the presence of vehicle control (RXR + EtOH), 200 nM 4-hydroxytamoxifen (RXR + 4OHT), or 200 nM 4OHT and 80 nM rapamycin (RXR + 4OHT + rapa). (B) c-MYC-ER MPROs were treated as described in panel A. Quantitative real-time PCR (qRT-PCR) was performed using primers directed against myeloperoxidase (Mpo) and neutrophil galactosidase-associated lipocalcin (Ngal), corrected for the expression of β-2-microglobulin and normalized to expression in day-0 undifferentiated controls. (C) Surface expression of CD11b was determined by FACS analysis for MPRO c-MYC-ER cells treated as indicated in panel A. Results in panels B and C are expressed as mean plus or minus SEM for 3 independent experiments.
Rapamycin restores differentiation in granulocytes with enforced expression of c-MYC. (A) Representative morphology of MGG-stained MPRO c-MYC-ER cells induced to differentiate prior to induction (day 0) and after induction of differentiation (day 2 and day 4) by 10−6 M AGN194204 in the presence of vehicle control (RXR + EtOH), 200 nM 4-hydroxytamoxifen (RXR + 4OHT), or 200 nM 4OHT and 80 nM rapamycin (RXR + 4OHT + rapa). (B) c-MYC-ER MPROs were treated as described in panel A. Quantitative real-time PCR (qRT-PCR) was performed using primers directed against myeloperoxidase (Mpo) and neutrophil galactosidase-associated lipocalcin (Ngal), corrected for the expression of β-2-microglobulin and normalized to expression in day-0 undifferentiated controls. (C) Surface expression of CD11b was determined by FACS analysis for MPRO c-MYC-ER cells treated as indicated in panel A. Results in panels B and C are expressed as mean plus or minus SEM for 3 independent experiments.
c-MYC–dependent growth in granulocytes is reduced by rapamycin
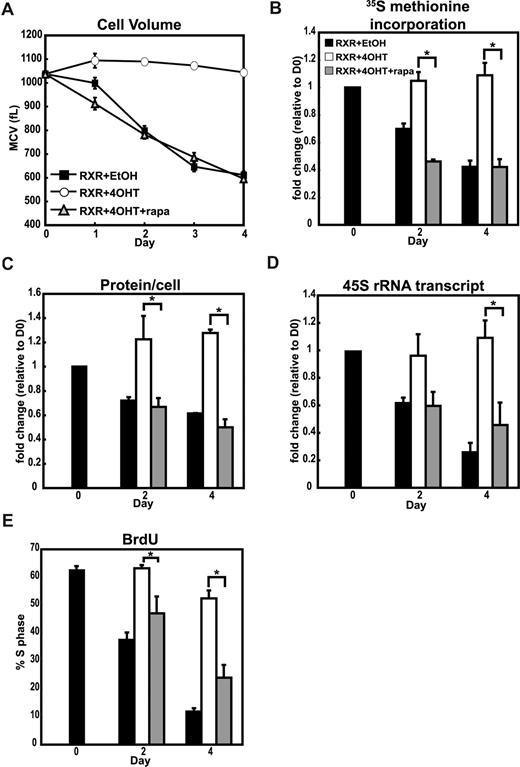
Experimental approaches used to identify and classify MYC target genes have consistently identified a subset of genes involved in promoting cellular metabolism and protein synthesis.20,21,24 Conversely, sensing of reduced growth factor signaling and nutrient availability by mTORC1 results in down-regulation of rDNA transcription and ribosome biogenesis leading to G1 cell-cycle arrest.55-57 Since down-regulation of cell growth is a feature of TMD, we asked whether antagonism of c-MYC–driven cell growth was characteristic of granulocytes with restored differentiation potential due to rapamycin. We therefore examined the growth and proliferative behavior of granulocytes with enforced c-MYC expression treated with RXR to induce differentiation after mTORC1 inhibition.
Cells with enforced c-MYC expression do not reduce their cell volume in response to RXR. Although rapamycin-treated cells were smaller than differentiating controls at day 1, from day 2 onward cell volumes of rapamycin- and control-treated cells were indistinguishable (Figure 2A). These changes in cell volume suggested that c-MYC–driven growth and/or proliferation were restricted by mTORC1 inhibition, prompting us to explore these parameters after rapamycin treatment.
mTORC1 activity is required for c-MYC–mediated cell growth in granulocytes. (A) MPRO c-MYC-ER cells were induced to differentiate with 10−6 M AGN194204 and treated with EtOH (RXR + EtOH), 200 nM 4OHT (RXR + EtOH), or 200 nM 4OHT and 80 nM rapamycin (RXR +4OHT + rapa). The mean cell volume (MCV) was determined at the indicated time points by the Coulter method. (B) Protein synthesis was determined by measuring incorporation of 35S methionine into total cellular protein in c-MYC-ER MPRO cells treated as indicated as described for panel A. Results at day 2 and day 4 are represented as the percentage counts per minute relative to undifferentiated (day 0) cells. (C) c-MYC-ER MPRO cells (107) treated as described in panel A were lysed in 1% SDS lysis buffer containing protease inhibitors. Total protein per cell was determined using a modified Lowry assay. Results at day 2 and day 4 are represented as fold change relative to values for undifferentiated (day 0) cells. (D) Abundance of the unprocessed 45S rRNA transcript was determined by qRT-PCR using primers directed against the 5′ ETS region, corrected for β-2-microglobulin transcript abundance and represented as fold change over day 0 for MPRO c-MYC-ER cells induced to differentiate under the conditions described in panel A. (E) The percentage of cells in S phase was determined by FACS analysis of BrdU-positive cells for MPRO c-MYC-ER cells under the conditions described in panel A. For all sections, the data shown are the mean plus or minus SEM of 3 independent experiments. *P < .05, Student t test.
mTORC1 activity is required for c-MYC–mediated cell growth in granulocytes. (A) MPRO c-MYC-ER cells were induced to differentiate with 10−6 M AGN194204 and treated with EtOH (RXR + EtOH), 200 nM 4OHT (RXR + EtOH), or 200 nM 4OHT and 80 nM rapamycin (RXR +4OHT + rapa). The mean cell volume (MCV) was determined at the indicated time points by the Coulter method. (B) Protein synthesis was determined by measuring incorporation of 35S methionine into total cellular protein in c-MYC-ER MPRO cells treated as indicated as described for panel A. Results at day 2 and day 4 are represented as the percentage counts per minute relative to undifferentiated (day 0) cells. (C) c-MYC-ER MPRO cells (107) treated as described in panel A were lysed in 1% SDS lysis buffer containing protease inhibitors. Total protein per cell was determined using a modified Lowry assay. Results at day 2 and day 4 are represented as fold change relative to values for undifferentiated (day 0) cells. (D) Abundance of the unprocessed 45S rRNA transcript was determined by qRT-PCR using primers directed against the 5′ ETS region, corrected for β-2-microglobulin transcript abundance and represented as fold change over day 0 for MPRO c-MYC-ER cells induced to differentiate under the conditions described in panel A. (E) The percentage of cells in S phase was determined by FACS analysis of BrdU-positive cells for MPRO c-MYC-ER cells under the conditions described in panel A. For all sections, the data shown are the mean plus or minus SEM of 3 independent experiments. *P < .05, Student t test.
As mTORC1 and c-MYC are known to regulate protein synthesis we examined whether rapamycin could reduce rates of de novo protein synthesis by measuring 35S methionine incorporation after induction of c-MYC. Whereas cells expressing c-MYC-ER continued to demonstrate high levels of 35S methionine incorporation, we found that rapamycin significantly inhibited de novo protein synthesis such that rates of 35S methionine incorporation were lower than or equivalent to those in differentiating control cells (Figure 2B). Since total protein per cell reflects the net result of rates of protein synthesis and turnover, we measured this to determine whether regulation of protein turnover by rapamycin contributed to the attenuated growth observed in differentiating granulocytes. There was an approximately 50% reduction in total protein per cell in rapamycin-treated c-MYC-ER–expressing cells compared with RXR- and 4OHT-treated cells (Figure 2C). Furthermore, inhibition of de novo protein synthesis by rapamycin accounted for the observed reduction in total protein per cell, suggesting that protein turnover makes a limited contribution to c-MYC–mediated effects on protein metabolism in differen-tiating granulocytes.
Since transcription of the rDNA genes has been reported to be limiting for ribosome biogenesis,58,59 we tested whether rates of rDNA transcription correlated with de novo protein synthesis. Because the 45S precursor rRNA is rapidly processed after transcription, the abundance of unprocessed 45S rRNA transcripts serve as an indirect measure of rates of rDNA transcription. To determine rates of rDNA transcription we used qRT-PCR, using primers directed against the 5′ externally transcribed spacer (5′ ETS) of the rDNA gene as we have done previously.27 We found an approximately 70% reduction in rRNA transcription during differentiation in control cells that was completely abrogated by enforced expression of c-MYC. Rapamycin treatment resulted in significant down-regulation of 45S rRNA precursor expression in cells with enforced MYC expression, indicating that mTORC1 inhibition is capable of curtailing c-MYC–driven rDNA transcription in differentiating granulocytes (Figure 2D).
Control of cell growth during G1 by mTORC1 has been reported to be a key regulator of G1 to S phase cell-cycle progression.60-62 We used a FACS-based assay of BrdU incorporation to perform cell-cycle analysis of MPRO c-MYC-ER–expressing cells treated with rapamycin. Enforced expression of c-MYC-ER resulted in a marked increase in the percentage of cells remaining in S phase after treatment with RXR and this was significantly reduced by rapamycin (Figure 2E). As dysregulated expression of c-MYC often induces apoptosis,63,64 we also examined surface expression of annexin V in RXR-treated MPRO MYC-ER cells. Induction of MYC-ER with 4OHT resulted in higher levels of annexin V expression at day 4 after RXR treatment that were reduced to a level comparable to control cells treated with 4OHT and rapamycin (Figure S2A,B), suggesting antagonism of the proapoptotic action of c-MYC by rapamycin. From these data, we conclude that attenuated growth, proliferation, and apoptosis are characteristics of rapamycin-induced TMD in cells with enforced c-MYC expression.
Rapamycin inhibits expression of c-MYC
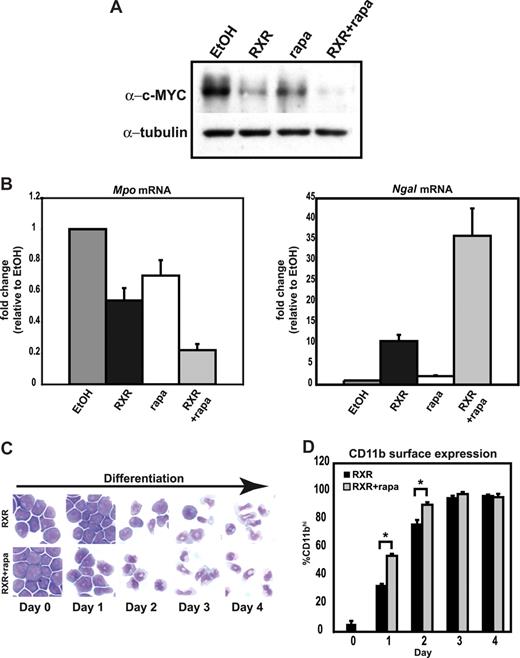
We hypothesized that the altered differentiation potential of rapamycin-treated granulocytes could be explained by direct inhibition of c-MYC expression or by reduction in mTORC1-dependent cell growth signaling pathways downstream of c-MYC. To test for alterations in c-MYC expression, we measured the amount of c-MYC-ER protein in differentiating MPROs after rapamycin treatment. We found c-MYC-ER was expressed at high levels in cells after 4OHT and RXR treatment but fell to noninduced levels with additional rapamycin treatment (Figure 3A). We also tested the ability of rapamycin to reduce expression of the c-MYC-ER fusion protein in the absence of RXR and observed comparable reductions in c-MYC-ER expression using rapamycin alone or in combina-tion with RXR (Figure 3B). Therefore rapamycin reduces c-MYC-ER levels independent of RXR.
mTORC1 activity is required to maintain expression of c-MYC-ER in MPRO granulocytes. (A) c-MYC-ER MPRO cells were induced to differentiate with 10−6 M AGN194204 in the presence of 200 nM 4OHT, EtOH (vehicle control), or 200 nM 4OHT plus 80 nM rapamycin (rapa) as indicated. Protein lysates made from cells harvested after 2 and 4 days of treatment were analyzed by Western blotting for expression of c-MYC-ER. (B) MPRO c-MYC-ER cells were treated with 200 nM 4OHT to activate c-MYC-ER in the presence of 10−6 M AGN194204 (RXR), rapamycin (rapa), or a combination of both for 48 hours. Expression of c-MYC-ER was determined by Western blotting. For panels A and B, α-tubulin was used as a loading control. (C) Abundance of the c-MYC target genes cyclin D2, mTERT, ODC, and UBF was determined by qRT-PCR in MPRO c-MYC-ER–expressing cells after differentiation induction, in the presence of EtOH (RXR + EtOH), 4OHT (RXR + 4OHT), or 4OHT and rapamycin (RXR + 4OHT + rapa). Results were corrected for β-2-microglobulin transcript abundance and represented as fold change over day-0 controls. (D) Transcript abundance of the retinoid responsive genes Mad1 and CEBPϵ was determined by qRT-PCR as described in panel C. For panels C and D, data represent mean plus or minus SEM of 3 independent experiments.
mTORC1 activity is required to maintain expression of c-MYC-ER in MPRO granulocytes. (A) c-MYC-ER MPRO cells were induced to differentiate with 10−6 M AGN194204 in the presence of 200 nM 4OHT, EtOH (vehicle control), or 200 nM 4OHT plus 80 nM rapamycin (rapa) as indicated. Protein lysates made from cells harvested after 2 and 4 days of treatment were analyzed by Western blotting for expression of c-MYC-ER. (B) MPRO c-MYC-ER cells were treated with 200 nM 4OHT to activate c-MYC-ER in the presence of 10−6 M AGN194204 (RXR), rapamycin (rapa), or a combination of both for 48 hours. Expression of c-MYC-ER was determined by Western blotting. For panels A and B, α-tubulin was used as a loading control. (C) Abundance of the c-MYC target genes cyclin D2, mTERT, ODC, and UBF was determined by qRT-PCR in MPRO c-MYC-ER–expressing cells after differentiation induction, in the presence of EtOH (RXR + EtOH), 4OHT (RXR + 4OHT), or 4OHT and rapamycin (RXR + 4OHT + rapa). Results were corrected for β-2-microglobulin transcript abundance and represented as fold change over day-0 controls. (D) Transcript abundance of the retinoid responsive genes Mad1 and CEBPϵ was determined by qRT-PCR as described in panel C. For panels C and D, data represent mean plus or minus SEM of 3 independent experiments.
In most instances, c-MYC functions as a heterodimer with MAX to bind E-box sequences within gene promoters and activate transcription. We therefore examined whether the reduction in exogenous c-MYC expression seen after rapamycin treatment also reduced transcriptional activation of c-MYC target genes. We assayed the mRNA abundance of the well-characterized c-MYC target genes cyclin D2, Odc, mTert, and Ubf by qRT-PCR and found that they were reduced in cells treated with rapamycin and 4OHT compared with 4OHT-treated cells (Figure 3C). In contrast, transcript abundance of the retinoid-regulated genes Mad1 and Cebpϵ was not regulated by rapamycin (Figure 3D), suggesting the observed changes in abundance of c-MYC target gene mRNAs resulted from rapamycin regulation of c-MYC protein expression rather than more global inhibition of gene transcription per se. Thus, reduced c-MYC-ER protein expression after rapamycin treatment leads to decreased c-MYC function at target gene promoters.
To confirm the effects of mTORC1 inhibition also applied to expression of endogenous c-MYC in myeloid cells, we used a nontransduced MPRO model. Expression of c-MYC was considerably reduced by RXR alone after 2 days of treatment, a time when c-MYC is known to be dynamically regulated in MPROs.27 Inhibition of mTORC1 with rapamycin alone also reduced expression of c-MYC by approximately 50% in the absence of RXR. More striking was the observation that combined treatment with rapamycin and RXR was able to augment the reduction in c-MYC expression induced by RXR alone, suggesting that mTORC1 can regulate endogenous c-MYC levels during TMD (Figure 4A). qRT-PCR of MPROs treated with rapamycin in the absence of RXR resulted in some reduction in Mpo mRNA and a negligible increase in Ngal mRNA abundance (Figure 4B), however these modest changes in granule transcript abundance were not accompanied by morphologic evidence of differentiation (data not shown). Importantly, changes in Mpo and Ngal expression after RXR and rapamycin combination treatment were greater than the shifts induced by RXR alone (Figure 4B). These data suggests rapamycin could not substitute for RXR but could cooperate with retinoids to enhance differentiation.
Rapamycin reduces expression of endogenous c-MYC and promotes terminal myeloid differentiation. (A) MPRO cells were treated with EtOH (vehicle control), 10−6 M AGN194204 (RXR), 80 nM rapamycin (rapa), or 10−6 M AGN194204 and 80 nM rapamycin in combination (RXR + rapa) for 48 hours. Protein lysates were analyzed for c-MYC expression by Western blotting. α-Tubulin was used as a loading control. (B) Quantitative real-time PCR was used to assay the abundance of myeloperoxidase (Mpo) and neutrophil-galactosidase-associated lipocalcin (Ngal) transcripts in MPRO cells treated as described in panel A. Results were corrected for β-2-microglobulin transcript abundance and represented as fold change relative to undifferentiated EtOH (vehicle control). Results are the mean plus or minus SEM of 3 independent experiments. (C) Representative morphology of MGG-stained MPRO cells treated with 10−6 M AGN194204 and EtOH (vehicle control) or 80 nM rapamycin. (D) Cells treated as in panel C were subject to FACS analysis for surface expression of CD11b. For panels B and D, results are the mean plus or minus SEM of 3 independent experiments. *P < .05, Student t test.
Rapamycin reduces expression of endogenous c-MYC and promotes terminal myeloid differentiation. (A) MPRO cells were treated with EtOH (vehicle control), 10−6 M AGN194204 (RXR), 80 nM rapamycin (rapa), or 10−6 M AGN194204 and 80 nM rapamycin in combination (RXR + rapa) for 48 hours. Protein lysates were analyzed for c-MYC expression by Western blotting. α-Tubulin was used as a loading control. (B) Quantitative real-time PCR was used to assay the abundance of myeloperoxidase (Mpo) and neutrophil-galactosidase-associated lipocalcin (Ngal) transcripts in MPRO cells treated as described in panel A. Results were corrected for β-2-microglobulin transcript abundance and represented as fold change relative to undifferentiated EtOH (vehicle control). Results are the mean plus or minus SEM of 3 independent experiments. (C) Representative morphology of MGG-stained MPRO cells treated with 10−6 M AGN194204 and EtOH (vehicle control) or 80 nM rapamycin. (D) Cells treated as in panel C were subject to FACS analysis for surface expression of CD11b. For panels B and D, results are the mean plus or minus SEM of 3 independent experiments. *P < .05, Student t test.
To analyze the differentiation phenotype more carefully, a 4-day time course was performed using MPROs treated with RXR and either rapamycin or control. Differential cell counts performed on MGG-stained cytospin preparations revealed a subtle increase in the percentage of differentiated neutrophils in rapamycin-treated cultures relative to controls (Table 1). In keeping with the earlier appearance of morphologically differentiated cells in cytospin preparations obtained after rapamycin (Figure 4C), we also observed a significant increase in the number of cells with high CD11b expression after rapamycin treatment at both 1 and 2 days of differentiation (Figure 4D), suggesting that the retinoid-dependent differentiation of MPROs could be accelerated by rapamycin. MPRO c-MYC-ER cells differentiated in the absence of 4OHT (and therefore expressing only endogenous c-MYC) also exhibited evidence of enhanced morphologic differentiation when treated with rapamycin (data not shown). Therefore, as with expression of c-MYC-ER, endogenous c-MYC expression is regulated by mTORC1 and correlates with the differentiation status of MPRO granulocytes. These data suggest that pharmacologic inhibition of mTORC1 by rapamycin can cooperate with a transcriptional differentiation program initiated by retinoids to regulate endogenous c-MYC expression and accelerate TMD.
Rapamycin reduces c-MYC protein by inhibition of translation of c-Myc mRNA
To investigate the mechanism by which rapamycin regulated c-MYC expression in granulocytes, we examined regulation of those processes required for gene expression: gene transcription, mRNA translation, and protein stability.
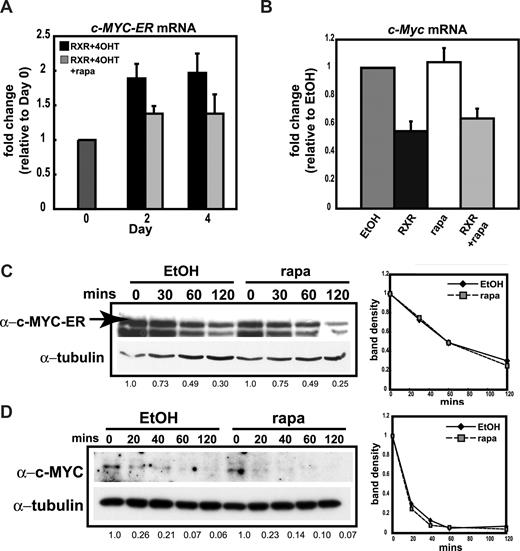
Using the inducible c-MYC-ER system, we measured mRNA abundance to determine whether rapamycin regulated the expression of c-MYC-ER mRNA. Using primers specific to the human c-MYC gene to distinguish c-MYC-ER from endogenous murine c-Myc mRNA, we assayed c-MYC-ER mRNA by qRT-PCR. c-MYC-ER mRNA abundance did not fall below the baseline level seen in day-0 c-MYC-ER MPROs, suggesting that constitutive expression of the fusion gene was maintained despite rapamycin treatment (Figure 5A). In addition, endogenous c-Myc mRNA levels in nontransduced MPROs were unaffected by rapamycin alone (Figure 5B). Conversely, treatment with RXR for 48 hours reduced c-Myc mRNA transcript abundance by approximately 50% in accordance with previous reports.65,66 Importantly, this retinoid-dependent reduction in c-Myc mRNA could not be augmented by treating the cells with rapamycin (Figure 5B). These data suggest that rapamycin regulates c-MYC expression at a posttranscriptional level.
Total c-Myc mRNA and c-MYC protein stability do not change in MPRO granulocytes treated with rapamycin. (A) Abundance of c-MYC-ER mRNA in c-MYC-ER MPRO cells induced to differentiate with 10−6 M AGN194204 and treated with 200 nM 4-hydroxytamoxifen (RXR + 4OHT) or 200 nM 4OHT and 80 nM rapamycin (RXR + 4OHT + rapa) was determined by qRT-PCR. Results were corrected for β-2-microglobulin transcript abundance and represented as fold change over untreated (day 0) cells. (B) Abundance of c-MYC mRNA was determined by qRT-PCR in MPRO cells treated with EtOH, 10−6 M AGN194204 (RXR), 80 nM rapamycin (rapa), or 10−6 M AGN194204 and 80 nM rapamycin (RXR + rapa). Results were corrected for β-2-microglobulin transcript abundance and represented as fold change relative to EtOH control. For panels A and B, data shown are the mean plus or minus SEM of 3 independent experiments. (C) c-MYC-ER MPRO cells were treated with 200 nM 4OHT and either EtOH or 80 nM rapamycin. Cycloheximide (10 μg/mL) was added to inhibit new protein synthesis and cells were harvested after 0, 30, 60, and 120 minutes. Protein lysates were analyzed for c-MYC-ER expression by Western blotting and α-tubulin was used as a loading control. To determine protein turnover, band densitometry was performed using ImageJ software. c-MYC-ER band density was corrected for α-tubulin and represented as fold change over time 0. Calculated band density normalized to time 0 is shown under the Western blot. (D) Cycloheximide (10 μg/mL) was added to MPRO cells treated with EtOH or 80 nM rapamycin. Lysates were generated from cells harvested at 0, 20, 40, 60, and 120 minutes. Endogenous c-MYC and α-tubulin levels were determined by Western blotting and quantitated by ImageJ software to determine protein turnover as described in panel C. Calculated band density for the gel pictured is shown under the Western blot. Quantitation in the right hand panel is the mean of 2 independent experiments.
Total c-Myc mRNA and c-MYC protein stability do not change in MPRO granulocytes treated with rapamycin. (A) Abundance of c-MYC-ER mRNA in c-MYC-ER MPRO cells induced to differentiate with 10−6 M AGN194204 and treated with 200 nM 4-hydroxytamoxifen (RXR + 4OHT) or 200 nM 4OHT and 80 nM rapamycin (RXR + 4OHT + rapa) was determined by qRT-PCR. Results were corrected for β-2-microglobulin transcript abundance and represented as fold change over untreated (day 0) cells. (B) Abundance of c-MYC mRNA was determined by qRT-PCR in MPRO cells treated with EtOH, 10−6 M AGN194204 (RXR), 80 nM rapamycin (rapa), or 10−6 M AGN194204 and 80 nM rapamycin (RXR + rapa). Results were corrected for β-2-microglobulin transcript abundance and represented as fold change relative to EtOH control. For panels A and B, data shown are the mean plus or minus SEM of 3 independent experiments. (C) c-MYC-ER MPRO cells were treated with 200 nM 4OHT and either EtOH or 80 nM rapamycin. Cycloheximide (10 μg/mL) was added to inhibit new protein synthesis and cells were harvested after 0, 30, 60, and 120 minutes. Protein lysates were analyzed for c-MYC-ER expression by Western blotting and α-tubulin was used as a loading control. To determine protein turnover, band densitometry was performed using ImageJ software. c-MYC-ER band density was corrected for α-tubulin and represented as fold change over time 0. Calculated band density normalized to time 0 is shown under the Western blot. (D) Cycloheximide (10 μg/mL) was added to MPRO cells treated with EtOH or 80 nM rapamycin. Lysates were generated from cells harvested at 0, 20, 40, 60, and 120 minutes. Endogenous c-MYC and α-tubulin levels were determined by Western blotting and quantitated by ImageJ software to determine protein turnover as described in panel C. Calculated band density for the gel pictured is shown under the Western blot. Quantitation in the right hand panel is the mean of 2 independent experiments.
Next, we tested whether c-MYC-ER protein stability was reduced after rapamycin treatment using cycloheximide to prevent nascent protein synthesis then following c-MYC-ER protein levels by Western blotting. There was no detectable difference in the turnover of c-MYC-ER between control- and rapamycin-treated cells when protein levels were quantitated by densitometry (Figure 5C). Furthermore, c-MYC-ER levels still decreased in rapamycin-treated MPRO cells expressing the ER fusion of the MYCT58A point mutant known to increase protein stability, suggesting the effect of rapamycin on c-MYC protein levels is independent of turnover mechanisms regulated by phosphorylation of c-MYC at T58 (Figure S1). Moreover, rates of endogenous c-MYC protein turnover in nontransduced MPROs were unchanged after rapamycin treatment (Figure 5D). These results exclude reduced protein stability as a mechanism for modulation of c-MYC expression in rapamycin-treated MPROs.
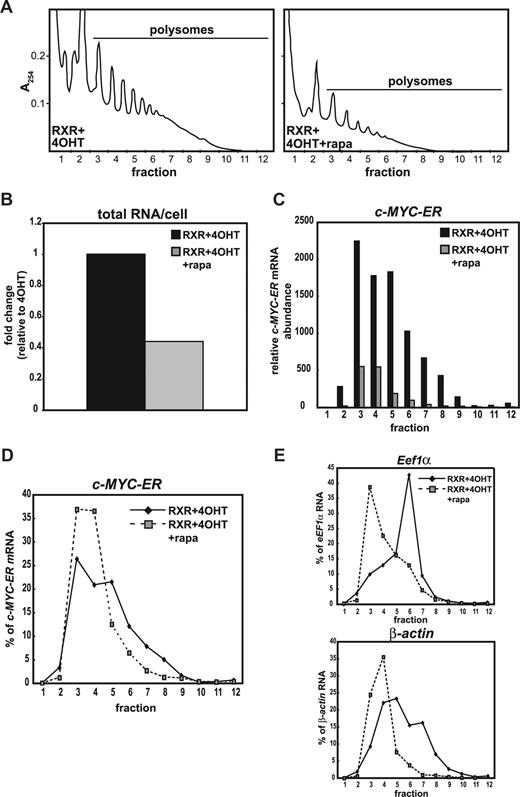
Our results demonstrated that the reductions in c-MYC expression in differentiating granulocytes observed after rapamycin treatment did not result from attenuation of gene transcription or decreased protein stability. Accordingly, we examined c-Myc mRNA translation after rapamycin treatment. mTORC1 activity has been shown to be required for efficient translation of mRNAs with complex 5′ UTRs such as c-Myc and Eef1α as well as mRNAs that lack 5′ regulatory sequences such as Actin.67-70 Thus, rapamycin treatment induces the redistribution of these mRNAs from heavier, actively translated polysomes to lighter monosomes and disomes. Sucrose density gradient centrifugation of cell extracts was used to separate monosomes and disomes from polysomes. First, we analyzed sucrose gradients performed on cell extracts from c-MYC-ER cells treated for 4 days with RXR, 4OHT, and either rapamycin or vehicle control to investigate changes in c-MYC-ER mRNA translation. The amount of RNA per fraction was determined by continuous A254 monitoring during the separation process. Profiles obtained from fractionated cell lysates showed an obvious reduction in cellular polysome content after rapamycin treatment (Figure 6A). Consistent with the A254 profiles, there was an approximately 50% reduction in total RNA content per cell (Figure 6B). These global changes in RNA were accompanied by a dramatic fall in absolute abundance of both monosomal and polysomal c-MYC-ER transcripts per cell after rapamycin treatment (Figure 6C). In addition, rapamycin induced a clear shift of c-MYC-ER transcripts from the actively translating polysomes to lighter, less active polysomes (Figure 6D), despite the pBabe c-MYC-ER construct lacking the 5′ regulatory structure characteristic of endogenous c-Myc. This translational regulation of c-MYC-ER mRNA by rapamycin was comparable to that observed for both Eef1α and for β-actin mRNA that lacks 5′ regulatory sequence (Figure 6E), consistent with changes in the distribution of transcripts lacking a regulatory 5′ UTR after prolonged rapamycin treatment reported by others.67-71 These data suggest that rapamycin negatively regulates translation of c-MYC-ER mRNA.
Rapamycin reduces c-MYC-ER mRNA translation in differentiating MPRO c-MYC-ER granulocytes. (A) Polysome profiles generated from lysates of AGN194204 (RXR)–treated MPRO c-MYC-ER cells treated with 200 nM 4-hydroxytamoxifen (RXR + 4OHT) or 200 nM 4OHT and 80 nM rapamycin (RXR + 4OHT + rapa) for 4 days and normalized by loading equal cell number. (B) Total RNA per cell was measured using a NanoDrop ND-1000 UV-Vis Spectrophotometer (NanoDrop Technologies, Wilmington, DE). (C) Abundance of c-MYC-ER mRNA per fraction determined by qRT-PCR in c-MYC-ER–expressing MPRO cells treated as described in panel A. Values are normalized to c-MYC-ER mRNA abundance in fraction 1 for MPRO c-MYC-ER cells treated with 4OHT. (D,E) Distribution of Eef1α, β-actin, and c-MYC-ER mRNA in fractionated lysates was determined by qRT-PCR. For each individual transcript, results are expressed as the percentage of the sum of the transcript mRNA present in 12 fractions. Data in panels A through E are from a single representative experiment.
Rapamycin reduces c-MYC-ER mRNA translation in differentiating MPRO c-MYC-ER granulocytes. (A) Polysome profiles generated from lysates of AGN194204 (RXR)–treated MPRO c-MYC-ER cells treated with 200 nM 4-hydroxytamoxifen (RXR + 4OHT) or 200 nM 4OHT and 80 nM rapamycin (RXR + 4OHT + rapa) for 4 days and normalized by loading equal cell number. (B) Total RNA per cell was measured using a NanoDrop ND-1000 UV-Vis Spectrophotometer (NanoDrop Technologies, Wilmington, DE). (C) Abundance of c-MYC-ER mRNA per fraction determined by qRT-PCR in c-MYC-ER–expressing MPRO cells treated as described in panel A. Values are normalized to c-MYC-ER mRNA abundance in fraction 1 for MPRO c-MYC-ER cells treated with 4OHT. (D,E) Distribution of Eef1α, β-actin, and c-MYC-ER mRNA in fractionated lysates was determined by qRT-PCR. For each individual transcript, results are expressed as the percentage of the sum of the transcript mRNA present in 12 fractions. Data in panels A through E are from a single representative experiment.
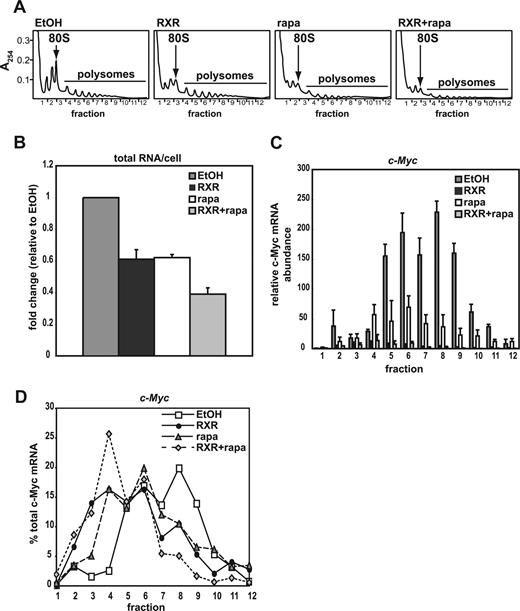
We next examined native c-Myc that contains functional 5′ regulatory sequences. A254 profiles generated from fractionated MPRO cell lysates showed a reduction in 80S ribosome content per cell after treatment with RXR alone compared with vehicle-treated undifferentiated promyelocytes, suggesting that cellular ribosome content changes during TMD in MPROs. Rapamycin alone resulted in a similar reduction in 80S ribosome content and an additional reduction in polysome content. Combination treatment with RXR and rapamycin further reduced both 80S ribosome and polysome content over single-agent treatment (Figure 7A). In keeping with changes in the polysome profiles, single-agent treatment with RXR or rapamycin decreased total RNA per cell by approximately 40%, whereas combination treatment led to a more marked approximately 60% drop (Figure 7B). These data suggest that rapamycin acts individually and cooperates with retinoids to limit ribosome number per cell. Measurement of c-Myc mRNA per fraction after single-agent rapamycin treatment revealed a reduction in c-Myc transcript across all fractions relative to control cells (Figure 7C) consistent with reduced ribosome capacity in response to mTORC1 inhibition. RXR treatment alone showed a greater reduction in c-Myc mRNA per fraction, representing net changes in gene transcription and ribosome capacity (Figures 5B and 7C). Treatment of MPRO granulocytes with rapamycin alone or induction of differentiation with RXR alone also led to a relocation of c-Myc mRNA from actively translating polysomes to the subpolysomal fractions (Figure 7D). Interestingly, combination RXR and rapamycin treatment resulted in a more pronounced redistribution of c-Myc mRNA to lighter less actively translated fractions (Figure 7C,D). Since the addition of rapamycin to RXR does not alter total c-Myc mRNA abundance in MPROs (Figure 5B), we conclude that the additional reduction in polysomal c-Myc mRNA observed after combination treatment with RXR and rapamycin resulted from inhibition of c-Myc mRNA translation by rapamycin. This finding implies an additional effect of RXR on c-Myc mRNA translation beyond rapamycin inhibition of cap-dependent translational initiation and the formation of the 48S initiation complex. To examine whether RXR treatment could also effect formation of the 80S initiation complex containing c-Myc mRNA, the sucrose density gradient conditions were optimized to separate 40S, 60S, and 80S complexes as determined by of the 28S/18S rRNA ratio (Figure S3A,B). The relative distribution of c-Myc mRNA in these fractions (Figure S3C) was compared with the distribution of the cap-regulated mRNA transcript Eef1α (Figure S3D). Combination of rapamycin and RXR resulted in an increased proportion of c-Myc mRNA in 80S ribosomes, rather than smaller particles, indicating both agents regulated translational initiation. Interestingly, rapamycin increased the proportion of Eef1α mRNA on subribosomal particles as well as 80S ribosomes, perhaps reflecting the different 5′ UTRs of the 2 mRNAs. Overall, measures of total cellular mRNA, polysomal mRNA, and protein stability show that rapamycin reduces both c-MYC-ER and endogenous c-MYC expression in differentiating MPRO granulocytes at the level of mRNA translation.
Rapamycin inhibits endogenous c-Myc mRNA translation in MPRO granulocytes. (A) Polysome profiles generated from cell lysates obtained from MPRO cells treated with 48 hours of EtOH (undifferentiated vehicle control), 10−6 M AGN194204 (RXR), 80 nM rapamycin (rapa), or 10−6 M AGN194204 and 80 nM rapamycin (RXR + rapa) normalized by loading equal cell number. (B) Total RNA per cell was measured using a NanoDrop ND-1000 UV-Vis Spectrophotometer. (C) c-MYC mRNA abundance per fraction was determined by qRT-PCR in MPRO cells treated as described in panel A. Values are normalized to c-Myc mRNA abundance in fraction 1 for EtOH-treated cells. Data shown are the mean plus or minus SEM of 3 independent experiments. (D) Distribution of c-Myc mRNA in fractionated lysates was determined by qRT-PCR. Average transcript abundance in each fraction was divided by average net transcript abundance in all fractions and expressed as a percentage of total for the 3 experiments included in panel C.
Rapamycin inhibits endogenous c-Myc mRNA translation in MPRO granulocytes. (A) Polysome profiles generated from cell lysates obtained from MPRO cells treated with 48 hours of EtOH (undifferentiated vehicle control), 10−6 M AGN194204 (RXR), 80 nM rapamycin (rapa), or 10−6 M AGN194204 and 80 nM rapamycin (RXR + rapa) normalized by loading equal cell number. (B) Total RNA per cell was measured using a NanoDrop ND-1000 UV-Vis Spectrophotometer. (C) c-MYC mRNA abundance per fraction was determined by qRT-PCR in MPRO cells treated as described in panel A. Values are normalized to c-Myc mRNA abundance in fraction 1 for EtOH-treated cells. Data shown are the mean plus or minus SEM of 3 independent experiments. (D) Distribution of c-Myc mRNA in fractionated lysates was determined by qRT-PCR. Average transcript abundance in each fraction was divided by average net transcript abundance in all fractions and expressed as a percentage of total for the 3 experiments included in panel C.
Discussion
This paper demonstrates that mTORC1 inhibition cooperates with retinoids to promote TMD by posttranscriptional regulation of c-MYC. In the MPRO model, total cellular c-Myc mRNA and c-MYC protein stability were unchanged by rapamycin, however the amount of polysomal c-MYC mRNA and c-MYC protein were reduced. These data indicate that rapamycin regulated c-MYC expression by controlling c-Myc mRNA translation. The importance of translational regulation was emphasized by the finding that translational control of c-MYC by rapamycin restored differentiation to granulocytes rendered refractory to differentiation by enforced expression of c-MYC.
Our findings are consistent with previous studies demonstrating down-regulation of the PI3K/AKT/mTORC1 pathway in differentiating granulocytes in response to retinoids72-74 (and M.W. and G.A.M., unpublished data, February, 2004). Furthermore, inhibition of mTORC1 by rapamycin alone can promote the differentiation of several myeloid leukemia cell lines,75 and enhances differentiation in the myeloid leukemia–derived HL-60 cell line in concert with DMSO, G-CSF,76 or with all-trans-retinoic acid (ATRA).77 Subsequently Kanayasu-Toyoda et al showed that rapamycin reduced expression of c-MYC in the HL-60 cells demonstrating enhanced differentiation.78 Importantly, MPRO cells are immortalized promyelocytes derived from normal murine bone marrow that undergo more complete differentiation in response to retinoids,79 extending the relevance of mTORC1-dependent regulation of differentiation to nontransformed cells. In addition, we show that regulation of c-Myc mRNA translation is an important mechanism for the enhanced differentiation phenotype resulting from mTORC1 inhibition in MPROs.
There are multiple mechanisms for c-MYC regulation by PI3K/AKT/mTORC1 including the regulation of c-Myc mRNA stability,80 and translation,70,81 and c-MYC protein stability.82 The mechanism used likely reflects cellular context. Granulocytes, a cell type strongly programmed to dismantle their protein synthetic machinery during differentiation, may be particularly sensitive to interventions that limit ribosome biogenesis to influence differentiation.
The 5′ UTR of c-Myc mRNA contains a complex secondary structure that limits the efficiency of cap-dependent translation; it also contains an internal ribosome entry site (IRES) that permits initiation of translation in a cap-independent manner, particularly in response to cellular stress, for example, during apoptosis,83,84 mitosis85 or genotoxic stress.86 Kobayashi et al87 studied regulation of c-Myc mRNA translation in myeloid leukemia cells; the authors reported that addition of cytokines to growth factor–deprived cells resulted in up-regulation of c-Myc mRNA translation via an IRES-mediated mechanism that was resistant to rapamycin. In our studies, only the treatment of differentiating cells with rapamycin resulted in an effect on c-Myc mRNA translation with functional consequences for the cells, suggesting parallel modes of action for RXR and rapamycin. Interestingly, mTORC1 inhibition enhanced the reductions in ribosome capacity induced by differentiation of granulocytes with retinoids as well as the redistribution of native c-Myc transcripts away from heavy polysomes. It may be that once translation capacity falls below a critical threshold, competition for ribosomes becomes acute, resulting in less efficient trans-lation of c-Myc mRNA by both cap-dependent and cap-independent (IRES) mediated mechanisms.
We performed a detailed analysis of the subpolysomal sucrose density gradient fractions to better delineate steps in the process of c-Myc mRNA translation most affected by rapamycin in our myeloid differentiation model. Accumulation of c-Myc transcripts in the 80S-containing fraction in preference to the subribosomal fractions suggests the predominant action of rapamycin is inhibition of translation initiation and not inhibition of joining of the 60S ribosome to the 48S preinitiation complex. In support of this conclusion, a similar pattern of transcript accumulation on 80S ribosomes was observed for Eef1α and rapamycin is known to inhibit its translation initiation in a cap-dependent fashion.32 Subtle differences in transcript distribution patterns for c-Myc and Eef1α in the subpolysomal fractions may reflect the makeup of their respective 5′ UTRs, that is, the cap and IRES in c-Myc mRNA versus the 5′ TOP sequence in the Eef1α cap. However, our experiments do not allow us to draw any conclusions about the effect of rapamycin on IRES-mediated translation of c-Myc mRNA during retinoid-induced TMD.
These data show that changes in ribosome number and function can lead to significant alterations in the expression of dynamically regulated proteins that alter growth and proliferation such as c-MYC. We cannot exclude the possibility that expression of other important genes is also subject to translational regulation by mTORC1 in a manner analogous to c-MYC. Comparing polysomal mRNA to total cellular mRNA using microarray technology to identify retinoid- and mTORC1-dependent translationally regulated transcripts will be important in order to define additional key mediators of TMD.
Dysregulated expression of c-MYC is a frequent event in AML and may contribute to the aberrant differentiation that is a hallmark of this condition. Overactivity of the PI3K/AKT/mTOR pathway has also been reported to be frequent in AML.88-91 Therefore, AML may be particularly amenable to therapies that inhibit cell growth and/or result in altered differentiation potential. One of the most successful innovations in the treatment of myeloid malignancies has been the use of ATRA to differentiate blasts in acute promyelocytic leukemia resulting in improved cure rates.92-94 Preliminary preclinical data and results of early phase clinical trials in AML have demonstrated encouraging single-agent activity for rapamycin, and its analogues everolimus and temsirolimus.89,95-97 Later phase clinical trials of mTORC1 inhibitor therapy in AML are ongoing. As we observed cooperation between retinoids and rapamycin, our results predict that mTORC1 inhibition may have enhanced efficacy in malignant granulocytes when used in combination with therapies designed to reinstitute transcriptional programs of differentiation, for example, retinoids or epigenetic regulators of gene expression such as HDAC inhibitors or hypomethylating agents. More generally, the ability of rapamycin to modulate c-MYC expression and rescue MYC-driven phenotypes suggests that mTORC1 may offer the ability to intervene downstream of c-MYC transcription to modulate c-MYC activity in malignancies where transcriptional regulation over c-MYC expression has been lost.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
Many thanks to Carl R. Walkley for helpful discussion and for generating MPRO c-MYC-ER cell lines, and to Nelly Conus for helpful discussions.
This work was supported in part by grants from the National Health and Medical Research Council (Canberra, Australia) (G.A.M., R.B.P., and R.D.H.). M.W. is a recipient of a Cancer Council Victoria Postgraduate Scholarship and G.A.M. is a recipient of a Cancer Council of Victoria Sir Edward Weary Dunlop Clinical Research Fellowship.
Authorship
Contribution: M.W. and G.P. designed and performed research, analyzed data, and wrote the paper; and K.M.H., R.B.P., and R.D.H. analyzed data and wrote the paper; and G.A.M. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: M.W. has acted as a consultant for Novartis (Basel, Switzerland); G.A.M. has acted as a consultant for and received honoraria and research support from Novartis. All other authors declare no competing financial interests.
Correspondence: Grant McArthur, Research Division, Peter MacCallum Cancer Centre, Locked Bag 1, A'Beckett Street, Melbourne Victoria 8006, Australia; e-mail: grant.mcarthur@petermac.org.