In this issue, Desmarets and colleagues examine whether transfused RBCs themselves participate in priming the immune response against subsequent allogeneic BMT.1
An early conundrum in clinical transplantation was that previous red blood cell (RBC) transfusions may reduce the risk of solid organ transplant rejection but increase the risk of bone marrow graft failure in patients undergoing bone marrow transplantation (BMT) for aplastic anemia.2 Because RBCs do not express the major histocompatibility complex (MHC), the hypothesis was that leukocytes present in the blood products were responsible for alloimmunization causing marrow graft rejection.3 Studies in the canine model demonstrated that leukocyte depletion of RBC products mitigated the alloimmunization by transfusions and permitted engraftment.4 It is therefore good practice to transfuse patients who are candidates for BMT exclusively with leukocyte-reduced blood products. Although leukocyte depletion reduced the risk of graft failure associated with previous transfusion, the risk has not been eliminated,5 particularly in the setting of reduced-intensity preparative regimens for patients with hemoglobinopathies. In addition to alloimmunization, other explanations for poorer outcomes in patients with extensive transfusion histories include iron overload, hepatitis from blood-borne infections, and that more transfusions reflect more severe underlying diseases.6
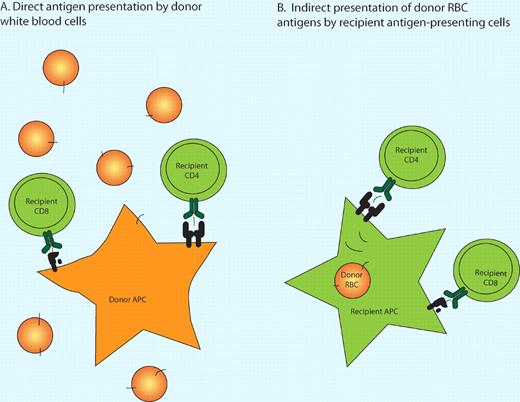
Two mechanisms of alloimmunization by RBC transfusions. (A) In the direct pathway of antigen presentation, residual donor leukocytes in the RBC product present endogenous minor histocompatibility antigens to recipient T cells. (B) In the indirect pathway, recipient antigen-presenting cells take up donor RBCs that express minor histocompatibility antigens and process and present these donor epitopes to recipient T cells. Cross-presentation permits exogenous epitopes to be presented in the context of class I MHC antigens.
Two mechanisms of alloimmunization by RBC transfusions. (A) In the direct pathway of antigen presentation, residual donor leukocytes in the RBC product present endogenous minor histocompatibility antigens to recipient T cells. (B) In the indirect pathway, recipient antigen-presenting cells take up donor RBCs that express minor histocompatibility antigens and process and present these donor epitopes to recipient T cells. Cross-presentation permits exogenous epitopes to be presented in the context of class I MHC antigens.
Desmarets et al have re-examined this issue recognizing that, in addition to the classic, direct pathway of minor antigen presentation by donor white blood cells (WBCs), recipient antigen-presenting cells may take up and present donor minor histocompatibility antigens (mHAs). This indirect pathway could be responsible for graft rejection.7 They hypothesize that if RBCs express mHAs that are also expressed on marrow stem cells, RBCs may contribute to alloimmunization of the recipient and lead to resistance to marrow engraftment. In their murine model, as in the canine model and in clinical BMT, leukocyte reduction increases the threshold number of RBC transfusions needed to cause rejection.
To test the indirect pathway of mHA presentation, they substituted leukocyte-reduced RBCs from a strain congenic to the marrow donors, but differing in MHC, so MHC-restricted T-cell responses to minor antigens presented by residual donor leukocytes would be irrelevant to the subsequent MHC-compatible marrow transplant. These transfusions had the same effect as leukocyte-reduced RBCs from the marrow donor strain, suggesting mHA presentation by recipient antigen-presenting cells and not by residual leukocytes within the RBC products. Conversely, when the donor mice differ from the recipient mice only by the H-Y mHAs, which are expressed in WBCs (but not RBCs), leukocyte depletion almost completely prevents subsequent rejection. Thus, a clinically relevant degree of leukocyte depletion is enough to mitigate direct mHA presentation. Finally, the authors demonstrate that RBC transfusion from a mouse strain engineered to express an alloantigen exclusively on RBCs can induce antigen-specific CD8 T-cell proliferation, independent of leukocyte reduction. This finding confirms that epitopes from mHAs on transfused RBCs can be cross-presented in the indirect pathway.
If recipient antigen-presenting cells can cross-present mHAs expressed on RBCs themselves to create an immunologic barrier to subsequent BMT, then even total leukocyte depletion cannot prevent alloimmunization by repeated RBC transfusion. What next? If we are not prepared to perform BMT earlier in the management of the disease, perhaps elucidation of the cellular mechanisms of this alloimmune response may allow its prevention by immunomodulation during transfusion. Identification of the mHAs relevant for clinical BMT may allow selection of RBC donors or processing of blood products in a manner that prevents alloimmunity cross-reactive with the prospective marrow donor's stem cells. This line of research is important for the goal of developing the least toxic BMT methods that can produce durable engraftment of normal hematopoietic cells in patients with nonmalignant disorders.
Conflict-of-interest disclosure: The author declares no competing financial interests. ■