Abstract
We have previously shown that intratumoral injection of CpG oligodeoxynucleotide plus systemic chemotherapy can induce a T-cell immune response against lymphoma and serve as a therapeutic vaccine to cure tumors in a murine model. Here, we demonstrate that antibody-mediated modulation of T cells increases the efficacy of CpG vaccination, thereby eliminating the need for chemotherapy. T-cell modulation was accomplished by targeting both effector and regulatory T-cell populations using systemic administration of monoclonal antibodies against OX40, CTLA4, GITR, and folate receptor 4 (FR4). Each of these antibodies enhanced the effect of intratumoral CpG. Some pairwise combinations of these antibodies potentiated T-cell modulation and further enhanced the efficacy of CpG vaccination. Specifically, the combination of anti-OX40 and anti-CTLA4 which enhance activation and block cell-intrinsic negative regulatory circuits in T cells, respectively, was especially potent. When combined with intratumoral CpG, it induced antitumor CD4 and CD8 T-cell immunity, cured large and systemic lymphoma tumors without chemotherapy, and provided long-lasting immunity against tumor rechallenge. Our results show that the combination of intratumoral CpG and immunomodulatory T-cell antibodies has promise for therapeutic vaccination against lymphoma. These reagents are becoming available for human clinical trials.
Introduction
Lymphoma is a malignancy which is responsive to immunotherapy.1 Despite the success of passive immunotherapy with monoclonal antibodies (eg anti-CD20, rituximab), many patients with lymphoma remain incurable. Therapeutic vaccines against lymphoma might elicit long-lasting antitumor immune responses and prevent or prolong the time to recurrence. Most recently, our group has shown that intratumoral injection of CpG, in combination with systemic chemotherapy, can serve as a therapeutic vaccine to eradicate large and metastatic lymphoma tumors.2 CpG oligodeoxynucleotides (ODNs) are ssDNA fragments containing immune stimulatory unmethylated C-G sequence motifs similar to those found in microbes, capable of activating dendritic cells (DCs) and B cells by engaging Toll-like receptor 9.3 In our model, intratumoral injection of CpG can directly activate tumor-infiltrating DCs as well as tumor B cells to force tumor-antigen presentation in situ.2 In addition, CpG can directly inhibit proliferation of tumor cells in contrast to their proliferative and antiapoptotic effects on normal B cells.2
This vaccine strategy has several advantages. First, it does not require in vitro manipulation and can thus be made available to large numbers of patients. Second, the therapy is personalized since the patients will be immunized against their own tumor antigens (Ag). Third, this therapy does not hinge on a single tumor antigen, thus, multiple tumor antigens may be targeted, reducing the risk that the tumor will be able to evade the immune response.
In this study, we hypothesized that antibody-mediated modulation of T-cell populations would increase the efficacy of CpG vaccination, thereby eliminating the need for chemotherapy. Indeed, we have previously shown that the antitumor effect of CpG vaccination is T-cell mediated.2 Moreover, antitumor T cells may be rendered inefficient due to tumor-induced immunosuppression.4 We postulated that T-cell modulation would amplify the antitumor response and overcome these immunosuppressive mechanisms, leading to enhanced efficacy of CpG vaccination. T-cell modulation was accomplished by systemic administration of monoclonal antibodies (mAb) against both effector and CD4+CD25+ regulatory T-cell (Treg) populations.
T-cell modulation aimed at enhancing antitumor immunity can be accomplished in 3 ways: (1) by stimulating antitumor T cells directly, (2) by blocking intrinsic negative T-cell signals, or (3) by eliminating Treg cells that typically dampen antitumor immune responses. Following MHC-TCR engagement (signal 1), additional signals from costimulatory receptors (signal 2) are required for T-cell activation.5 One of these receptors, OX40 (CD134) is expressed on activated but not resting T cells and its engagement leads to increased proliferation and survival of these cells.6 Conversely, cytotoxic T-lymphocyte–associated antigen (CTLA4, also known as CD152)7,8 is a cell intrinsic negative regulator of activated T cells which suppresses T-cell activity by binding to the B7 molecules, CD80 and 86. Therefore, enhancing activation of effector T cells can be achieved by stimulating OX40 with an agonist mAb or by blocking CTLA4 with an antagonist mAb. Treg cells are another target for antibody-mediated T-cell modulation. Folate-receptor 4 (FR4) is constitutively and preferentially expressed by Treg cells and mAb directed against this receptor can be used to specifically deplete Treg cells while sparing effector T cells.9 Glucocorticoid-induced TNF-related protein (GITR) is another potential Treg target. This receptor is constitutively expressed on Treg cells and is up-regulated following T-cell activation.10 Signaling through GITR has been shown to both abrogate the suppressive functions of Treg cells and also serve as a costimulatory molecule for effector T cells.11 Therefore, Treg cells can be effectively depleted with anti-FR4 mAb9 or can be functionally inhibited with anti-GITR mAb.12 In addition to its effect on effector T cells, triggering of OX40 has also been shown to block Treg cell suppression.13-15
Using a 2-tumor site model to evaluate the systemic effects of this immunotherapy, we show that antibody-mediated T-cell modulation can greatly enhance the efficacy of intratumoral CpG vaccination against lymphoma and thus cure large and systemic tumors without the need for chemotherapy.
Methods
Reagents
CpG 1826 5′-TCCATGACGTTCCTGACGTT (the bold nucleotides represent the immunomodulatory CpG sequences) was provided by Coley Pharmaceutical Group (Ottawa, ON). In vivo systemic administration of monoclonal antibodies against T-cell targets was performed by intraperitoneal injections on days 1 and 5 of treatment. Anti-OX40 (CD134) mAb (rat IgG1, clone OX86; European Collection of Cell Cultures, Salisbury, United Kingdom), anti-CTLA4 (CD152) mAb (hamster IgG, clone 9H10; kind gift from Dr J. Allison, Memorial Sloan-Kettering Cancer Center, New York, NY), anti-GITR mAb (rat IgG2b, clone DTA-1; kind gift from Dr S. Sakaguchi, Kyoto University, Kyoto, Japan), and anti-FR4 mAb (rat IgG2a, clone TH6; kind gift from Dr S. Sakaguchi) were produced from ascites in severe combined immunodeficient (SCID) mice. None of the targeted molecules (OX40, CTLA4, GITR, FR4) is expressed on the surface of A20 tumor cells (data not shown).
Cell line and mice
The A20 cell line, a BALB/c B cell lymphoma expressing MHC class I and class II H-2d molecules, was obtained from the ATCC (Manassas, VA). Tumor cells were cultured in RPMI 1640 medium (Invitrogen Life Technologies, Carlsbad, CA) supplemented with 10% heat-inactivated FCS (HyClone Laboratories, Logan, UT), 100 U/mL penicillin, 100 μg/mL streptomycin (both from Invitrogen Life Technologies), and 50 μM 2-ME (Sigma-Aldrich, St Louis, MO), as complete medium. Cells were grown in suspension culture at 37°C in 5% CO2.
Female BALB/c mice (8 to 10 weeks old) were purchased from Charles River Laboratories (Wilmington, MA) and were housed at the Laboratory Animal Facility at the Stanford University Medical Center (Stanford, CA). CD8 knockout (KO) mice on the BALB/c background were provided by Dr C.G. Fathman (Stanford University School of Medicine). All experiments were conducted in accordance with Stanford University Animal Facility and National Institutes of Health (NIH) guidelines.
Tumor transplantation and immunotherapy
A20 lymphoma cells were implanted into 8- to 10-week-old female BALB/c mice at a dose of 5 × 106 cells in 50 μL RPMI by the subcutaneous route into 2 separate sites on the right and left side of the abdomen. Treatment began when tumors reached 5 mm to 7 mm in largest diameter, which typically occurred at days 5 to 7 after tumor inoculation. CpG was given intratumorally into one tumor site at a dose of 100 μg in a volume of 50 μL for each of 5 consecutive days (days 1 to 5 of treatment). Each antibody used for T-cell modulation was given intraperitoneally on days 1 and 5 of treatment at what is generally considered to be the optimal dose according to prior publications:9,12,16,17 400 μg per injection for anti-OX40, 100 μg per injection for anti-CTLA4, 500 μg per injection for anti-GITR, and 100 μg per injection for anti-FR4. Treg depletion following anti-FR4 treatment was confirmed by flow cytometry using anti-CD25 (BD Biosciences, San Jose, CA) and anti-FoxP3 (eBioscience, San Diego, CA) antibodies, typically showing more than 60% depletion, comparable to previous publication.9 The growth of tumor was monitored by a caliper twice a week, and expressed as length by width in square centimeters. Mice were killed when tumor size reached 4 cm2 or when tumor sites ulcerated.
Detection of tumor reactive T cells and Treg cells
Mice were killed 4 days after the end of treatment; spleens and tumors were harvested separately and made into single-cell suspensions, and the red blood cells were lysed. A total of 5 × 105 splenocytes or cells from the tumor were cocultured with 5 × 105 irradiated A20 cells plus anti-CD28 Ab (5 μg/mL, BD Biosciences) for 24 hours at 37°C and 5% CO2. Monensin was added during the last 5 hours of culture. Afterward, cells were washed and surface stained with anti-CD8 FITC, anti-CD4 PerCP, and anti-CD44 APC (BD Biosciences). Intracellular IFN-γ expression was assessed using BD Cytofix/Cytoperm kit (catalog no. 554722) per instructions, and BD anti–IFN-γ PE-conjugated Ab. Treg cells from the freshly isolated tumors were stained with anti-CD4 PE (BD Biosciences), anti-CD25 FITC (BD Biosciences), and anti-FoxP3 APC (eBioscience) using eBioscience Cytofix/Cytoperm kit. Cells were studied by flow cytometry on a BD FACSCalibur and analyzed using FlowJo (TreeStar, Ashland, OR) or Cytobank (http://cytobank.stanford.edu/public).
Depletion of CD4 and CD8 T cells
Ascitic fluid was harvested from SCID mice bearing hybridoma GK1.5 and 2.43 producing anti-CD4 (rat IgG2b) and anti-CD8 (rat IgG2b) mAbs, respectively. The ascites was diluted in sterile phosphate-buffered saline (PBS). Depleting antibodies were injected on day −2, day −1, day 1, and day 5 of treatment at a dose of 500 μg per injection. The depletion conditions were validated by flow cytometry of blood showing more than 95% depletion.
Results
Intratumoral CpG induces regression of the injected tumor but fails to cure the distant tumor
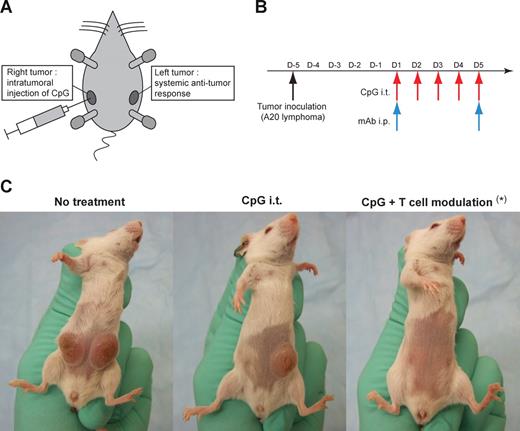
Since we have previously shown that CpG has a direct antiproliferative effect on A20 lymphoma cells,2 we developed a 2-tumor site model to measure the systemic effect of intratumoral CpG vaccination. In this model, mice were challenged with A20 cells at 2 subcutaneous sites (right and left) on the abdomen (Figure 1A). The right tumor was used for intratumoral injections of CpG while the left tumor was used to evaluate the systemic antitumor immune response. When tumors reached 5 mm to 7 mm in diameter, mice received daily injections of intratumoral CpG over 5 days plus 2 intraperitoneal injections of T cell–modulating mAb (anti-OX40, anti-CTLA4, anti-GITR, anti-FR4) on the first and last day of treatment (Figure 1B). Although CpG induced complete regression of the injected (right) tumor, it failed to cure the noninjected (left) tumor (Figures 1C and 2A,B).
Experimental model and treatment administration. (A) The 2-tumor site model. BALB/c mice were inoculated subcutaneously with 5 × 106 A20 tumor cells at 2 different sites: right and left abdomen. Intratumoral injections of CpG were performed in the right tumor while the left tumor served for evaluation of the systemic antitumor immune response. (B) Schema of treatment. Treatment started 5 to 7 days after tumor inoculation when the tumors reached 0.5 cm to 0.7 cm in largest diameter. Mice then received daily injections of intratumoral CpG over 5 days (100 μg per injection, red arrows) and 2 intraperitoneal injections of mAbs used for T-cell modulation (anti-OX40, anti-CTLA4, anti-GITR, anti-FR4) on the first and last day of treatment (blue arrows). (C) CpG effect on the injected (right) and noninjected (left) tumors. In mice bearing 2 tumors, intratumoral injections of CpG induced regression of the injected (right) tumor, but failed to cure the distant (left) tumor, unless combined with effective T-cell modulation (*anti-OX40 + anti-CTLA4 mAbs were used in this example for T-cell modulation). All tumor curves presented in the following figures will show tumor growth at the left (non-CpG injected) site, which reflects the systemic antitumor effect of the immunotherapy.
Experimental model and treatment administration. (A) The 2-tumor site model. BALB/c mice were inoculated subcutaneously with 5 × 106 A20 tumor cells at 2 different sites: right and left abdomen. Intratumoral injections of CpG were performed in the right tumor while the left tumor served for evaluation of the systemic antitumor immune response. (B) Schema of treatment. Treatment started 5 to 7 days after tumor inoculation when the tumors reached 0.5 cm to 0.7 cm in largest diameter. Mice then received daily injections of intratumoral CpG over 5 days (100 μg per injection, red arrows) and 2 intraperitoneal injections of mAbs used for T-cell modulation (anti-OX40, anti-CTLA4, anti-GITR, anti-FR4) on the first and last day of treatment (blue arrows). (C) CpG effect on the injected (right) and noninjected (left) tumors. In mice bearing 2 tumors, intratumoral injections of CpG induced regression of the injected (right) tumor, but failed to cure the distant (left) tumor, unless combined with effective T-cell modulation (*anti-OX40 + anti-CTLA4 mAbs were used in this example for T-cell modulation). All tumor curves presented in the following figures will show tumor growth at the left (non-CpG injected) site, which reflects the systemic antitumor effect of the immunotherapy.
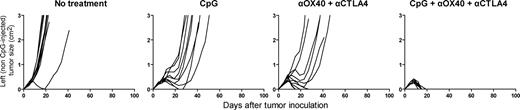
T-cell modulation improves intratumoral CpG vaccination efficacy. (A) Single mAb therapy can improve the therapeutic efficacy of CpG vaccination. Using the 2-tumor model, mice were either left untreated or treated with CpG intratumorally with or without one mAb for T-cell modulation, as described in Figure 1. A panel of 4 different antibodies was tested: anti-OX40 (400 μg/injection), anti-CTLA4 (100 μg/injection), anti-GITR (500 μg/injection), anti-FR4 (100 μg/injection). (B) Some double mAb therapy, but not all, can greatly enhance the therapeutic efficacy of CpG vaccination over single mAb therapy. Anti-OX40, anti-CTLA4, anti-GITR, and anti-FR4 were combined 2 by 2 in conjunction with CpG vaccination and tested for their ability to induce tumor regression. Similar to the previous experiment, mice bearing 2 tumors were either left untreated or treated with CpG intratumorally with or without injection of 2 different antibodies for T-cell modulation. Doses of antibodies were the same as previously described. To rule out a possible dose-effect, one additional group of mice received double dose (2x) of anti-OX40 mAb (800 μg/injection). All growth curves represent the size of the left (non-CpG–injected) tumor. Numbers indicate the ratio of tumor-free mice at day 100 (some groups experienced regression of the left [non-CpG–injected] tumor but eventually grew distant metastasic lymph nodes which are represented in the denominator shown).
T-cell modulation improves intratumoral CpG vaccination efficacy. (A) Single mAb therapy can improve the therapeutic efficacy of CpG vaccination. Using the 2-tumor model, mice were either left untreated or treated with CpG intratumorally with or without one mAb for T-cell modulation, as described in Figure 1. A panel of 4 different antibodies was tested: anti-OX40 (400 μg/injection), anti-CTLA4 (100 μg/injection), anti-GITR (500 μg/injection), anti-FR4 (100 μg/injection). (B) Some double mAb therapy, but not all, can greatly enhance the therapeutic efficacy of CpG vaccination over single mAb therapy. Anti-OX40, anti-CTLA4, anti-GITR, and anti-FR4 were combined 2 by 2 in conjunction with CpG vaccination and tested for their ability to induce tumor regression. Similar to the previous experiment, mice bearing 2 tumors were either left untreated or treated with CpG intratumorally with or without injection of 2 different antibodies for T-cell modulation. Doses of antibodies were the same as previously described. To rule out a possible dose-effect, one additional group of mice received double dose (2x) of anti-OX40 mAb (800 μg/injection). All growth curves represent the size of the left (non-CpG–injected) tumor. Numbers indicate the ratio of tumor-free mice at day 100 (some groups experienced regression of the left [non-CpG–injected] tumor but eventually grew distant metastasic lymph nodes which are represented in the denominator shown).
T-cell modulation enhances intratumoral CpG vaccination efficacy
We next assessed the effect of antibody-mediated T-cell modulation in combination with CpG vaccination in the 2-tumor site model. Four different antibodies (anti-OX40, anti-CTLA4, anti-GITR, anti-FR4) were separately tested in combination with intratumoral CpG. Addition of a single antibody was able to improve CpG vaccination: tumor growth was slowed in the majority of cases and some mice (about 20%-30%) were cured (Figure 2A). In contrast, CpG vaccination alone did not cure any mice.
To further improve these results, we tested the efficacy of pairwise combinations of mAb against T-cell targets together with intratumoral CpG vaccination (Figure 2B). Three combinations (anti-OX40 + anti-CTLA4, anti-OX40 + anti-FR4, anti-CTLA4 + anti-GITR) showed significantly greater efficacy compared with single antibody treatment or to other combinations. Specifically, the combination of anti-OX40 + anti-CTLA4, which gave a consistent and powerful enhancement of CpG vaccination (curing 80% to 100% of the mice), became the focus of our subsequent experiments because all 3 reagents (CpG, anti-OX40, and anti-CTLA4) will soon be available for use in human clinical trials.
Intratumoral CpG is required for anti-OX40 + anti-CTLA4 therapeutic effect
We next tested whether the T-cell–modulating component, anti-OX40 + anti-CTLA4, alone was sufficient to cure lymphoma. Using the 2-tumor site model, mice were treated with CpG alone (without mAb), anti-OX40 + anti-CTLA4 (without CpG), or the full combination (CpG + anti-OX40 + anti-CTLA4). Although the combination of mAb alone (without CpG) was able to delay the tumor growth, only the combination of T-cell modulation with intratumoral CpG was sufficient to completely cure these mice (Figure 3).
CpG is required for therapeutic effect of anti-OX40 + anti-CTLA4 combination. Mice bearing tumors at 2 sites received either no treatment, CpG intratumorally alone at one site, anti-OX40 + anti-CTLA4 intraperitoneally (without CpG), or the combination of both (CpG + anti-OX40 + anti-CTLA4), according to the schedule described previously. Growth curves represent the size of the left (non-CpG–injected) tumor.
CpG is required for therapeutic effect of anti-OX40 + anti-CTLA4 combination. Mice bearing tumors at 2 sites received either no treatment, CpG intratumorally alone at one site, anti-OX40 + anti-CTLA4 intraperitoneally (without CpG), or the combination of both (CpG + anti-OX40 + anti-CTLA4), according to the schedule described previously. Growth curves represent the size of the left (non-CpG–injected) tumor.
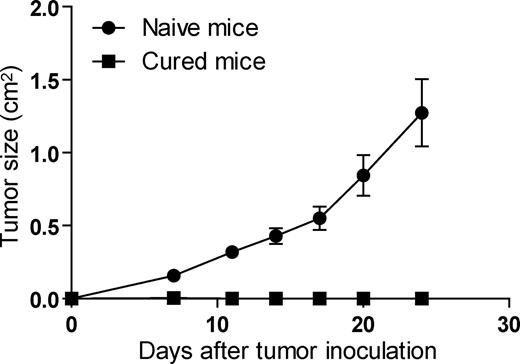
Mice cured with CpG + anti-OX40 + anti-CTLA4 are protected from tumor rechallenge
We next tested whether mice cured with this therapy developed long-term immune protection against the tumor. Mice cured with CpG + anti-OX40 + anti-CTLA4 were rechallenged after 100 days with A20 tumor cells implanted subcutaneously at a different site from the original tumor (dorsally). Naive mice were used as a positive control. Cured mice showed complete protection from tumor rechallenge whereas naive mice grew tumors as expected (Figure 4). This result implies the existence of immunologic memory. Interestingly, vaccination with irradiated A20 cells only provided partial protection following tumor rechallenge as only 2 of 10 mice did not grow tumors (data not shown), suggesting that prior exposition to the tumor may not be the only mechanism by which immunologic memory is being induced in our system.
Mice cured with CpG + anti-OX40 + anti-CTLA4 combination are protected from rechallenge. Naive mice (●) or mice cured from A20 tumors with CpG + anti-OX40 + anti-CTLA4 given 100 days earlier (■) were (re)challenged with 2.5 × 106 A20 tumors cells dorsally. Growth curves represent the average size of the tumor (n = 10 mice per group).
Mice cured with CpG + anti-OX40 + anti-CTLA4 combination are protected from rechallenge. Naive mice (●) or mice cured from A20 tumors with CpG + anti-OX40 + anti-CTLA4 given 100 days earlier (■) were (re)challenged with 2.5 × 106 A20 tumors cells dorsally. Growth curves represent the average size of the tumor (n = 10 mice per group).
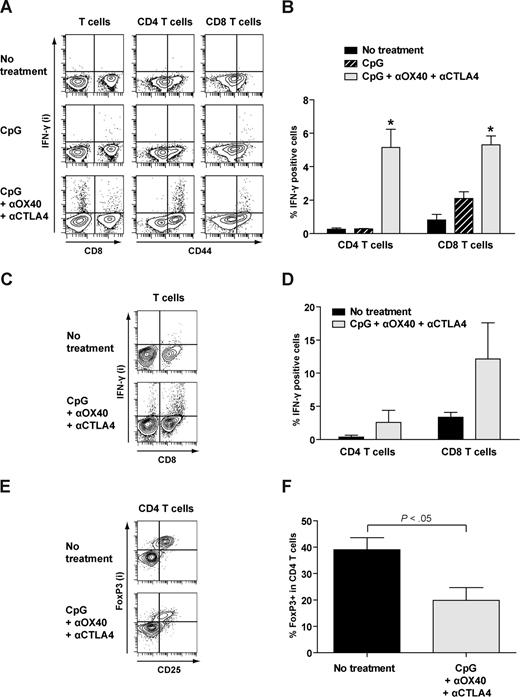
CpG + anti-OX40 + anti-CTLA4 induces antitumor IFN-γ–producing T cells and decreases the percentage of Treg cells
Given the existence of immunologic memory and the effectiveness of T-cell modulation in this therapy, we searched for the induction of antitumor T cells following treatment. Four days after the end of therapy, splenocytes or tumors from mice receiving intratumoral CpG alone or the combination of CpG + anti-OX40 + anti-CTLA4 were incubated overnight in vitro with irradiated A20 tumor cells and then tested for the production of IFN-γ. CD4 and CD8 T cells were analyzed separately for the production of IFN-γ by intracellular flow cytometry. In the spleen, we found a significantly higher percentage of CD4 and CD8 T cells responding to A20 tumor stimulation in mice treated with CpG + anti-OX40 + anti-CTLA4 compared with those that received CpG alone or untreated controls (Figure 5A,B). The full treatment also increased the percentage of IFN-γ–producing T cells in the tumor with a predominance of responding CD8 T cells (Figure 5C,D). These findings are consistent with development of antitumor immune responses in mice that received CpG + anti-OX40 + anti-CTLA4. These IFN-γ–producing T cells were mostly restricted to the CD44high population, a surface marker for memory T cells (Figure 5A). Interestingly, the CD44high T-cell population also significantly increased following treatment compared with the nontreated mice, both in the CD4 (54.6% vs 33.3%, P ≤ .01) and the CD8-positive subsets (35.1% vs 27% respectively, P ≤ .01). The existence of an antitumor memory population was verified functionally as treated mice were protected from tumor rechallenge over 100 days after regression of their primary tumors (Figure 4). We also evaluated the presence of Treg cells in the tumor microenvironment by measuring the percentage of FoxP3-positive CD4 T cells from freshly isolated tumors 4 days after treatment (Figure 5E,F). Interestingly, the proportion of Treg cells appeared to be significantly lower in the treated group compared with the nontreated group (19.8% vs 39% respectively, P < .05).
CpG + anti-OX40 + anti-CTLA4 induces antitumor IFN-γ–producing T cells and decreases the percentage of Treg cells. (A-F) Using the 2-tumor site model, mice bearing A20 tumors were either left untreated, treated with CpG alone, or treated with CpG + anti-OX40 + anti + CTLA4, using the same therapeutic protocol as previously described. Four days after the end of treatment, mice were killed and spleens and tumors were harvested separately and made into a single cell suspension. (A,B) Total splenocytes were cocultured in vitro in the presence of irradiated A20 tumor cells plus anti-CD28 mAb for 24 hours. CD4 and CD8 T cells were assayed for CD44 and intracellular IFN-γ expression. (A) Data from one representative mouse of each group shows IFN-γ expression according to CD44 expression. (B) Average percentage of CD4 and CD8 T cells expressing intracellular IFN-γ of each group (n = 3 mice per group). * indicates a statistically significant difference (P < .05). (C,D) Total cells from the tumor were cocultured in vitro in the presence of irradiated A20 tumor cells plus anti-CD28 mAb for 24 hours. Intracellular expression of IFN-γ for CD4 and CD8 T cells is shown for one representative mouse of each group (C) and as the average of each group (n = 3 mice per group; D). (E,F) Total cells from the tumor were directly analyzed for Treg subpopulation. The proportion of intracellular FoxP3 expressing CD4 T cells is shown for one representative mouse of each group (E) and as the average of each group (n = 3 mice per group; F).
CpG + anti-OX40 + anti-CTLA4 induces antitumor IFN-γ–producing T cells and decreases the percentage of Treg cells. (A-F) Using the 2-tumor site model, mice bearing A20 tumors were either left untreated, treated with CpG alone, or treated with CpG + anti-OX40 + anti + CTLA4, using the same therapeutic protocol as previously described. Four days after the end of treatment, mice were killed and spleens and tumors were harvested separately and made into a single cell suspension. (A,B) Total splenocytes were cocultured in vitro in the presence of irradiated A20 tumor cells plus anti-CD28 mAb for 24 hours. CD4 and CD8 T cells were assayed for CD44 and intracellular IFN-γ expression. (A) Data from one representative mouse of each group shows IFN-γ expression according to CD44 expression. (B) Average percentage of CD4 and CD8 T cells expressing intracellular IFN-γ of each group (n = 3 mice per group). * indicates a statistically significant difference (P < .05). (C,D) Total cells from the tumor were cocultured in vitro in the presence of irradiated A20 tumor cells plus anti-CD28 mAb for 24 hours. Intracellular expression of IFN-γ for CD4 and CD8 T cells is shown for one representative mouse of each group (C) and as the average of each group (n = 3 mice per group; D). (E,F) Total cells from the tumor were directly analyzed for Treg subpopulation. The proportion of intracellular FoxP3 expressing CD4 T cells is shown for one representative mouse of each group (E) and as the average of each group (n = 3 mice per group; F).
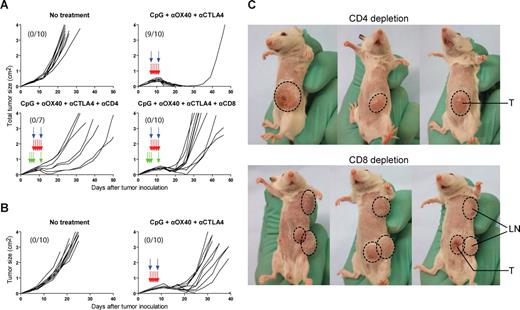
CD4 and CD8 T cells are required for CpG + anti-OX40 + anti-CTLA4 therapeutic effect
To confirm the importance of T cells in our treatment and to study the role of individual T-cell subsets, CD4 or CD8 T cells were depleted from the host using appropriate monoclonal antibodies. The total tumor burden (including the left primary tumor and all the superficial metastatic lymph nodes, with exception of the CpG-injected tumor) was compared among the different groups. Depletion of either CD4 or CD8 T cells completely abolished the therapeutic effect of CpG + anti-OX40 + anti-CTLA4 (Figure 6A). The therapeutic maneuver was also assessed in CD8 KO mice and confirmed the necessity of CD8 T cells (Figure 6B). Interestingly, in CD4 T cell–depleted animals, treatment was effective in controlling tumor dissemination to distant lymph nodes while the primary site grew. In contrast, in CD8 T cell–depleted animals, treatment was more effective in controlling growth in the primary tumor site while disease rapidly spread to lymph nodes (Figure 6C). Finally, late CD4 and CD8 depletions were performed starting the day after the end of therapy to evaluate the requirement for CD4 and CD8 T cells at early versus late phase of the immune response. More than half of the mice were cured in both late CD4- or CD8-depleted groups although more than 80% or 90% depletion of CD4 or CD8 T cells, respectively, was achieved as early as day 7 of therapy (24 hours after start of depletion), suggesting that the antitumor immune T cells acted rapidly after their induction (data not shown).
CD4 and CD8 T cells are required for CpG + anti-OX40 + anti-CTLA4 therapeutic effect. (A) Using the 2-tumor site model, mice received either no treatment or CpG + anti-OX40 + anti-CTLA4, with or without CD4 or CD8 depletion. CpG (red arrows) and anti-OX40 + anti-CTLA4 mAb (blue arrows) were administered as previously. CD4 and CD8 depletion (green arrows) was performed by intraperitoneal injections of ascitic fluid containing 0.5 mg of either anti-CD4 mAb (GK1.5 hybridoma) or anti-CD8 mAb (2.43 hybridoma) on days −2, −1, 1, and 5 from start of treatment. Depletion of CD4 and CD8 T cells was confirmed by flow cytometry on peripheral blood. Growth curves represent the total tumor volume (with exception of the right, CpG-injected tumor) expressed as the sum of the surface of the left tumor and all superficial metastatic lymph nodes when present. Numbers indicate the ratio of tumor-free mice at day 100. (B) Alternatively, BALB/c CD8 KO mice bearing 2 tumors received either no treatment or CpG + anti-OX40 + anti-CTLA4 as previously described. Numbers indicate the ratio of tumor-free mice at day 100. (C) Cancer growth was strikingly different between CD4- and CD8-depleted mice after treatment: tumor cells rapidly disseminated to the lymph nodes (LNs) in CD8-depleted mice whereas they remained confined to the primary tumor site (T) in the CD4-depleted mice. Photographs show 3 representative mice from each group.
CD4 and CD8 T cells are required for CpG + anti-OX40 + anti-CTLA4 therapeutic effect. (A) Using the 2-tumor site model, mice received either no treatment or CpG + anti-OX40 + anti-CTLA4, with or without CD4 or CD8 depletion. CpG (red arrows) and anti-OX40 + anti-CTLA4 mAb (blue arrows) were administered as previously. CD4 and CD8 depletion (green arrows) was performed by intraperitoneal injections of ascitic fluid containing 0.5 mg of either anti-CD4 mAb (GK1.5 hybridoma) or anti-CD8 mAb (2.43 hybridoma) on days −2, −1, 1, and 5 from start of treatment. Depletion of CD4 and CD8 T cells was confirmed by flow cytometry on peripheral blood. Growth curves represent the total tumor volume (with exception of the right, CpG-injected tumor) expressed as the sum of the surface of the left tumor and all superficial metastatic lymph nodes when present. Numbers indicate the ratio of tumor-free mice at day 100. (B) Alternatively, BALB/c CD8 KO mice bearing 2 tumors received either no treatment or CpG + anti-OX40 + anti-CTLA4 as previously described. Numbers indicate the ratio of tumor-free mice at day 100. (C) Cancer growth was strikingly different between CD4- and CD8-depleted mice after treatment: tumor cells rapidly disseminated to the lymph nodes (LNs) in CD8-depleted mice whereas they remained confined to the primary tumor site (T) in the CD4-depleted mice. Photographs show 3 representative mice from each group.
Discussion
In this study, we have shown that T-cell modulation can greatly enhance the efficacy of intratumoral CpG vaccination in lymphoma, thereby eliminating the need for chemotherapy. In our previous system,2 chemotherapy was thought to play an important and useful role by reducing tumor burden, facilitating tumor Ag presentation by inducing apoptosis of tumor cells, or by depleting Treg cells. However, chemotherapy is often marked by toxicity and may induce cellular immune suppression, which could be partly detrimental in inducing an optimally effective vaccine. In the present work, chemotherapy was successfully replaced by T-cell modulation, which allowed cure of large and systemic lymphoma tumors when combined with CpG vaccination.
Some combinations of mAb against T-cell targets (anti-OX40 + anti-CTLA4, anti-OX40 + anti-FR4, and anti-CTLA4 + anti-GITR) appeared to potentiate T-cell modulation whereas other combinations did not show any significant improvement over the respective single antibody treatments. Although the antitumor effect of each of these mAbs used as a single agent has already been described,9,12,17,18 their optimal combination could not have been predicted from prior knowledge about their action. In this study, we used a systematic approach to identify which combinations provided the most powerful antitumor effects.
Among the efficient combinations that we have identified, we decided to focus specifically on CpG + anti-OX40 + anti-CTLA4 because all 3 of these reagents will soon be available for use in human clinical trials. This combination showed a powerful antitumor effect. First, the therapy induced antitumor T cells capable of secreting IFN-γ in response to overnight culture with A20 tumor cells and reduced the proportion of Treg cells at the tumor site. Both CD4 and CD8 T cells were required for the therapy to be effective as shown by CD4 and CD8 depletion studies and CD8 KO mice. Second, greater than 80% of treated mice were cured of large and systemic lymphoma tumors without the need for chemotherapy. Third, the therapy provided long-lasting protection against tumor rechallenge, consistent with the finding that this therapy also produced high numbers of CD44high memory T cells. Finally, we found that CD8 depletion prior to therapy led to rapid dissemination of the tumor to the lymph nodes whereas tumor growth following CD4 depletion was confined to the primary tumor site. This observation is in line with previous findings2 and suggests that CD8 T cells may play an important role in eradicating the tumor cells in the periphery whereas CD4 T cells seem to be required for tumor eradication at the primary site.
The results of the present study have important clinical implications. They support the relevance of new strategies for cancer vaccination that include antibody-mediated T-cell modulation.4,19 Indeed, when dealing with cancer vaccines, it is important to consider 2 equally important phases of the immune response. First is the Ag-priming phase, during which tumor Ags are presented to the immune system by the antigen-presenting cells (primarily DCs) and generate antitumor T cells. Second is the effector phase, during which antitumor T cells migrate to and eradicate the tumor. Importantly, this effector phase may be compromised by tumor-induced immunosuppression.4 In our studies, although intratumoral injection of CpG was efficient in triggering the Ag-priming phase, it was not sufficient to elicit an immune response capable of eradicating advanced and systemic tumors. However, the combination of CpG vaccination with mAb-mediated T-cell modulation was able to amplify the antitumor immune response and thus led to an effective therapy. Combining T-cell modulation with cancer vaccines may therefore be critical to achieve significant clinical efficacy.
A significant concern when using antibodies to enhance the antitumor T-cell response is the potential induction of autoimmunity as T-cell modulation may also activate T cells directed against auto-antigens. This phenomenon has been particularly well described in patients with cancer, mostly melanoma and renal cell carcinoma, treated with anti-CTLA4 antibody. Some of these patients developed autoimmune manifestations including dermatitis, enterocolitis, hypophysitis, and hepatitis.20,21 Additionally, anti-OX40 mAb, which enhances effector T-cell activation and abrogates Treg suppression, may be expected to exacerbate these side effects when combined with anti-CTLA4. In our mouse model, we did not observe any clinical manifestations of autoimmunity. However, this cannot be a guarantee that autoimmunity will not occur in humans because autoimmune manifestations may be subtle and, more importantly, these manifestations may not be equivalent in mice and humans. Indeed, most autoimmune manifestations occurring in patients treated with anti-CTLA4 mAb had not been detected in previous animal studies, including nonhuman primates.22 Finally, these autoimmune manifestations often correlate with antitumor immune response23 and therefore some level of autoimmunity may not be avoidable to achieve clinical efficacy.
Following-up on our previous preclinical results,2 our group recently conducted a phase II clinical trial of a CpG-based vaccine in patients with recurrent follicular lymphoma.24 In this trial, the vaccine consisted of combined low dose local radiotherapy plus intratumoral injections of CpG. As predicted by our mouse model, objective tumor responses have been observed. Given the preclinical results in the present study, we look forward to the testing of anti-OX40 and anti-CTLA4 mAbs in future trials of intratumoral CpG vaccination for lymphoma.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank A. Krieg for providing CpG oligonucleotides, J. Allison for giving the 9H10 hybridoma, and S. Sakaguchi for giving the TH6 and DTA-1 hybridomas. We thank D. Czerwinski for excellent technical help. We thank M. Goldstein, J. Brody, and J. Myklebust for review of this manuscript.
This work was supported by the National Institutes of Health (CA34233 and CA33399) and a Leukemia & Lymphoma Society SCOR grant. R.H. is supported by fellowships from the Fondation de France and the Association pour la Recherche sur le Cancer, and awards from the Institut Lilly and the Fondation Philippe. R.L. is an American Cancer Society Clinical Research Professor.
National Institutes of Health
Authorship
Contribution: R.H. designed and performed experiments, analyzed data, and wrote the paper; and R.L. designed experiments, reviewed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ronald Levy, Professor of Medicine, Chief, Division of Oncology, 269 Campus Dr, CCSR 1105, Stanford University Medical Center, Stanford, CA 94305-5151; e-mail: levy@stanford.edu.

![Figure 2. T-cell modulation improves intratumoral CpG vaccination efficacy. (A) Single mAb therapy can improve the therapeutic efficacy of CpG vaccination. Using the 2-tumor model, mice were either left untreated or treated with CpG intratumorally with or without one mAb for T-cell modulation, as described in Figure 1. A panel of 4 different antibodies was tested: anti-OX40 (400 μg/injection), anti-CTLA4 (100 μg/injection), anti-GITR (500 μg/injection), anti-FR4 (100 μg/injection). (B) Some double mAb therapy, but not all, can greatly enhance the therapeutic efficacy of CpG vaccination over single mAb therapy. Anti-OX40, anti-CTLA4, anti-GITR, and anti-FR4 were combined 2 by 2 in conjunction with CpG vaccination and tested for their ability to induce tumor regression. Similar to the previous experiment, mice bearing 2 tumors were either left untreated or treated with CpG intratumorally with or without injection of 2 different antibodies for T-cell modulation. Doses of antibodies were the same as previously described. To rule out a possible dose-effect, one additional group of mice received double dose (2x) of anti-OX40 mAb (800 μg/injection). All growth curves represent the size of the left (non-CpG–injected) tumor. Numbers indicate the ratio of tumor-free mice at day 100 (some groups experienced regression of the left [non-CpG–injected] tumor but eventually grew distant metastasic lymph nodes which are represented in the denominator shown).](https://ash.silverchair-cdn.com/ash/content_public/journal/blood/113/15/10.1182_blood-2008-07-170274/7/m_zh80020929180002.jpeg?Expires=1767964826&Signature=GHzOhngdEXMlAE1Xo2iuRdGL1DKBHqNRsKn8fp7~q5aXRW~e8KdUf~cpfHvAF32ICQ74d7l7pR5K-ojBqbr7~-JhlIIxwR9z5NU6Iq89MerJ1tZfSVQCox4SPP4zxFxcFoLFbqHa7YrtXcpw2mpK1~oJDXyib4v8JvfktPCHHCf6knAIWuITsI59xDinlTy8ca8NCruqbhUwrAHrXOKlLraD7ONF6w1ogaCEG-gXoCi2MPyD~hrMA1vBQeLLS-1sqkbhst3rdOB3T3CV3KWW7pFekNLEh4B3pYptS9bFACHLd5Xg5XPilCyH46a3wmMdEj6caCco40jYVqaq~jdQMQ__&Key-Pair-Id=APKAIE5G5CRDK6RD3PGA)