Abstract
Although immunoglobulin VH mutation status (IgVH MS) is prognostic in patients with chronic lymphocytic leukemia (CLL) who are treated with alkylating agents or single-agent fludarabine, its significance in the era of chemoimmunotherapy is not known. We determined the IgVH somatic mutation status (MS) in 177 patients enrolled in a phase 2 study of fludarabine, cyclophosphamide, and rituximab (FCR) and in 127 patients treated with subsequent chemoimmunotherapy protocols. IgVH MS did not impact significantly on the complete remission (CR) rate of patients receiving FCR or related regimens. However, CR duration was significantly shorter in patients with CLL that used unmutated IgVH than those whose CLL used mutated IgVH (TTP 47% vs 82% at 6 years, P < .001). In a multivariate model considering all baseline characteristics, IgVH MS emerged as the only determinant of remission duration (hazard ratio 3.8, P < .001). Our results suggest that postremission interventions should be targeted toward patients with unmutated IgVH status.
Introduction
Immunoglobulin VH somatic mutation status (IgVH MS) is an important prognostic marker in patients with chronic lymphocytic leukemia (CLL). In the chemotherapy era, patients with cells that used an unmutated IgVH gene (UM-CLL) had inferior rates of survival compared with those that used a mutated IgVH gene (M-CLL).1,2 However, it was unclear whether this difference was because of inferior treatment response, increased risk of relapse from remission, or both. Furthermore, it is not known whether IgVH MS remains relevant in patients treated with combinations of chemotherapy and monoclonal antibodies (chemoimmunotherapy).3,4 To address these questions, we analyzed the impact of IgVH MS on the outcome of patients treated with frontline chemoimmunotherapy at our center.
Methods
The University of Texas M. D. Anderson Cancer Center Institutional Review Board approved the studies included in this report, and informed consent was obtained in accordance with the Declaration of Helsinki. The main analysis was based on 300 patients treated with the phase 2 study of the fludarabine, cyclophosphamide, rituximab (FCR) regimen, which had a mature median follow-up of 6 years. The complete remission (CR) rate was 72%, and the time to progression (TTP) for complete responders was 85 months; 6-year overall survival (OS) for all patients was 77%.3,4 Subsequent to the FCR study, our center evaluated several other chemoimmunotherapy regimens: FCR3 (FCR with 3 rituximab doses per cycle, n = 56),5 FCMR (FCR with mitoxantrone, n = 24),6 FCR plus granulocyte macrophage colony-stimulating factor (GMCSF; n = 21), and CFAR (FCR with alemtuzumab, n = 26).7 These protocols were single-arm studies with differences in baseline characteristics; however, they were conducted in patients with CLL commencing initial chemotherapy according to uniform criteria,8 and patients underwent response staging in an identical manner.8 Therefore, studies subsequent to FCR were included to provide additional insight into the impact of IgVH MS on CR achievement. The impact of IgVH MS on TTP and OS was not evaluable in these studies because of the short median follow-up (35, 26, 12, and 8 months for FCR3, FCMR, CFAR, and FCR + GMCSF, respectively).
For patients treated with FCR, IgVH MS was determined retrospectively in 101 patients from pretreatment formalin-fixed, paraffin-embedded bone marrow aspirate clot section samples and prospectively in 76 patients from fresh peripheral blood or bone marrow samples. The remaining 123 patients had insufficient specimens for analysis. All patients in protocols subsequent to FCR had their IgVH mutation status (MS) determined prospectively from fresh tissue. The technique for testing in fresh tissue was according to published methods.9
The technique for paraffin-embedded tissue was as follows: DNA was extracted from paraffin-embedded tissue section with the DNeasy Blood and Tissue Kit (QIAGEN, Hilden, Germany) and amplified with HotStar Taq DNA Polymerase (QIAGEN) and FRc1 primer set, as described previously.10 Amplified monoclonal bands were detected on 1.5% agarose gel, excised, and extracted with use of the QIAquick Gel Extraction Kit (QIAGEN). The purified DNA was subjected to sequence analysis. The mutation status was designated as unmutated (UM-CLL) if we detected fewer than 2.0% mutations (> 98.0% homology to germline sequences) or as mutated (M-CLL) if we detected 2.0% or greater mutations (≤98.0% homology to germline sequences) compared with the germline sequences in VBASE2 (www.vbase2.org).11
TTP and OS were calculated from the date of therapy until disease progression and death, respectively. Because most (> 70%) patients achieved CR, and to obtain as homogenous a group of patients as possible, the analysis of the impact of IgVH MS on TTP was restricted to complete responders only. Categorical variables were compared by use of the χ2 or Fisher exact test, and continuous variables were compared by use of the Mann-Whitney test. Survival distributions were compared with the log-rank test and Cox regression, as appropriate. The number of FCR patients analyzed were sufficient to detect with 85% power (at a 1-sided significance level of P = .05), an absolute difference of 20% or more in CR rate favoring patients with M-CLL. The 20% threshold was regarded by our treating physicians as being clinically relevant. All other P values were 2-sided.
Results and discussion
IgVH MS was available in 177 FCR patients, with 59% having UM-CLL and 41% having M-CLL (Table 1). Their baseline characteristics and treatment outcome were not significantly different from that of FCR patients whose IgVH MS was not determined (P > .20 for all comparisons, data not shown). Clinical data from 127 patients treated on protocols subsequent to FCR were pooled (Table 1) to examine for differences between patients with UM-CLL (69%) and M-CLL (31%). In general, patients with UM-CLL were more likely to have a high white cell count, elevated β2-microglobulin (β2m), and/or abnormal conventional karyotypic or adverse fluorescence in situ hybridization findings (Table 1).
Among FCR patients, CR rates were similar between UM-CLL and M-CLL patients, being 73% and 83%, respectively (P = .12). The proportions of patients achieving flow cytometry–negative CR (defined as < 1% CD5/19 coexpressing cells in the marrow lymphoid gate, with normal light chain ratio) were 57% and 67%, respectively (P = .21). This result was reproduced in patients treated on protocols subsequent to FCR, where the CR rates were similar between UM-CLL and M-CLL patients both as a group (71% vs 78%, respectively; P = .46), and within individual regimens (Table 1). Within this group, the proportions of UM-CLL and M-CLL patients achieving flow cytometry–negative CR were 54% and 69%, respectively (P = .16). Thus, IgVH MS did not substantially influence the probability of achieving CR.
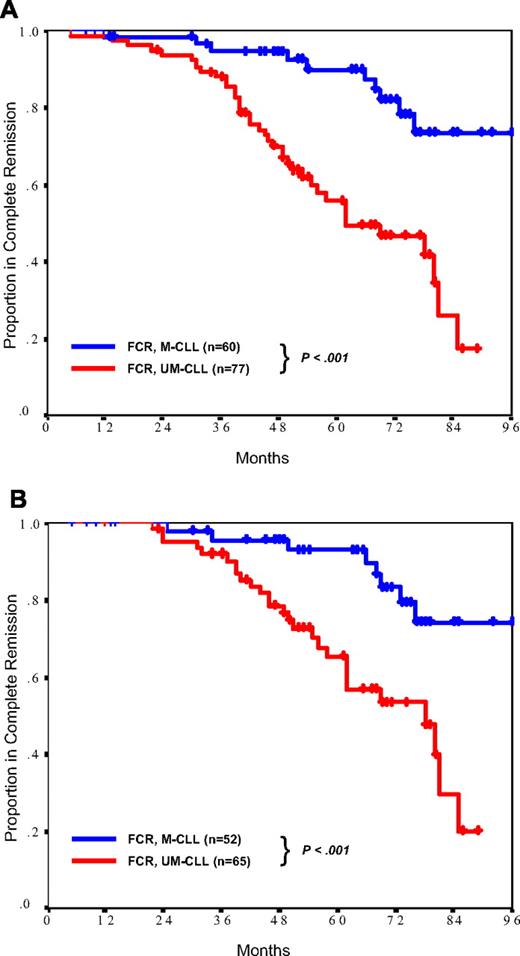
In the analysis of CR duration in FCR patients, however, UM-CLL patients who entered CR were found to have a significantly inferior TTP compared with M-CLL patients (Figure 1A). At 6 years, the proportions of complete responders remaining progression free were 47% and 82% for UM-CLL and M-CLL patients, respectively (P < .001). Among M-CLL patients, those using the VH3-21 gene were at an increased risk of relapse (3 relapses in 6 patients) compared with those using other VH subfamilies (7 relapses in 54 patients, P = .05). This effect of IgVH MS on TTP was maintained when the analysis was restricted only to complete responders with confirmed flow cytometric negativity (Figure 1B). Multivariate analysis was performed to determine whether the significance of IgVH MS was independent of prognostic factors previously established in the FCR population.4 In this analysis, IgVH MS status was strongly and independently significant for TTP (hazard ratio 3.8, P < .001), whereas established factors (including age, β2m, cytogenetic abnormalities, white cell count, marrow CD38 positivity, and interval between diagnosis and treatment) failed to reach statistical significance.
Duration of complete remission. In the FCR cohort, patients with CLL cells that used mutated IgVH (M-CLL) had significantly longer complete remission duration than did patients with CLL cells that used unmutated IgVH (UM-CLL), despite similar proportions achieving complete remission. This effect was present both in the total population of complete responders (A) and in complete responders with negative marrow flow cytometry (B).
Duration of complete remission. In the FCR cohort, patients with CLL cells that used mutated IgVH (M-CLL) had significantly longer complete remission duration than did patients with CLL cells that used unmutated IgVH (UM-CLL), despite similar proportions achieving complete remission. This effect was present both in the total population of complete responders (A) and in complete responders with negative marrow flow cytometry (B).
Considering all patients treated with FCR, 6-year OS was significantly inferior in UM-CLL compared with M-CLL patients (71% and 82%, respectively; P = .05). However, on multivariate analysis, IgVH MS was not independently associated with inferior OS (P = .10), whereas advancing age (P = .001) and high β2m (P = .006) were significant.
This study demonstrated that the prognostic impact of IgVH MS in patients receiving chemoimmunotherapy regimens was not related to differences in CR rates but was caused by aggressive relapse kinetics in patients with UM-CLL. The reason for this effect is uncertain and may be related to differential responses to B-cell receptor signaling.12 These data are highly relevant to clinical investigators because they suggest that studies of postremission interventions (eg, maintenance therapy, early relapse detection strategies, use of novel agents in remission) should be targeted toward those patients with UM-CLL, because these are the patients at the greatest risk of early relapse. Patients with CLL which use the VH3-21 gene should be managed as if they have UM-CLL.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: K.I.L. performed the IgVH mutation determination in paraffin-embedded tissue and wrote the paper; C.S.T. analyzed the data and coauthored the manuscript; M.J.K. and L.V.A. designed the study and provided supervision and advice in data analysis and manuscript preparation; T.J.K. and L.R. performed the IgVH mutation determination in fresh tissue and provided advice and oversight in manuscript preparation; K.R.C. performed the sample size analysis and provided statistical oversight; E.S. and L.L.B. assisted in the sample preparation and provided technical advice; W.G.W., S.O., A.F., S.F., and H.K. contributed and verified the accuracy of patient data and provided advice and oversight on data analysis and manuscript preparation; and S.L. collected the patient data and coordinated the verification of data integrity.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Michael J. Keating, M.B.B.S., Leukemia Department, Unit 428, The University of Texas M. D. Anderson Cancer Center, 1515 Holcombe Blvd, Houston, TX 77030; e-mail: mkeating@mdanderson.org.