Abstract
Interleukin 7 (IL-7) is a common gamma chain receptor cytokine implicated in thymopoiesis and in peripheral expansion and survival of T lymphocytes. The safety and activity of recombinant human IL-7 (rhIL-7) administration were therefore examined in HIV-infected persons. In this prospective randomized placebo-controlled study, a single subcutaneous dose of rhIL-7 was well tolerated with biologic activity demonstrable at 3 μg/kg and a maximum tolerated dose of 30 μg/kg. Injection site reactions and transient elevations of liver function tests were the most notable side effects. Transient increases in plasma HIV-RNA levels were observed in 6 of 11 IL-7–treated patients. Recombinant hIL-7 induced CD4 and CD8 T cells to enter cell cycle; cell-cycle entry was also confirmed in antigen-specific CD8 T cells. Administration of rhIL-7 led to transient down-regulation of the IL-7 receptor alpha chain (CD127) in both CD4+ and CD8+ T cells. Single-dose rhIL-7 increased the numbers of circulating CD4+ and CD8+ T cells, predominantly of central memory phenotype. The frequency of CD4+ T cells with a regulatory T-cell phenotype (CD25high CD127low) did not change after rhIL-7 administration. Thus, rhIL-7 has a biologic and toxicity profile suggesting a potential for therapeutic trials in HIV infection and other settings of lymphopenia. This clinical trial has been registered at http://www.clinicaltrials.gov under NCT0099671.
Introduction
Interleukin 7 (IL-7) is a cytokine produced by epithelial, stromal, and endothelial cells in bone marrow, thymus, and lymph nodes that plays a fundamental role in thymopoiesis as well as in the homeostasis and survival of mature T cells.1-3 Previous studies have shown significant increases in serum or plasma IL-7 levels in lymphopenic states due to HIV infection, chemotherapy, bone marrow transplantation, or idiopathic CD4+ T lymphopenia.4-7
In humans, a significant inverse correlation has been reported between serum IL-7 levels and CD4+ T-cell counts, particularly when counts are below 200 cells/μL in the setting of HIV infection and other lymphopenias.5,7 This phenomenon is thought to represent a compensatory homeostatic response to CD4+ T lymphopenia, and/or cytokine accumulation due to decreased receptor-mediated clearance of IL-7 as a result of lower availability of the IL-7 receptor alpha chain (IL-7Rα, CD127) in these conditions.3,8-11 In animal models of lymphopenia, administration of IL-7 can facilitate restoration of lymphocyte homeostasis even in the presence of high serum levels of IL-7 and low T-cell IL-7 receptor levels.12 Despite its central role in B-cell lymphopoiesis in the mouse, the role of IL-7 in human B-cell lymphopoiesis is not considered essential.3,13 The fundamental roles of IL-7 in thymopoiesis, maturation, survival, and differentiation of T cells provided the rationale for testing this cytokine as an immune adjuvant therapy in HIV infection.
Preclinical studies in SIV-infected macaques have demonstrated a favorable therapeutic index for IL-7 as reflected in proliferation and expansion of both CD4+ and CD8+ T cells without an effect on viremia14,15 and with only minimal demonstrable toxicity. Furthermore, phase 1 studies of rhIL-7 in patients with cancer confirmed the potential for substantial T-cell expansions in the absence of significant toxicity.16
We report here the results of AIDS Clinical Trials group (ACTG) 5214, a phase 1 study designed to evaluate the safety, pharmacokinetic, and biologic properties of a single dose of recombinant human IL-7 (rhIL-7, CYT 0097) in persons with HIV infection.
Methods
Study design
ACTG5214 was a multicenter phase 1, placebo-controlled double-blinded study with a 3:1 randomization (rhIL-7/placebo) for each dose level in each of 2 strata according to plasma HIV RNA levels at screening (stratum 1: < 50 copies/mL, stratum 2: 50-50000 copies/mL). Participants with HIV infection, older than 18 years of age with CD4+ T-cell counts more than 100 cells/μL and HIV-RNA less than 50000 copies/mL receiving highly active antiretroviral therapy (HAART) for a minimum of 12 months without hepatitis B or C or other significant comorbidities were eligible to participate. The protocol was designed to study 3, 10, 30, 60, and 100 μg/kg rhIL-7 as a single subcutaneous dose in a consecutive dose escalation design. A safety monitoring committee evaluated safety data at the completion of each dose group before the next dose group could begin enrollment. Participants were given rhIL-7 or placebo (injection of equal volume of normal saline) on day 0 and then monitored for toxicity on days 1, 4, 14, and 28 with an additional visit on day 56 to test for anti–IL-7 antibodies. Data up to day 28 were used to determine occurrence of dose limiting toxicity (DLT), which was defined as any grade 3 or 4 laboratory or clinical symptom, persistent grade 2 toxicity, protocol-specified increases in viremia (> 0.5 log10 from baseline confirmed by a second measurement), or development of anti–IL-7 antibodies. The Division of AIDS (DAIDS) toxicity table version 1992 was used17 (at the start of the trial the December 2004 version18 was not yet available). Dose escalation progressed independently in the 2 strata. The study was approved by the institutional review boards (IRBs) of all participating sites and written informed consent was obtained from all participants in accordance with the Declaration of Helsinki (NCT 00099671).
rhIL-7
rhIL-7 is a nonglycosylated protein, composed of 153 amino acids (with an additional Escherichia coli–derived methionine at the N-terminus and with a relative nonglycosylated molecular mass of ∼ 18 kDa). The unglycosylated protein is fully active and has 3 disulfide bridges: Cys3-Cys93, Cys35-Cys130, and Cys48-Cys142. The molecular formula is C767H1250N214O229S12.
Flow cytometric studies
CD4+ and CD8+ T-cell absolute counts, expression of the IL-7 receptor α chain CD127, and expression of CD31 (a marker identifying naive T cells enriched in primary thymic emigrants19 ) and intracellular Ki67 by T cells, the proportions of naive and memory subsets defined by expression of CD45RA and CD62L (naive: CD45RA+CD62L+, primary thymic emigrant CD4+ T cells: naive CD31+, central memory: CD45RA−CD62L+, effector memory: CD45RA−CD62L−, and CD45RA+ effectors: CD45RA+CD62L−), and proportions of activated T cells as indicated by expression of HLA-DR and CD38 were measured in whole blood within 6 hours of blood draw by flow cytometry assays using ACTG consensus methods (https://www.actgnetwork.org) at baseline and days 1, 4, 14, and 28. The following monoclonal antibodies were used for flow cytometry: CD3 FITC or APC (clone SK7), CD4 PerCP and APC (clone SK3), CD8 FITC, PE, PerCP, and APC (clone SK1), CD31 PE (clone L133.1), CD38 PE (clone HIT2), CD45RA FITC (clone HI100), CD62L APC (clone Dreg 56), HLA-DR FITC (clone L243), and Ki67 PE (clone B56) all from BD Biosciences; and CD127 PE (clone 11711) from R&D Systems. Whole blood was stained according to the manufacturer's recommended protocol. CellQuest (BD Biosciences) was used for data acquisition and CellQuest or FlowJo (TreeStar) was used for data analyses.
Cryopreserved peripheral blood mononuclear cells (PBMCs) collected at baseline, day 4, and day 28 were used to define B-cell phenotypes, measure the expression of Ki67 among phenotypically defined CD4+ and CD8+ T-cell maturation subsets, as well as to enumerate and characterize the phenotype of preexisting memory T-cell responses using MHC class I tetramers. Cryopreserved cells were thawed according to standard protocols and stained with a panel of fluorochrome-labeled monoclonal antibodies specific for surface and intracellular antigens including: CD19-PE-Cy7 (clone SJ25C1), CD10-APC (clone HI10a), CD27-APC (L128l), CD3-Alexa 700 (clone SP34-2), CD4-PerCP-Cy5.5 (clone L200), CD25-APC-Cy7 (clone MA251), and Ki67-FITC (clone B56), all from BD Biosciences; CD27-PC5 (clone 1A4CD27), CD21-FITC (clone BL13), and CD45RO-ECD (clone UCHL1) from Beckman Coulter; CD127-PE-Cy7 and CD127-APC Alexa 750 (clone eBioRDR5) from eBioscience; CD8-Pacific Orange (clone 3B5) from Invitrogen; as well as an amine reactive dye for live-dead discrimination (LIVE/DEAD Fixable Violet Dead Cell Stain; also from Invitrogen). Stained samples were acquired on an LSR-II or a FACSAria flow cytometer operated by BD FACSDiVa software both from BD Biosciences and analyzed using the FlowJo software package version 8.
MHC class I tetramers
MHC class I tetramers were prepared as previously described.20 Briefly, HLA-A2, -A3, and -B7 monomers were synthesized and biotinylated in the National Institutes of Health (NIH, Bethesda, MD) tetramer core facility with peptides corresponding to HLA-A2, -A3, and -B7 restricted CD8+ T-cell epitopes previously characterized as specific for cytomegalovirus, Epstein-Barr virus, influenza virus, and HIV (Table S1, available on the Blood website; see the Supplemental Materials link at the top of the online article) folded in the peptide-binding groove. These monomers were subsequently tetramerized using streptavidin-APC (BD Pharmingen). The A2/ebv.GLC and B7/cmv.TPR tetramers were purchased from Beckman Coulter.
Plasma HIV-RNA measurements
HIV-1 RNA levels in plasma were measured using the Roche Amplicor HIV-1 Monitor UltraSensitive assay, by Clinical Laboratory Improvement Amendments–certified or equivalent laboratories.
Pharmacokinetic analysis
Plasma IL-7 levels were measured at baseline, and 0.5, 1, 1.5, 2, 2.5, 4, 8, 12, 24, 48, and 72 hours after subcutaneous injection of rhIL-7 or placebo. IL-7 was assayed by enzyme-linked immunosorbent assay (ELISA: Diaclone SAS) with a lower limit of detection established at 2.47 pg/mL. Pharmacokinetic indices were calculated by the Kinetica 4.2 software (Thermo Fisher Scientific) using the extravascular route and the noncompartmental model.
Statistical methods
Tests reported are 2-sided and exploratory without adjustment for multiple testing; we report P values less than .01 as statistically significant. The 2 strata (HIV RNA levels < 50 copies/mL and HIV RNA levels 50-50000 copies/mL) were combined and results among actively treated (rhIL-7) and placebo-treated subjects were compared after multiple linear regression models showed that the stratum assignment had no significant effect on biologic activity (T-cell count or T-cell expression of Ki67). The rhIL-7 effect on each end point was tested and estimated by comparing the subjects on the active rhIL-7 arm of a particular dose versus the combined placebo subjects. Median values of all tested variables are reported throughout and median values with bars representing interquartile ranges (IQR) are shown in the figures. Comparisons of continuous end points between 2 groups were analyzed with a Wilcoxon rank sum test, and within a single group the Wilcoxon signed rank test was used to test for a nonzero median.
Results
Study participants
Twenty-five subjects were enrolled between June 2005 and February 2007. Seventeen subjects were enrolled in stratum 1 (4 in the 3-μg/kg, 4 in the 10-μg/kg, 5 in the 30-μg/kg, and 4 in the 60-μg/kg dose group) and 8 subjects in stratum 2 (4 in the 3-μg/kg and 4 in the 10-μg/kg dose group). One of these 25 subjects was enrolled in the 30-μg/kg dose group to replace a subject with missing flow cytometric data who was excluded from all analyses except safety. The demographic and baseline characteristics of study participants are shown in Table 1. The randomization and stratum distribution of all participants is shown in Table S2.
Toxicity data
Two dose-limiting toxicities (DLTs) occurred in 2 different subjects in stratum 1 at the 60-μg/kg dose, defining 30 μg/kg as the maximum tolerated dose (MTD) according to the study design. One DLT was a grade 3 skin induration at the site of 2 rhIL-7injections (the dose was split to fit within the 1-mL maximum allowable injection volume). Of note, this skin reaction would be scored as a grade 2 toxicity using the most recent (December 2004) Division of AIDS toxicity table.18 The second DLT was a transient grade 3 elevation of alanine aminotransferase and aspartate aminotransferase. There were no grade 4 toxicities and apart from these DLTs, the most noted toxicities were grade 1 and 2 localized skin injection site reactions and mild generalized symptoms (headache, body aches, fatigue) as outlined in Table S3. There were no changes in QTc intervals on electrocardiographic examination (data not shown). No subject developed neutralizing antibodies to IL-7 in samples obtained on days 28 and 56.
Plasma levels of HIV-RNA
Transient “blips” in plasma HIV viremia were observed during the days of observed peak T-cell proliferation or increased T-cell counts (days 4 or 14) in 6 of 11 rhIL-7 recipients (Table 2) with HIV-RNA less than 50 copies/mL at day 0; however, plasma HIV-RNA levels returned to less than 50 copies/mL in all subjects by day 28 or by the end of study (day 56) with the exception of one subject with an HIV-RNA level of 61 copies/mL (< 50 copies/mL on day 70) and a second subject with an HIV-RNA level of 96 copies/mL on day 28. After the end of study participation this subject had consecutive HIV-RNA levels of less than 50 copies/mL at clinical follow-up. No statistically significant differences in plasma HIV-RNA from day 0 to day 28 were found in the rhIL-7–treated subjects in stratum 2 (median of 1717 HIV-RNA copies/mL at day 0 and 244 copies/mL on day 28, P = .19).
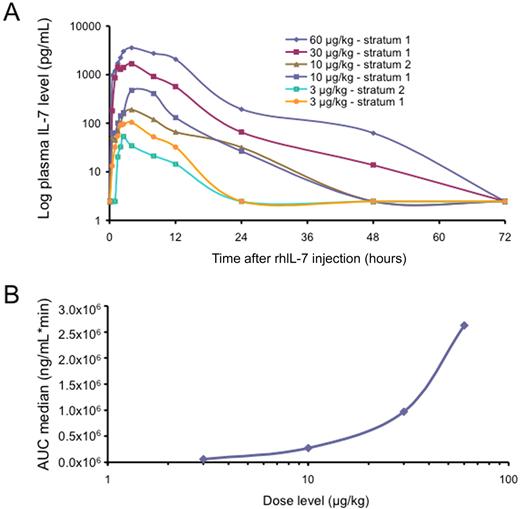
Pharmacokinetic data
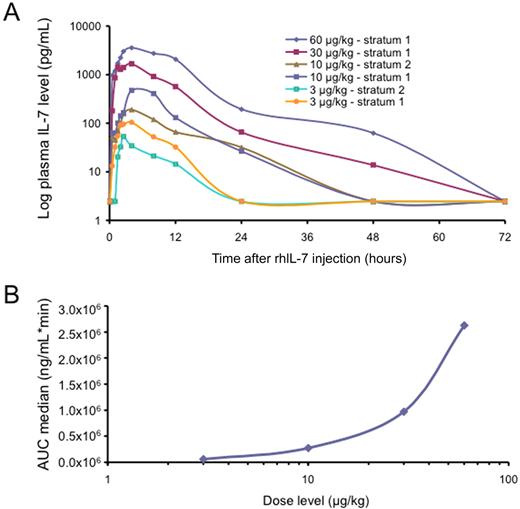
The log10 of median blood levels of rhIL-7 were plotted by dose levels against time (Figure 1A) showing large dose-dependent increases in both peak levels and areas under the curve (AUCs). Both AUC (Figure 1B) and peak levels (Table 3) clearly demonstrate a nonlinear pharmacokinetic profile with blood levels increasing much more than expected at the highest doses. A calculation of the apparent distribution volume of IL-7 produced extremely high figures in the range of 15000 L at 3 μg/kg decreasing to 1000 L at 60 μg/kg. This typically reflects drug distribution to a high-affinity compartment with a progressive saturation of this mechanism at higher doses, suggesting that CD127+ T cells may be responsible for this high affinity and saturable uptake from the plasma.
Pharmacokinetic data. (A) Plasma IL-7 levels by stratum and dose after rhIL-7 administration are shown. (B) The median AUC is plotted, demonstrating a nonlinear pharmacokinetic profile with small increases of the dose leading to large increases in AUC.
Pharmacokinetic data. (A) Plasma IL-7 levels by stratum and dose after rhIL-7 administration are shown. (B) The median AUC is plotted, demonstrating a nonlinear pharmacokinetic profile with small increases of the dose leading to large increases in AUC.
Endogenous serum IL-7 levels
Serum IL-7 levels were measured on day 28 to assess the potential impact of exogenous administration of supraphysiologic levels of cytokine on endogenous IL-7 expression. There was no effect of treatment on serum levels of IL-7 as measured on day 28 (median change, −0.90 pg/mL in the rhIL-7 arm versus +0.09 pg/mL in the placebo arm, P = .733).
Changes in lymphocyte counts
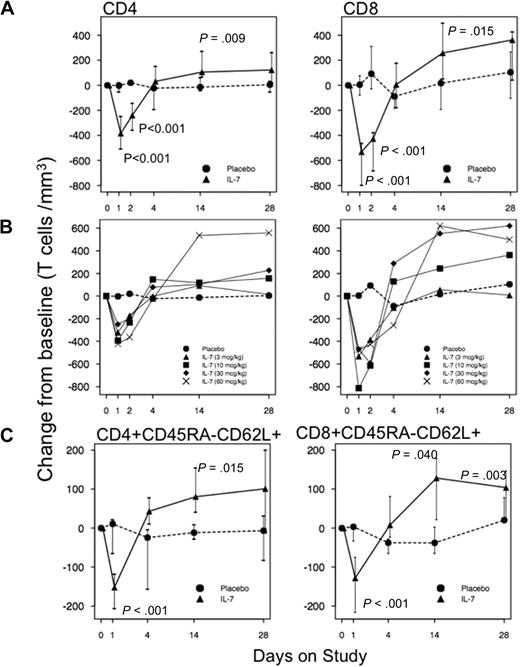
A significant decrease in circulating CD4+ and CD8+ T-cell counts was noted combining all rhIL-7–treated subjects on days 1 and 2 following dosing (P < .001). On day 1, CD4+ T-cell counts fell by a median of 384 cells/μL from baseline compared with only a drop of 2 cells/μL in placebo recipients (P < .001, Figure 2A). Over the same interval, CD8+ T cells fell by a median of 532 cells/μL in actively treated subjects and increased by 5 cells/μL in placebo recipients (P < .001, Figure 2A). This transient T-cell lymphopenia, which has also been described in IL-2–treated patients and in IL-7–treated macaques, possibly represents redistribution of cells out of the circulation and reversed quickly.21,22 Statistically significant increases in median circulating CD4+ T-cell counts were observed in the rhIL-7 recipients compared with those in placebo recipients on day 14 (+106 vs −14 cells/μL, P = .009, Figure 2A). Similar increases were seen in the CD8+ T-cell counts in the rhIL-7–treated subjects on day 14 (+258 cells/μL versus +17 cells/μL in the placebo group, P = .015, Figure 2A). Similar results were obtained when the subjects treated with rhIL-7 at 60 μg/kg were excluded from the analysis (Figure S1A). The T-cell increases were seen predominantly at the 10-, 30-, and 60-μg/kg doses with some evidence of dose response, although the numbers were too small for statistical comparisons (Figure 2B). The T-cell increases on day 14 were due predominantly to increases in central memory CD4+ (+81 versus −12 cells/μL, P = .003) and CD8+ T cells (+128 versus −38 cells/μL, P = .003) as shown in Figure 2C (and Figure S1B with the 60-μg/kg subjects excluded) and to a lesser extent to increases in naive CD4+ (+19 in rhIL-7 versus −5 cells/μL, P = .378) and CD8+ T cells (+66 versus −5 cells/μL in placebo recipients, P = .047) as shown in Figure S2A. No statistically significant changes were observed in the percentages or numbers of naive CD4+ cells expressing CD31 (data not shown). Moderate increases of effector CD4+ but not CD8+ T cells were observed on days 14 and 28 (Figure S2B), whereas no significant changes were seen in CD45RA+ effector memory CD8+ T cells (Figure S2C).
Changes in T-cell counts after rhIL-7 administration. (A) CD4+ and CD8+ T-cell counts decreased significantly on days 1 and 2 and increased significantly on day 14 after the rhIL-7 dose. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ). (B) CD4+ and CD8+ T-cell changes from baseline according to rhIL-7 dose group. ● represents placebo participants (
). (B) CD4+ and CD8+ T-cell changes from baseline according to rhIL-7 dose group. ● represents placebo participants ( ) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). (C) Central memory CD4+ and CD8+ T cells decreased significantly on day 1 and increased significantly on day 14 and day 28 (CD8+ T cells) after a single rhIL-7 administration. ● represents placebo participants (
) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). (C) Central memory CD4+ and CD8+ T cells decreased significantly on day 1 and increased significantly on day 14 and day 28 (CD8+ T cells) after a single rhIL-7 administration. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ).
).
Changes in T-cell counts after rhIL-7 administration. (A) CD4+ and CD8+ T-cell counts decreased significantly on days 1 and 2 and increased significantly on day 14 after the rhIL-7 dose. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ). (B) CD4+ and CD8+ T-cell changes from baseline according to rhIL-7 dose group. ● represents placebo participants (
). (B) CD4+ and CD8+ T-cell changes from baseline according to rhIL-7 dose group. ● represents placebo participants ( ) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). (C) Central memory CD4+ and CD8+ T cells decreased significantly on day 1 and increased significantly on day 14 and day 28 (CD8+ T cells) after a single rhIL-7 administration. ● represents placebo participants (
) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). (C) Central memory CD4+ and CD8+ T cells decreased significantly on day 1 and increased significantly on day 14 and day 28 (CD8+ T cells) after a single rhIL-7 administration. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ).
).
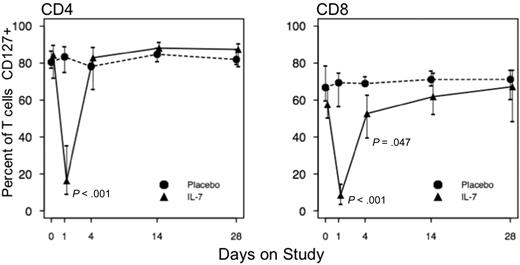
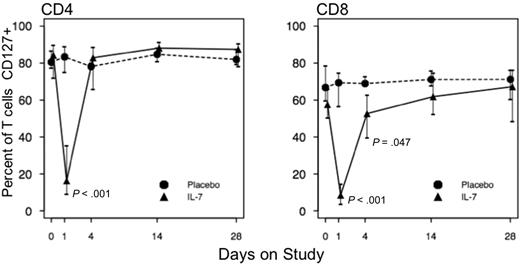
The proportion of CD4+ T cells expressing CD127 (the IL-7 receptor α chain) decreased significantly but transiently on day 1 from 84.29% at baseline to 16.33% (a median drop of 55.87 percentage points versus an increase of 2.2 percentage points among placebo recipients, P < .001, Figure 3 and Figure S3A with the subjects receiving 60 μg/kg rhIL-7 excluded). CD127 expression returned to baseline in rhIL-7 recipients by day 4 (Figure 3). Similarly, the proportion of CD8+ T cells expressing CD127 decreased on day 1 by a median of 47.7% in rhIL-7–treated subjects and increased by 0.20% in placebo recipients (P < .001, Figure 3 and Figure S3A). CD127 expression on CD8+ T cells returned to baseline by day 14.
Changes in CD127 expression on T cells after rhIL-7 administration. CD127-expressing CD4+ and CD8+ T cells decreased after rhIL-7 administration and re-emerged by day 4 among CD4+ T cells or day 14 among CD8+ T cells. P values represent comparisons between rhIL-7 and placebo recipients by Wilcoxon rank sum test. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ).
).
Changes in CD127 expression on T cells after rhIL-7 administration. CD127-expressing CD4+ and CD8+ T cells decreased after rhIL-7 administration and re-emerged by day 4 among CD4+ T cells or day 14 among CD8+ T cells. P values represent comparisons between rhIL-7 and placebo recipients by Wilcoxon rank sum test. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ).
).
T-cell cycling and activation
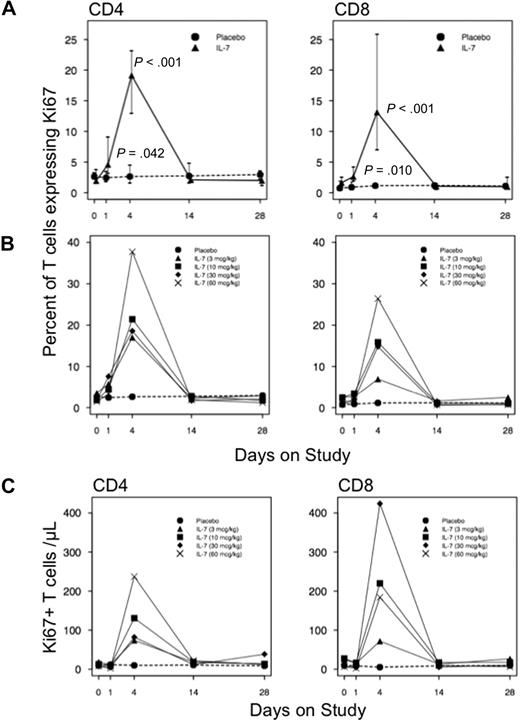
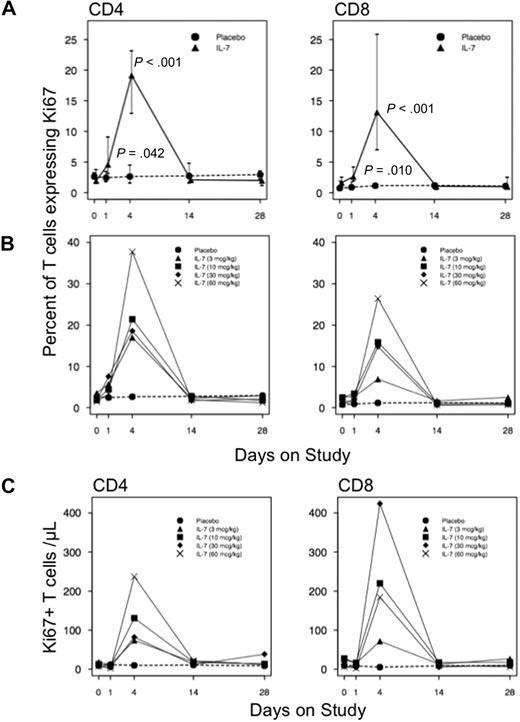
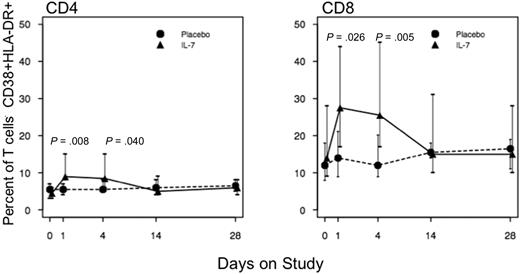
Recombinant hIL-7–treated subjects manifested increases in the frequencies of T cells in cell cycle as measured by increases in the proportions of cells expressing intracellular Ki67. The proportion of CD4+ T cells expressing Ki67 increased from 1.95% at baseline to 4.60% on day 1 (P = .042 compared with placebo) and peaked at 19.15% (P < .001) on day 4 (Figure 4A). Expression of Ki67 in CD8+ T cells increased from 1.65% at baseline to 2.63% on day 1 (P = .010 compared with placebo) and further increased to 13.15% (P < .001) at day 4 (Figure 4A). This effect appeared to be dose dependent in both CD4+ and CD8+ T cells (Figure 4B) and was also observed when the numbers of T cells expressing Ki67 were compared (Figure 4C). Statistically significant increases of T cells expressing Ki67 were also observed when the subjects who received 60 μg/kg were excluded from the analysis (Figure S4A-B). Transient increases in other phenotypic markers of T-cell activation (coexpression of CD38 and HLA-DR) accompanied T-cell proliferation on days 1 and 4 (Figure 5 and Figure S3B) with the peak preceding the peak Ki67 expression. As shown in Figure 5, the proportion of activated (CD38+HLA-DR+) CD4+ T cells increased from 4.5% (vs 5.5% in placebo recipients, P = .882) at baseline to 9% on day 1 (P = .008 compared with placebo) and 8.5% on day 4 (P = .040 compared with placebo). The proportion of activated CD8+ T cells in rhIL-7 recipients increased from 14% versus 12% in placebo recipients at baseline (P = .444) to 27.50% on day 1 and 25.50% on day 4 (P = .026 and P = .005, respectively, compared with placebo recipients). There were no statistically significant changes in the intracellular levels of the antiapoptotic protein Bcl-2 (as measured by mean fluorescence intensity) in either CD4+ or CD8+ T cells (data not shown).
Cycling of CD4+ and CD8+ T cells in response to rhIL-7. (A) Increased CD4+ and CD8+ T-cell cycling was seen on days 1 and 4, returning to baseline by day 14. (B) The degree of T-cell proliferation was higher at higher dosing levels. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ). (C) Absolute counts of Ki67+ T cells during study participation by rhIL-7 dose. ● represents placebo participants (
). (C) Absolute counts of Ki67+ T cells during study participation by rhIL-7 dose. ● represents placebo participants ( ) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). P values represent comparisons between rhIL-7 and placebo recipients by Wilcoxon rank sum test.
) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). P values represent comparisons between rhIL-7 and placebo recipients by Wilcoxon rank sum test.
Cycling of CD4+ and CD8+ T cells in response to rhIL-7. (A) Increased CD4+ and CD8+ T-cell cycling was seen on days 1 and 4, returning to baseline by day 14. (B) The degree of T-cell proliferation was higher at higher dosing levels. ● represents placebo participants ( ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ). (C) Absolute counts of Ki67+ T cells during study participation by rhIL-7 dose. ● represents placebo participants (
). (C) Absolute counts of Ki67+ T cells during study participation by rhIL-7 dose. ● represents placebo participants ( ) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). P values represent comparisons between rhIL-7 and placebo recipients by Wilcoxon rank sum test.
) and rhIL-7 participants are represented by ▲ (3 μg/kg), ■ (10 μg/kg), ♦ (30 μg/kg), and X (60 μg/kg). P values represent comparisons between rhIL-7 and placebo recipients by Wilcoxon rank sum test.
Emergence of activated CD4+ and CD8+ T cells after rhIL-7 administration. Activated CD4+ and CD8+ T cells (HLA-DR+CD38+) increased on days 1 and 4 after rhIL-7 administration but remained unchanged in placebo recipients. ● represents placebo participants ( ) and ▲ represets rhIL-7 participants (
) and ▲ represets rhIL-7 participants ( ).
).
Emergence of activated CD4+ and CD8+ T cells after rhIL-7 administration. Activated CD4+ and CD8+ T cells (HLA-DR+CD38+) increased on days 1 and 4 after rhIL-7 administration but remained unchanged in placebo recipients. ● represents placebo participants ( ) and ▲ represets rhIL-7 participants (
) and ▲ represets rhIL-7 participants ( ).
).
Further analysis of Ki67 expression within memory and naive as well as in CD127+ and CD127− T-cell subsets was performed to ascertain whether distinct cell populations were differentially induced to enter cell cycle in response to IL-7. We found that naive cells and all defined memory and effector subsets of CD4+ and CD8+ T cells were induced to enter cell cycle after IL-7 exposure (Table 4). Although cycling within naive CD8+ (+10.58%, P < .001) and CD4+ T cells (+2.98%, P < .001) significantly increased from baseline, the increase that was seen in naive CD8+ T cells was much higher than that observed in CD4+ T cells (P < .001). As anticipated, CD4+ T-cell cycling increased significantly only in the CD127+ (IL-7Rα) subset but significant increases in CD8+ T-cell cycling were seen in subsets with detectable IL-7Rα expression and also in those in which this receptor could not be detected. It should be noted that the increase in Ki67 expression among the CD8+CD127− T cells was modest (median change from baseline, +3.18%) and substantially lower (P < .001) than the increase seen in CD8+CD127+ T cells (median change from baseline, +13.46%).
CD4+ T cells with regulatory phenotype
Regulatory CD4+ T cells (Tregs) were defined as CD4+CD25high CD127low.23,24 The proportion of Tregs was studied at baseline, day 4, and day 28. There was no evidence of significant increases in cycling of Tregs (Ki67+) in rhIL-7 recipients on day 4 (+0.57% in rhIL-7 versus +1.30% in placebo recipients, P = .300, Table 4). Changes from baseline in the proportion of CD4+ T cells with Treg phenotype did not differ between rhIL-7 and placebo recipients on day 28 (−0.92% versus −1.40%, P = .481, Figure S5).
Responses of antigen-specific CD8+ T cells to IL-7 administration
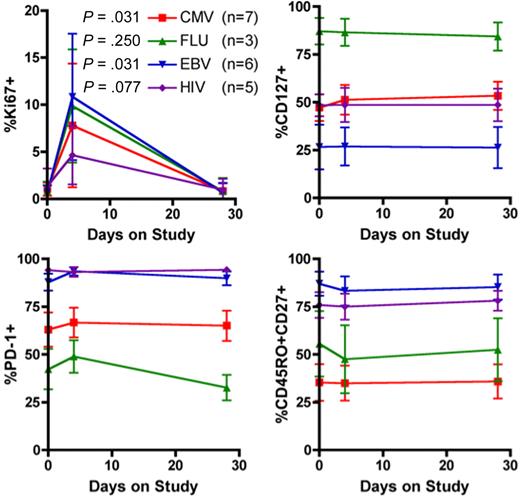
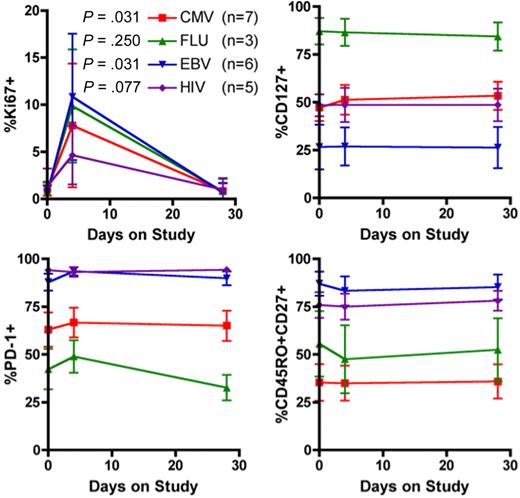
To determine the effect of rhIL-7 administration on the pool of antigen-specific CD8+ T cells, we used MHC class I tetramer staining in conjunction with monoclonal antibody staining for markers of CD8+ T-cell differentiation, activation, and proliferation. The tetramers used are described in Table S1. Our study population contained 11 HLA-A2+ subjects (of whom one was also HLA-A3+ and another was also HLA-A3+ and HLA-B7+), 5 HLA-A3+ subjects, and 4 HLA-B7+ subjects. We therefore focused on epitopes from common pathogens presented by HLA-A2, -A3, and -B7 and found 9 subjects with cytomegalovirus (CMV)–reactive cells (2 placebo recipients, 2 at 3 μg/kg, 2 at 10 μg/kg, and 3 at 30 μg/kg rhIL-7), 7 with Epstein-Barr virus (EBV)–reactive cells (1 placebo, 1 at 3 μg/kg, 3 at 10 μg/kg, and 2 at 30 μg/kg rhIL-7), 3 with influenza virus (FLU)–reactive cells (all treated with rhIL-7, 1 at 3 μg/kg and 2 at 10 μg/kg), and 6 with HIV-specific cells (1 placebo, 3 at 3 μg/kg, and 2 at 10 μg/kg rhIL-7), one of whom had 2 distinct populations binding the A3/hiv.QVP and A3/hiv.RLR tetramers. In total, we measured 26 antigen-specific populations (4 among placebo recipients) in 13 participants.
We found that rhIL-7 administration did not result in an increase in the fraction or absolute number of peptide/tetramer-binding CD8+ T cells (Figure S6), with no significant differences in the impact of IL-7 among CD8+ T cells of various antigenic specificities. The fraction of these cells in cycle, as reflected by Ki67 expression, was increased on day 4 and returned to baseline levels by day 28 (Figure 6). We next sought to determine whether IL-7 administration altered the fraction of antigen-specific CD8+ T cells expressing markers of memory T-cell differentiation or expression of CD127 or PD-1. This analysis did not reveal any significant rhIL-7 effect on the expression of CD45RO, CD27, CD127, or PD-1 on tetramer-positive CD8+ T cells (Figure 6).
Characterization of Ag-specific CD8+ T cells during study participation. Phenotypic analysis of Ag-specific CD8+ T cells at baseline, day 4, and day 28. Significant increases in Ki67 expression were observed on day 4, returning to baseline on day 28. PD-1, CD127, and CD45RO/CD27 expression did not change significantly after rhIL-7 administration.
Characterization of Ag-specific CD8+ T cells during study participation. Phenotypic analysis of Ag-specific CD8+ T cells at baseline, day 4, and day 28. Significant increases in Ki67 expression were observed on day 4, returning to baseline on day 28. PD-1, CD127, and CD45RO/CD27 expression did not change significantly after rhIL-7 administration.
In all, these results indicate that single-dose rhIL-7 administration increased the nonselective recruitment of antigen-specific memory CD8+ T cells into cell cycle without inducing a major shift in the balance among phenotypically defined memory subsets.
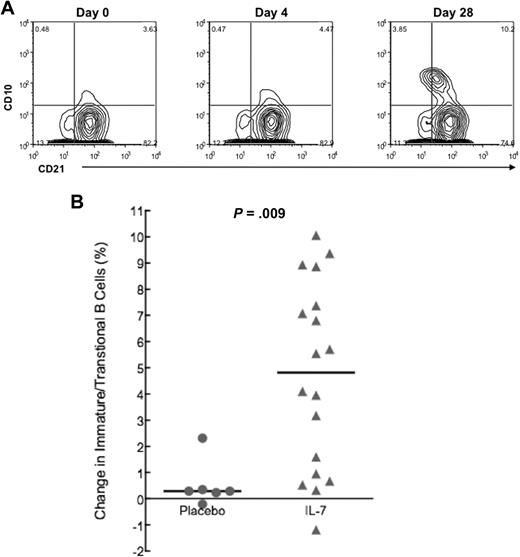
B lymphocytes
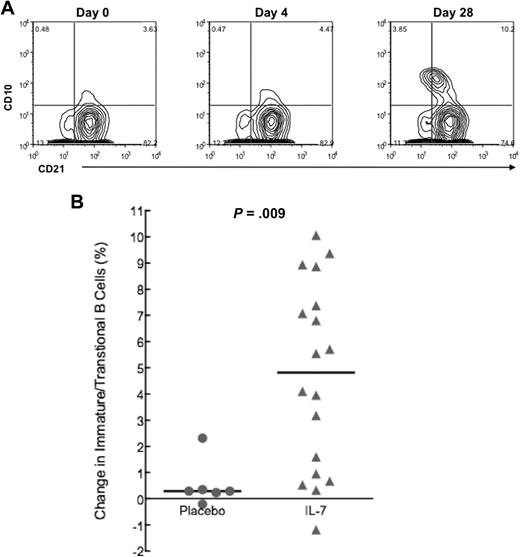
In HIV infection and in idiopathic CD4+ T lymphopenia, an increased proportion of immature/transitional B cells expressing CD10 has been described. The proportion of these cells, which can further be divided into T1 (CD21low) and T2 (CD21high) transitional stages, correlates with serum levels of IL-7.6,25 To assess the potential impact on B lymphocytes of in vivo administration of supraphysiologic levels of rhIL-7, the proportion of immature/transitional B cells (CD19+CD27−/CD10+ and CD21low/high, Figure 7A) was measured at baseline, day 4, and day 28 in IL-7– and placebo-treated participants. The increase in the proportion of immature/transitional B cells in the rhIL-7 group (median, 5.7% at day 0 vs 12.7% at day 28; median change from baseline, 4.82%) was significantly greater (P = .009) than the corresponding change in placebo subjects (median, 5.1% at day 0 vs 5.4% at day 28; median change from baseline, 0.29%) as shown in Figure 7B and was not correlated with the dose of rhIL-7. Total circulating B-cell counts were unaffected by rhIL-7 administration (data not shown).
Emergence of immature/transitional B cells after rhIL-7 administration. (A) Example of contour plot demonstrating the emergence of CD27−CD10+CD21low/high (immature/transitional) B cells at day 28. (B) Summary data from placebo and rhIL-7 recipients confirmed a statistically significant increase of the subset of immature/transitional B cells on day 28. PBMCs were gated on CD19+ cells and mature CD27+CD10+ B cells were excluded.
Emergence of immature/transitional B cells after rhIL-7 administration. (A) Example of contour plot demonstrating the emergence of CD27−CD10+CD21low/high (immature/transitional) B cells at day 28. (B) Summary data from placebo and rhIL-7 recipients confirmed a statistically significant increase of the subset of immature/transitional B cells on day 28. PBMCs were gated on CD19+ cells and mature CD27+CD10+ B cells were excluded.
Discussion
In this phase 1 dose escalation study, administration of rhIL-7 to HIV-infected participants was well tolerated with significant biologic activity observed even at the lowest doses, suggesting a favorable profile for further development in the setting of HIV infection.
Cytokine therapies have been studied in HIV infection with the purpose of enhancing T-cell reconstitution or function and/or improving antiviral responses.26 The cytokine in the most advanced stages of development as an immune-based therapy is IL-2, which was evaluated in phase 3 studies for treatment of HIV infection27 and was found to confer no clinical benefit despite significant expansions of CD4+ T cells.28,29 Cyclic administration of IL-2 to HIV+ patients led to substantial CD4+ T-cell expansions and was associated with significant toxicities.30 Of note, after IL-2 administration, the majority of expanded CD4+ T cells expressed the IL-2 receptor α chain (CD25), had a central memory or naive phenotype, expressed FoxP3, and exerted moderate suppressive activity in vitro.31,32 It should be noted that CD4+ T-cell expansion after IL-7 administration to cancer patients was not associated with either increased CD25 or FoxP3 expression,16 or with relative expansion of phenotypically defined Tregs as shown in the present study. In addition, naive T cells expanded by IL-7 express CD31 and have broad specificities as suggested by their broad T-cell receptor repertoire.33
We demonstrate here that IL-7 appears to have a very potent effect in vivo as we found that even the lowest dose of 3 μg/kg was associated with evidence of biologic activity after only a single subcutaneous injection. Overall, injections were well tolerated with mainly local reactions and transient liver function test elevations as the only clinically significant toxicity. More importantly, there were no sustained or significant elevations in plasma viremia either in viremic subjects or in subjects with baseline levels of plasma virus below the limits of detection. Small transient increases in plasma viremia were observed in some participants similar to those seen after IL-2 administration in the pre-HAART era.34 It is not clear whether these “blips” represent reactivation of virus from latently infected reservoirs35,36 or reflect increased viral production from activated T cells since we did see evidence of transient T-cell activation and cell-cycle entry. The source and significance of these blips remain to be determined and should be monitored carefully during administration of IL-7.
A single dose of IL-7 did lead to substantial CD4+ and CD8+ T-cell recruitment into cell cycle without demonstrable up-regulation of the antiapoptotic molecule Bcl-2. Increases in Ki67 expression were observed among naive, central memory, effector memory, and CD45RA+ effectors of both CD4+ and CD8+ T-cell lineage. In contrast, there was no evidence for induction of cycling in CD4+ T cells with Treg phenotype, consistent with their low expression of CD127. Of note, IL-7–induced recruitment of T cells into cell cycle was also observed for a wide array of antigen-specific memory CD8+ T cells that recognized HIV, CMV, EBV, and influenza class I–restricted epitopes.
The fraction of circulating T cells with an activated surface phenotype (coexpression of HLA-DR and CD38) increased after IL-7 administration and peaked at day 1, before the peak in Ki67 expression, which occurred on day 4 after injection. Interestingly, when CD4+ and CD8+ T cells were examined according to CD127 expression, recruitment into cell cycle was seen predominantly among CD4+ T cells that expressed CD127, whereas among CD8+ T cells, small increases in Ki67 were also seen in CD127− T cells, albeit at a significantly lower degree than that seen among CD127+ CD8+ T cells. This suggests that the down-regulation of CD127 seen immediately after rhIL-7 injection is self-limited with responding cells capable of expansion and re-expression of CD127, but the kinetics of re-expression might be different in CD4 and CD8 T cells. It is also feasible that recruitment of T cells expressing low levels of CD127 occurs predominantly at higher dose levels.
A single administration of rhIL-7 in this study led to significant expansion of CD4+ and CD8+ T cells at day 14 after injection. These increases were seen predominantly in the central memory and to a lesser extent in the naive subsets. Although this trend was expected, as naive and central memory T cells usually express the IL-7 receptor alpha chain CD127+, this finding is of interest as it suggests that administration of rhIL-7 may counteract the progressive depletion of naive and central memory T cells that is considered a key immunologic dysfunction in HIV-infected individuals.37-39 Although all T-cell subsets seemed to proliferate in response to rhIL-7 (as measured by increased Ki67 expression), it is possible that concomitant cell death disproportionally affected the effector memory pool of T cells. Although we did not observe significant increases in levels of Bcl-2 in total CD4+ or total CD8+ T cells, differential induction of this survival molecule in distinct T-cell subpopulations was not measured, and may have explained these findings.33 It is also possible that Bcl-2 induction may require repeated dosing in humans. Alternatively, cells activated by rhIL-7 to express Bcl2 (and to expand) were also those most likely to disappear rapidly from the circulation. Since our observations were limited to analyses of peripheral blood, the potential impact of rhIL-7 on tissue redistribution of lymphocyte subpopulations was not addressed by these data. Moreover, whereas tetramer/peptide-binding CD8+ T cells were also induced to enter cell cycle, there were no significant changes in their phenotype or in their absolute counts at day 28. It is possible that this was due to the timing of collection of PBMCs used for this analysis at baseline, day 4, and day 28, which did not coincide with the observed T-cell expansions in the peripheral blood seen on day 14. Nevertheless, there was clear evidence of induction of cycling of tetramer/peptide-binding CD8 T cells albeit at a lower level than that observed in total CD8+ T cells likely due to their lower levels of CD127 expression.
Although IL-7 has a defined role in mouse B-cell lymphopoiesis, the role of IL-7 in human B-cell development may be redundant because children with X-linked severe combined immunodeficiency syndrome (SCID) have normal B-cell development despite the lack of canonical IL-7 signaling.40 Malaspina et al6,25 have described an immature/transitional B-cell phenotype in both HIV-infected individuals as well as in patients with idiopathic CD4+ T lymphopenia. These cells are prone to intrinsic apoptosis due to reduced expression of Bcl-2 and Bcl-xL,41 and their frequency is correlated directly with serum levels of IL-7.25 In the present study, a single injection of rhIL-7 led to the emergence of this phenotype, showing clearly that IL-7 can affect maturation of circulating human B cells. Unfortunately, the persistence of this phenotypic change could not be assessed due to the limited follow-up in this study; this should be carefully monitored in future studies. It is also unclear what functional and/or clinical effects, if any, may be associated with these phenotypic B-cell changes.
In conclusion, our study has demonstrated that a single subcutaneous dose of rhIL-7 is well tolerated in HIV-infected persons receiving antiretroviral therapy. There was significant evidence of biologic activity at even the lowest dose tested, and there was no evidence of sustained increases in plasma viremia. Significant increases in circulating T-cell numbers particularly of central memory phenotype were observed. The concurrent increased entry of these cells into cell cycle indicated that rhIL-7 could provide a robust strategy to amplify numbers of immune competent cells and enhance immune effector function through replenishing the pool of naive and central memory T cells. Sportes et al33 clearly demonstrated in cancer patients the potential of repeated doses of rhIL-7 to drive polyclonal expansion of T cells and expansion of naive CD4+ and CD8+ T cells enriched for thymic emigrants. Our failure to demonstrate naive CD4+ T-cell expansion in our study may be a consequence of the single-dose strategy we used. The emergence of immature/transitional B cells will require close follow-up since the persistence and clinical significance of these cells are unclear. The simultaneous CD4+ and CD8+ T-cell expansions associated with proliferation of both naive and memory subsets could offer a therapeutic strategy for HIV-infected persons who do not achieve adequate immunologic reconstitution while receiving antiretroviral therapy. In addition, the absence of proportional increases in Tregs seen in this study as well as in an earlier trial among cancer patients16 suggests the possibility that rhIL-7 administration may enhance antigen-specific immune responses through effects distinguishable from those of IL-2. However, a failure of Treg expansion could also permit emergence of autoimmunity or other immune dysregulation with continuous long-term use. Finally, the biologic activity and low toxicity of rhIL-7 as seen in the present study with HIV-infected individuals suggest that this cytokine may have value for treatment of other conditions associated with T lymphocytopenia.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors thank all study participants and clinical staff in participating sites, Roy Matining for statistical support, Esmé K. Farley (Genelogic, Gaithersburg, MD) for performing the pharmacokinetic blood level assays, and Dr Anthony S. Fauci for review of the paper.
This study was supported in part by the AIDS Clinical Trials Group funded by the National Institute of Allergy and Infectious Diseases; the Statistical and Data Analysis Center (AI 38855); and the individual AIDS Clinical Trials Units at Case Western Reserve University (AI 25879, AI 68636), Northwestern University (AI 25915), University of California, Davis Medical Center (AI 38858), and University of Miami (AI 27675). This work was also supported in part by the Intramural Research Program of the National Institutes of Health, National Institute of Allergy and Infectious Diseases, and Cytheris, Issy les Moulineaux, France. G.S. was supported by a grant from the Concerned Parents for AIDS Research.
National Institutes of Health
Authorship
Contribution: I.S. and M.M.L. wrote the paper and contributed to study planning, design and execution, and data interpretation; R.M.D. performed experiments, analyzed data, and wrote parts of the paper; K.M. designed and organized laboratory experiments and assisted in paper preparation; C.A.B. assisted in study planning and execution; J.D.A. provided reagents and assisted in paper preparation; S.M. and A.M. designed and performed experiments and contributed to data analysis and interpretations and paper preparation; R.B. and M.M. contributed to study design and execution and paper preparation and provided study drug; L.F. assisted in study design and monitoring and paper preparation; G.S., S.P., and A.L.L. contributed in study planning, design and execution, data interpretation, and paper preparation; A.R.T., M.A.F., and D.M.A. contributed in study planning, design, data interpretation, and paper preparation; statistical analysis was performed as follows: E.A., J.S., and R.M.D. analyzed the baseline characteristics of study participants, and clinical (toxicity, CD4 and CD8 T-cell counts, HIV RNA) and real-time flow cytometry data; M.A.P. analyzed all data generated from cryopreserved PBMCs (B-cell phenotype and expression of Ki67 by T-cell subsets); and E.A. and J.S. contributed also in study design and execution and paper preparation.
A complete list of ACTG 5214 Study Team members can be found in the Supplemental Appendix, available on the Blood website.
Conflict-of-interest disclosure: Two coauthors had financial interest in Cytheris capital: M.M. is the founder and Chief Executive Officer and R.B. was an employee of Cytheris. M.A.F., A.R.T., and M.M.L. have received research support from Cytheris. The remaining authors declare no competing financial interests.
Correspondence: Irini Sereti, NIAID, 10 Center Dr, Bldg 10, Rm 11B-107A, Bethesda, MD, 20892; e-mail: isereti@niaid.nih.gov.



 ) and ▲ represents rhIL-7 participants (
) and ▲ represents rhIL-7 participants ( ). (B) CD4+ and CD8+ T-cell changes from baseline according to rhIL-7 dose group. ● represents placebo participants (
). (B) CD4+ and CD8+ T-cell changes from baseline according to rhIL-7 dose group. ● represents placebo participants (