Abstract
Cytotoxic CD8+ T cells control acute viremia in many viral infections. However, most viruses that establish chronic infections evade destruction by CD8+ T cells, and regulatory T cells (Treg) are thought to be involved in this immune evasion. We have infected transgenic mice, in which Treg can be selectively depleted, with Friend retrovirus (FV) to investigate the influence of Treg on pathogen-specific CD8+ T-cell responses in vivo. We observed that Treg expansion during acute infection was locally defined to organs with high viral loads and massive activation of virus-specific effector CD8+ T cells. Experimental ablation of Treg resulted in a significant increase of peak cytotoxic CD8+ T-cell responses against FV. In addition, it prevented the development of functional exhaustion of CD8+ T cells and significantly reduced FV loads in lymphatic organs. Surprisingly, despite the massive virus-specific CD8+ T-cell response after temporary Treg depletion, no evidence of immunopathology was found. These results demonstrate the important role of Treg in controlling acute retrovirus-specific CD8+ T-cell responses, and suggest that temporary manipulation of Treg might be a possible therapeutic approach in chronic infectious diseases.
Introduction
Cytotoxic CD8+ T cells (CTLs) are critical for the control of viral replication in many virus infections. Thus, viruses that establish chronic infections have developed mechanisms to evade destruction by CTLs. We and others have recently described that retroviruses induce the expansion of regulatory T cells (Treg), which might be a strategy to suppress antiviral CTL responses.1-5 This CTL suppression is likely to be a mechanism of immune regulation of the host during infections to avoid immunopathology induced by activated CTLs. In fact, there are viral infections in which the pathology induced by the host's immune response is far more detrimental than the cytopathic consequences of the virus infection itself.6-8 Thus, for the health of an infected person, it might be more important to control acute CD8+ T cell–mediated immunopathology than to prevent persistent viral infection. In contrast, a Treg response during a virus infection itself has to be controlled in some way or a general immunosuppression of the host would be the consequence of such a response. Previous studies with parasites suggest that compartmentalization might be a mechanism to restrict Treg to sites of infection, where CTL responses have to be dampened to prevent immunopathology.9 However, studies on localization and suppressive potential of Treg during an ongoing infection in vivo were mainly performed in animal models in which Treg could not be selectively depleted because all known Treg surface markers are shared with other cell subsets of the immune system. The only unique Treg marker in the mouse is Foxp3, an intracellularly expressed transcription factor.10 In this study, we used Foxp3 transgenic mice expressing the diphteria toxin (DT) receptor under the control of the Foxp3 promoter that allows to selectively deplete Treg in vivo and thus to clarify the relevance of Treg for antiviral CD8+ T-cell responses during an ongoing retroviral infection.
We have previously used the Friend virus (FV) model to study the interaction of retroviruses with CTLs and Treg.5,11,12 FV is a retroviral complex that induces erythroleukemia in susceptible mice. In contrast, resistant strains, like the C57BL/6 mice that were used in the current study, develop potent immune responses during acute infection that allow recovery from disease.13,14 CD8+ T cells are a key component of the immune response that is critical for this recovery, as animals lacking CD8+ T cells do not control viral replication and develop severe leukemia.15-17 These CD8+ T cells use the cytotoxic molecules perforin, granzyme A, and granzyme B to kill FV-infected cells and suppress viral replication by release of interferon γ (IFNγ).18,19 However, these virus-specific CD8+ T cells lose their ability to produce cytotoxic molecules11 and to secrete IFNγ5 during chronic FV infection. The functional suppression is mediated by CD4+ Foxp3+ Treg, which expand during the late phase of acute FV infection.5,12
In the current study, we analyzed the local restriction of the Treg response during FV infection, and used the model of DT-induced depletion of Treg in the living mouse to determine the role of Treg in controlling the magnitude and duration of a virus-specific CTL response during an acute retroviral infection.
Methods
Mice
Inbred C57BL/6 and DEREG20 mice were maintained under pathogen-free conditions. Experiments were done using mice (H-2b/b, Fv1b/b, Fv2r/r) or transgenic mice backcrossed on C57BL/6 background that are resistant to FV-induced leukemia. All mice were females of 8 to 16 weeks of age at the beginning of the experiments. All animal studies were approved by the institutional review board at the University of Duisburg-Essen.
Virus and viral infection
The FV stock used in these experiment was FV complex containing B-tropic Friend murine leukemia helper virus and polycythemia-inducing spleen focus-forming virus.21 The stock was prepared as a 10% spleen cell homogenate from BALB/c mice infected 14 days previously with 3000 spleen focus-forming units (SFFU) of noncloned virus stock. Experimental mice were injected intravenously with 0.5 mL phosphate-buffered saline (PBS) containing 25 000 SFFU of FV. The virus stock was free of lactate dehydrogenase-elevating virus.
Infectious center assays
Infectious center assays were performed as described previously.22
Cell-surface and intracellular staining by flow cytometry
Cell-surface staining was performed using BD Biosciences reagents. T-cell antibodies were as follows: anti-CD43 (1B11), anti-CD4 (RM4-5), anti-CD8 (53-6.7), and anti-CD107a (1D4B). Dead cells (7-aminoactinomycin D positive) were excluded from analyses. Intracellular granzyme A (polyclonal rabbit anti–mouse granzyme A immunoglobulin G, protein A purified) and granzyme B (monoclonal anti–human granzyme B antibody allophycocyanin [APC] conjugated, clone GB12; Caltag Laboratories) staining was performed as described.12 Foxp3 expression was detected by intracellular staining using the anti–mouse/rat Foxp3 antibody (clone FJK-16s) and the Foxp3 staining set (eBioscience). Data were acquired on a LSR II flow cytometer (BD Biosciences) from 100 000 to 300 000 lymphocyte-gated events per sample. Analyses were done using CellQuest Pro and FACSDiva software (BD Biosciences).
Lymphocyte depletion
CD8+ T-cell depletions were performed essentially as described.23 Briefly, mice were inoculated 4 times intraperitoneally with 0.5 mL of supernatant fluid obtained from hybridoma cell culture for the CD8a-specific monoclonal antibody 169.4. The treatment depleted more than 95% of the CD8+ cells in all investigated organs (at 10 days postinfection).
To deplete Treg, DEREG mice were injected with diphtheria toxin (DT; Merck), diluted in endotoxin-free PBS. A total of 1 μg DT was inoculated 4 times every other day starting on the day of FV infection. The treatment depleted more than 97% of the CD4+ enhanced green fluorescent protein (GFP)+ T cells in all investigated organs of DEREG mice (at 10 days postinfection).
Tetramers and tetramer staining
For detection of Db-GagL–specific CD8+ T cells, nucleated lymph nodes, spleen, and bone marrow cells were stained with APC-labeled anti-CD8 (Ly-2), fluorescein isothiocyanate–labeled CD43 (1B11; BD Biosciences), and phycoerythrin-labeled major histocompatibility complex (MHC) class I H2-Db tetramers specific for FV GagL peptide24,25 (Beckman Coulter).
In vivo cytotoxicity assay
The in vivo CTL assay described by Barber et al26 was modified to measure cytotoxicity in FV-infected mice. Splenocytes from naive mice were loaded with 1 μM DbGagL peptide.25 These loaded cells were then stained with 200 nM 5-(and 6-)carboxyfluorescein diacetate succinimidyl ester (CFSE; Molecular Probes). As control, spleen cells without peptide were stained with 2 nM CFSE. Splenocytes were transferred intravenously (i.v.; 107 cells of each population) into naive or FV-infected mice. Two hours after the transfer of cells, lymph nodes, spleen, and bone marrow were harvested, and cell suspensions were prepared. Target cells were distinguished from recipient cells and from one another based on CFSE staining. The percentage of killing was calculated as follows: 100 − ([(% peptide pulsed in infected/% unpulsed in infected)/(% peptide pulsed in uninfected/% unpulsed in uninfected)] × 100).
Bromodeoxyuridine staining
Bromodeoxyuridine (BrdU; Sigma-Aldrich) was dissolved in water, and mice were then exposed to BrdU (0.8 mg/mL) through drinking water from day 7 up to day 10 post-FV infection. Ten days postinfection (dpi) mice were killed, and single-cell suspensions from lymph nodes, spleen, and bone marrow were prepared. BrdU incorporation was detected using the BrdU flow kit protocol (BD Biosciences). In brief, cells were surface stained for CD4 (RM4-5) and CD25 (PC61), fixed, permeabilized, refixed, and treated with DNase. After that, cells were intracellularly stained with BrdU-specific monoclonal antibody and anti–mouse/rat Foxp3 antibody (FJK-16s; eBioscience). Staining of cells with the isotype control anti–mouse immunoglobulin G1-APC and staining of cells from mice, which were not exposed to BrdU, was used as negative control. Data were acquired from 150 000 lymphocyte-gated events per sample.
Statistical analysis
Statistical data were derived using the nonparametric Student t test (GraphPad Prism software; GraphPad).
Results
Distinct replication levels of FV in different lymphatic organs
In previous studies on FV-specific immunity, viral replication and immune responses were mainly determined in the spleens of infected mice. However, FV can infect various cells of the haematopoetic system,27 and infected cells have been found in several organs of the lymphatic system.5 In this study, we compared the kinetics of viral replication in the bone marrow, spleen, and lymph nodes after infection of C57BL/6 mice with 25 000 SFFU of FV. During acute infection, virus-infected cells were detected as early as 2 dpi, and peak viral loads were reached at 7 dpi in all 3 lymphatic organs (Figure 1A). Thereafter, viral loads decreased steadily until a persistent low-level infection was established at 60 dpi. The highest level of persistent virus was measured in the spleen, but the virus was detectable in all 3 organs during chronic infection. During peak viral loads at 7 dpi, the highest levels of infection were found in the bone marrow. It was more than 15 times higher compared with the spleen and almost 300 times higher than in lymph nodes (Figure 1A).
Kinetics of FV infection and kinetics of effector CD8+ T-cell responses during acute FV infection. (A) Viral loads in lymph nodes, spleen, and bone marrow (infectious centers) were determined at different time points after FV infection. Each dot represents the mean number + SEM of virus-infected cells per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 2 independent experiments with similar results. (B) Kinetics of effector CD8+ T cells specific for the FV gagL epitope during acute FV infection. CD8+ T cells from lymph nodes, spleen, and bone marrow of FV-infected mice were stained for DbgagL class I tetramers to identify FV-specific effector T cells. Costaining experiments indicated that all tetramer-positive CD8+ T cells also expressed the CD43 activation marker (data not shown). Each dot represents the mean number + SEM of CD8+ tetramer+ T cells per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 3 independent experiments with similar results. (C-D) Flow cytometry was used to detect intracellular granzyme B or the degranulation marker CD107a in effector CD8+ T cells (CD43+). The kinetic analysis was performed at different time points after FV infection. Shown are the numbers of CD8+ T cells expressing granzyme B (GzmB; C) or CD107a (D) from lymph nodes, spleen, and bone marrow. Each dot represents the mean number + SEM per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 2 independent experiments with similar results. (E) Splenocytes from naive mice were loaded with DbGagL peptide and labeled with CFSE. Target cells were injected intravenously into naive and acutely infected (10 dpi) mice. Two hours after transfer, donor cells from lymph nodes, spleen, and bone marrow were analyzed. The figure shows the percentage of target cell killing in the investigated organs. Three independent experiments with similar results were performed. Differences between investigated organs were analyzed by the unpaired Student t test. Statistically significant differences between the organs are indicated in the figure. (F-G) Splenocytes from naive mice were loaded with DbGagL peptide and labeled with CFSE. Target cells were injected intravenously into naive mice and in mice at different time points after FV infection. The figure shows the percentage of target cell killing at different time points after FV infection in the spleen (F) and in bone marrow (G). Two independent experiments with similar results were performed.
Kinetics of FV infection and kinetics of effector CD8+ T-cell responses during acute FV infection. (A) Viral loads in lymph nodes, spleen, and bone marrow (infectious centers) were determined at different time points after FV infection. Each dot represents the mean number + SEM of virus-infected cells per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 2 independent experiments with similar results. (B) Kinetics of effector CD8+ T cells specific for the FV gagL epitope during acute FV infection. CD8+ T cells from lymph nodes, spleen, and bone marrow of FV-infected mice were stained for DbgagL class I tetramers to identify FV-specific effector T cells. Costaining experiments indicated that all tetramer-positive CD8+ T cells also expressed the CD43 activation marker (data not shown). Each dot represents the mean number + SEM of CD8+ tetramer+ T cells per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 3 independent experiments with similar results. (C-D) Flow cytometry was used to detect intracellular granzyme B or the degranulation marker CD107a in effector CD8+ T cells (CD43+). The kinetic analysis was performed at different time points after FV infection. Shown are the numbers of CD8+ T cells expressing granzyme B (GzmB; C) or CD107a (D) from lymph nodes, spleen, and bone marrow. Each dot represents the mean number + SEM per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 2 independent experiments with similar results. (E) Splenocytes from naive mice were loaded with DbGagL peptide and labeled with CFSE. Target cells were injected intravenously into naive and acutely infected (10 dpi) mice. Two hours after transfer, donor cells from lymph nodes, spleen, and bone marrow were analyzed. The figure shows the percentage of target cell killing in the investigated organs. Three independent experiments with similar results were performed. Differences between investigated organs were analyzed by the unpaired Student t test. Statistically significant differences between the organs are indicated in the figure. (F-G) Splenocytes from naive mice were loaded with DbGagL peptide and labeled with CFSE. Target cells were injected intravenously into naive mice and in mice at different time points after FV infection. The figure shows the percentage of target cell killing at different time points after FV infection in the spleen (F) and in bone marrow (G). Two independent experiments with similar results were performed.
The kinetics of CD8+ T-cell responses in different lymphatic organs after FV infection
To compare the kinetics of FV replication with antiviral CD8+ T-cell responses, effector CD8+ T cells were analyzed in the spleen, lymph nodes, and bone marrow. As a marker for effector CD8+ T cells, the activation-associated glycoform of CD43 was used.11,12 In previous studies, CD8+ CD43+ T cells from FV-infected mice also expressed the other effector cell markers, CD44 and CD69, and were negative for CD62L.12
In FV-infected mice, the absolute numbers of CD43+ cells among the CD8+ T-cell population increased over time until it peaked in the spleen at 10 dpi and in the bone marrow and lymph nodes at 12 dpi (supplemental Figure 1A, available on the Blood website; see the Supplemental Materials link at the top of the online article). Reflecting the levels of viral loads in the different organs, the highest absolute number of CD8+ CD43+ T cells was found in the bone marrow, which was more than 2 times higher than in the spleen and approximately 2.5 times higher compared with lymph nodes. To assure viral specificity of this CD8+ T-cell response, effector T cells were stained with a MHC class I tetramer specific for the H-2Db–restricted Friend murine leukemia helper virus–glycosylated gag epitope.24 CD8+ tetramer+ T cells were not detected during the first 7 dpi (Figure 1B). However, shortly thereafter at 10 dpi, the CD8+ tetramer+ T-cell response peaked in the spleen and bone marrow. Peak tetramer+ CD8+ T-cell numbers in lymph nodes were observed at 15 dpi. All tetramer+ cells were also positive for the effector cell marker CD43+ (data not shown). The peak virus-specific CD8+ T-cell response against the FVgag epitope in the bone marrow was nearly 3 times higher than in the spleen and more than 20 times higher than in lymph nodes. After peak expansion of virus-specific CD8+ T cells, a contraction phase of the CD8+ T-cell response was found in all organs, but CD8+ tetramer+ T cells remained detectable throughout the chronic phase of infection in the spleen and bone marrow (Figure 1B).
To analyze functional properties of effector CD8+ T cells during FV infection, production of the cytotoxic molecules granzyme A and B and surface expression of the degranulation marker CD107a28,29 were determined (Figure 1C-D and supplemental Figure 1B). The highest numbers of CD8+ CD43+ T cell–expressing granzymes were measured within the first 2 days after the peak virus-specific CD8+ T-cell response (Figure 1C and supplemental Figure 1B). In addition, at 12 dpi, peak degranulation of cytotoxic molecules by effector CD8+ T cells was found by analyzing CD107a expression (Figure 1D). The highest number of granzyme or CD107a-expressing CD8+ CD43+ T cells was again detected in the bone marrow, followed by the spleen and the lymph nodes. The cytotoxic potential of the CD8+ T cells was analyzed by an in vivo CTL assay (Figure 1E). Spleen cells from a noninfected mouse were loaded with the FV-specific DbGagL peptide, labeled with CFSE, and injected i.v. into FV-infected recipient mice at 10 dpi. As negative control, CFSE-labeled cells without peptide were cotransferred. In the infected recipient mice, approximately 32% of the labeled cells were eliminated in the lymph nodes after 2 hours. The average killing in the spleen and bone marrow was significantly higher with 60% and 73%, respectively. These results demonstrate that there was a clear correlation between the magnitude of the CD8+ T-cell response in the 3 different organs and the magnitude of target cell killing. Kinetic studies of the CTL-mediated killing in the spleen (Figure 1F) and bone marrow (Figure 1G) revealed that it was still very effective at 15 dpi, but decreased at 20 dpi. This was slightly delayed in comparison with the decrease in granzyme and CD107a expression by CD8+ T cells, which might be explained by the high effector to target cell ratio in the described in vivo CTL assay.
The results indicate that the expansion of virus-specific CD8+ T cells and their functional properties in different organs of FV-infected mice were strictly correlated to the levels of viral replication. In addition, as reported previously,12 between the second and the third week postinfection, a functional impairment of the effector CD8+ T cells developed.
Kinetics of Treg responses in different lymphatic organs during FV infection
We have previously reported that Treg expand in the spleen after FV infection and that this expansion correlates with suppression of CD8+ T-cell responses.5,12 In this study, the kinetics of Treg responses in various lymphatic organs were compared. Treg were stained for the intracellular expression of Foxp3, the only unique marker for Treg. In naive mice, almost 4% of the total lymph node cells were Foxp3+ (Figure 2A). In contrast, only 2% of the splenocytes were Foxp3+ and less than 0.5% of the cells in the bone marrow of uninfected mice were Treg (Figure 2B-C). After FV infection, very little expansion of the Treg in comparison with naive mice (P > .05 at 7 dpi) was detected in lymph nodes (Figure 2A). In the spleen, a significant expansion of Treg was found at 10 dpi (P = .0005) and thereafter, which was shortly after peak viral loads in this organ. The most pronounced expansion of Treg after FV infection was detected in the bone marrow (P = .001). At 10 dpi, an expansion of almost 300% of the Foxp3+ cell population was found. This was 3 days after peak viral loads and contemporaneous with the peak of the CD8+ T-cell response. Thus, the magnitude of Treg expansion was associated with the level of viral replication and the strength of the CD8+ T-cell response in the different lymphatic organs. To determine whether or not different viral loads within the same organ can influence the magnitude of Treg expansion, we infected mice with various inoculation doses of FV. As expected, the challenge dose influenced the viral loads in all 3 lymphatic organs, with highest levels of infection being detected after inoculation of the highest FV dose (data not shown; Zelinskyy et al30 ). Increasing infection doses resulted in a gradual increase in the level of Treg expansion in the spleen and bone marrow (Figure 3A). In contrast, increasing viral loads in lymph nodes did not result in greater expansion of Treg, which might be associated with the high number of Treg that were already present in the lymph nodes of noninfected mice (Figure 2A). However, the analysis of spleens and bone marrow clearly demonstrated that the magnitude of Treg expansion correlated with the level of FV replication in these 2 lymphatic organs.
Expansion of Treg during infection with FV. Flow cytometry was used to quantify CD4+ Foxp3+ Treg in lymph nodes (A), spleen (B), and bone marrow (C) of naive mice and at different time points after infection with FV. Each column represents mean absolute numbers plus SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 3 independent experiments with similar results. Differences between naive mice and mice infected for 10 days with FV were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure.
Expansion of Treg during infection with FV. Flow cytometry was used to quantify CD4+ Foxp3+ Treg in lymph nodes (A), spleen (B), and bone marrow (C) of naive mice and at different time points after infection with FV. Each column represents mean absolute numbers plus SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells for a group of 5 to 10 mice. Data were pooled from 3 independent experiments with similar results. Differences between naive mice and mice infected for 10 days with FV were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure.
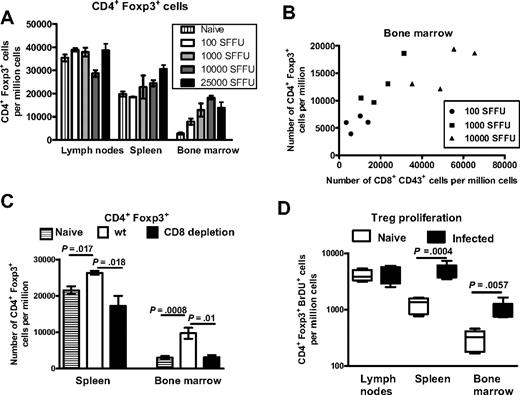
Influence of the level of viral replication and the magnitude of the CD8+ T-cell response on the expansion of Treg during FV infection. (A) Mice were infected with 4 different doses of FV (100; 1000; 10 000; 25 000 SFFU) to investigate the role of the viral inoculation dose on the expansion of Treg. Flow cytometry was used to detect numbers of CD4+ Foxp3+ Treg in lymph nodes, spleen, and bone marrow at 10 dpi. Each column represents mean numbers + SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells for a group of 6 mice. Data were pooled from 2 independent experiments with similar results. (B) Numbers of CD4+ Foxp3+ Treg were plotted against numbers of CD8+ CD43+ T cells in the bone marrow of mice at 10 dpi with different doses of FV. Each symbol represents an individual mouse. Pearson 1-grouping variable tables correlation analysis was performed for the numbers of CD4+ Foxp3+ Treg and CD8+ CD43+ T cells for individual mice (r = 0.7886; P = .0039). A representative experiment is shown. The experiment was repeated twice with similar results. (C) Mice were infected with 25 000 SFFU of FV and depleted for their CD8+ T ells by injecting monoclonal antibody 169.4. At 10 dpi, numbers of CD4+ Foxp3+ Treg were determined by flow cytometry in the spleen and bone marrow. Each column represents mean numbers + SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells for a group of 5 to 7 mice. Data were pooled from 2 independent experiments with similar results. Differences between the 2 groups were analyzed using the Mann-Whitney test. Statistically significant differences between the groups are indicated in the figure. (D) Noninfected mice (□) and mice at day 7 post-FV infection (■) were exposed to BrdU in drinking water. At 10 dpi, cells from lymph nodes, spleen, and bone marrow were stained for CD4, CD25, Foxp3, and incorporated BrdU. The figure shows mean numbers + SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells positive for BrdU in the 3 different organs of naive and FV-infected mice. Six mice per group were analyzed. The experiment was repeated twice with similar results. Differences between naive mice and mice infected for 10 days with FV were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure.
Influence of the level of viral replication and the magnitude of the CD8+ T-cell response on the expansion of Treg during FV infection. (A) Mice were infected with 4 different doses of FV (100; 1000; 10 000; 25 000 SFFU) to investigate the role of the viral inoculation dose on the expansion of Treg. Flow cytometry was used to detect numbers of CD4+ Foxp3+ Treg in lymph nodes, spleen, and bone marrow at 10 dpi. Each column represents mean numbers + SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells for a group of 6 mice. Data were pooled from 2 independent experiments with similar results. (B) Numbers of CD4+ Foxp3+ Treg were plotted against numbers of CD8+ CD43+ T cells in the bone marrow of mice at 10 dpi with different doses of FV. Each symbol represents an individual mouse. Pearson 1-grouping variable tables correlation analysis was performed for the numbers of CD4+ Foxp3+ Treg and CD8+ CD43+ T cells for individual mice (r = 0.7886; P = .0039). A representative experiment is shown. The experiment was repeated twice with similar results. (C) Mice were infected with 25 000 SFFU of FV and depleted for their CD8+ T ells by injecting monoclonal antibody 169.4. At 10 dpi, numbers of CD4+ Foxp3+ Treg were determined by flow cytometry in the spleen and bone marrow. Each column represents mean numbers + SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells for a group of 5 to 7 mice. Data were pooled from 2 independent experiments with similar results. Differences between the 2 groups were analyzed using the Mann-Whitney test. Statistically significant differences between the groups are indicated in the figure. (D) Noninfected mice (□) and mice at day 7 post-FV infection (■) were exposed to BrdU in drinking water. At 10 dpi, cells from lymph nodes, spleen, and bone marrow were stained for CD4, CD25, Foxp3, and incorporated BrdU. The figure shows mean numbers + SEM of CD4+ Foxp3+ Treg per 1 million nucleated cells positive for BrdU in the 3 different organs of naive and FV-infected mice. Six mice per group were analyzed. The experiment was repeated twice with similar results. Differences between naive mice and mice infected for 10 days with FV were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure.
However, these experiments do not answer the question of whether the level of viral replication or the subsequent CD8+ T-cell response resulted in Treg expansion. When the numbers of CD4+ Foxp3+ Treg were compared with the numbers of CD8+ CD43+ effector T cells in the bone marrow of mice infected with graduate doses of FV, a clear correlation was found (Figure 3B), suggesting that the magnitude of the CD8+ T-cell response might influence the level of Treg expansion. To investigate whether or not the presence of CD8+ T cells was essential for Treg expansion in the bone marrow and spleen, we depleted these cells by monoclonal antibodies during acute FV infection. The depletion protocol we used ablated more than 95% of all CD8+ T cells in both organs, but numbers of CD8-expressing dendritic cells (DC; CD11c-positive cells) were only reduced by 50% in the spleen and 15% in the bone marrow (data not shown). At 10 dpi, the expansion of Foxp3-expressing Treg was completely lost when CD8+ T cells were depleted from the spleen and bone marrow (Figure 3C). An involvement of DC in Treg expansion was unlikely because of the incomplete depletion of CD8+ DC by the monoclonal antibody. Thus, the antiviral CD8+ T-cell response was an essential factor involved in the expansion of Treg during acute FV infection. In contrast, viral replication alone, which was increased in CD8+ T cell–depleted mice compared with nondepleted mice (data not shown; Zelinskyy et al30 ), did not result in Treg expansion.
The expansion of Treg in organs with vigorous CD8+ T-cell responses might be mediated by recruitment and/or proliferation of these cells. To analyze whether Treg undergo proliferation at the different sites of infection, we stained proliferating cells by adding BrdU to the drinking water of naive and FV-infected mice. In noninfected control mice, the level of homeostatic Treg proliferation was different in lymph nodes, spleen, and bone marrow (Figure 3D). The highest number of proliferating Treg in noninfected mice was found in lymph nodes, and the lowest in the bone marrow. After infection, no increase in the proliferation was found in lymph nodes, whereas a significant increase in BrdU-positive Treg numbers was observed in the spleen and bone marrow. Thus, we observed a clear correlation between the expansion of Treg and their rate of proliferation in the investigated lymphatic organs after FV infection. To investigate whether de novo induction of Treg from Foxp3-negative CD4+ T cells occurred during FV infection, GFP-negative cells from naive DEREG mice were transferred into FV-infected wild-type recipients. At 10 dpi, the lymphatic organs were harvested, and several million cells were analyzed for induced expression of GFP. However, no significant conversion of Foxp3− CD4+ T cells to Treg was found (supplemental Figure 2). Even when Foxp3− cells from T-cell receptor transgenic mice,31 which were in part FV specific, were transferred, no conversion to Treg was found (data not shown). The data strongly suggest that proliferation rather than conversion of helper T cells to Treg plays an important role for Treg expansion during viral infections.
The role of Treg in controlling virus-specific CD8+ T-cell responses in vivo
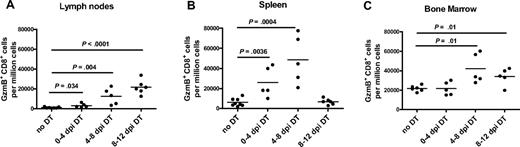
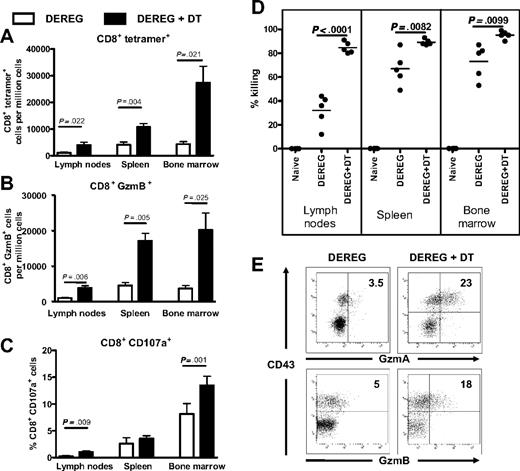
To prove that Treg control peak CD8+ T-cell responses and subsequent CD8+ T-cell dysfunction in vivo, we used a mouse model in which Foxp3-expressing Treg can be experimentally depleted. Injection of DT into DEREG mice20 that express the DT receptor under the control of the Foxp3 promoter depleted more than 95% of the Treg in all 3 investigated organs (data not shown). Only Treg and no other cell population was affected by this treatment.32 This effect of DT was only observed in DEREG mice, and no influence of DT on the T-cell repertoire or the FV-specific T-cell response was found in infected wild-type C57BL/6 mice (data not shown). If depletion of Treg was performed in DEREG mice during acute FV infection, peak CD8+ T-cell responses were dramatically enhanced (Figure 4A-C). At 10 dpi, significantly more virus-specific CD8+ T cells were present in all 3 organs compared with FV-infected nondepleted DEREG mice. A comparison of the different organs revealed that the enhancement of CD8+ T-cell responses after Treg depletion was the highest in organs with most prominent Treg expansion. For example, in the bone marrow of FV-infected mice, where the most significant expansion of Treg was found, the depletion of Treg in infected DEREG mice resulted in the most predominant enhancement of the CD8+ T-cell response. In addition to the increase of the overall numbers of virus-specific CD8+ T cells after Treg depletion, a lack of Treg also improved the function of the CD8+ T cells. At their peak response, significantly more CD8+ T cells with CD43+ effector phenotype produced granzyme B and expressed the CD107a degranulation marker when suppressive Treg were ablated (Figure 4B-C). This was seen in all 3 lymphatic organs analyzed, but was again most pronounced in the spleen and bone morrow. The increased expression and degranulation of cytotoxic molecules correlated with increased FV-specific in vivo CTL activity after Treg depletion (Figure 4D). As described above, cells were loaded with a CTL epitope peptide, labeled with CFSE, and injected i.v. into FV-infected nondepleted or Treg-depleted recipient DEREG mice at 10 dpi. In all 3 investigated organs, depletion of Treg resulted in a significant increase of target cell killing. More than 80% of all target cells were eliminated in the 3 organs of infected mice when no Treg were present, with the highest percentage of killing measured in the bone marrow. The result clearly indicates enhanced virus-specific cytolytic activity of CD8+ T cells in FV-infected mice after ablation of Treg. To determine whether Treg ablation also influenced the functional impairment of effector CD8+ T cells that develops after the second week of FV infection, we analyzed the expression of granzymes in CD8+ T cells with CD43+ effector phenotype from the bone marrow at 15 dpi. As reported previously,12 CD8+ T cells from FV-infected mice showed a reduced granzyme expression at this time point (Figure 4E). In contrast, Treg-depleted mice showed vigorous expression of granzymes in CD8+ CD43+ T cells. Thus, Treg depletion did not only result in augmentation of peak cytotoxic CD8+ T-cell responses, but also prevented the onset of CD8+ T-cell dysfunction during the late phase of acute FV infection. To determine at what time point during FV infection Treg suppress the peak CD8+ T-cell response, we depleted Foxp3+ cells by DT injection during different phases of the acute infection. To measure functional properties of effector CD8+ T cells, we determined absolute numbers of CD43+ granzyme B-producing cells at 12 dpi (Figure 5). Early depletion of Treg (0-4 dpi) only resulted in an increase of CD8+ T-cell responses in the spleen and lymph nodes, the 2 organs in which significant numbers of Treg were already found before FV infection (Figure 2). In the bone marrow, only Treg ablation during the phase of Treg expansion had an effect on CD8+ T-cell responses. In the spleen and bone marrow, where Treg expand during infection, the most significant effect of Treg on CD8+ cells was found after depletion from days 4 to 8 after infection. Because it takes approximately 3 additional days after the last DT injection for the first Treg to reappear (data not shown), this time point correlates nicely with the peak CD8+ T-cell response after FV infection (Figure 1). However, it remains elusive why late depletion (8-12 dpi) of Treg did not influence the CD8+ T-cell response in the spleen, whereas it significantly influenced the response in the bone marrow.
CD8+ T-cell responses in Foxp3+ Treg-depleted DEREG mice. (A-C) FV-infected DEREG mice were treated with DT to deplete Foxp3+ Treg during the first 10 days of infection (■). Control mice were FV infected, but received PBS instead of DT (□). Flow cytometry was used to determine the absolute numbers of CD43+ effector CD8+ T cells reactive with DbgagL class I tetramers (A), or granzyme B (GzmB; B), or the percentage of cells expressing the degranulation marker CD107a (C) in lymph nodes, spleen, and bone marrow at the peak of the FV-specific CD8+ T-cell response (10 dpi). Each column represents mean numbers + SEM per 1 million nucleated cells for a group of 5 to 7 mice. Data were pooled from 2 independent experiments with similar results. Differences between the groups were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure. (D) Splenocytes from naive mice were loaded with DbGagL peptide and labeled with CFSE. Target cells were injected intravenously into naive mice, DEREG mice infected for 10 days, and in 10-day FV-infected DEREG mice that were treated with DT. The figure shows the percentage of target cell killing in lymph nodes, spleen, and bone marrow. Each dot represents an individual mouse. Two independent experiments with similar results were performed. Differences between nondepleted and Treg-depleted groups were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure. (E) Granzyme expression by effector CD8+ CD43+ T cells from the bone marrow of FV-infected Treg-depleted and nondepleted DEREG mice is shown at 15 dpi. The mean percentages of CD8+ T cells that were positive for granzyme A or granzyme B are given in the top right quadrants. A representative mouse from a group of 6 animals is shown. The experiment was repeated twice with similar results.
CD8+ T-cell responses in Foxp3+ Treg-depleted DEREG mice. (A-C) FV-infected DEREG mice were treated with DT to deplete Foxp3+ Treg during the first 10 days of infection (■). Control mice were FV infected, but received PBS instead of DT (□). Flow cytometry was used to determine the absolute numbers of CD43+ effector CD8+ T cells reactive with DbgagL class I tetramers (A), or granzyme B (GzmB; B), or the percentage of cells expressing the degranulation marker CD107a (C) in lymph nodes, spleen, and bone marrow at the peak of the FV-specific CD8+ T-cell response (10 dpi). Each column represents mean numbers + SEM per 1 million nucleated cells for a group of 5 to 7 mice. Data were pooled from 2 independent experiments with similar results. Differences between the groups were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure. (D) Splenocytes from naive mice were loaded with DbGagL peptide and labeled with CFSE. Target cells were injected intravenously into naive mice, DEREG mice infected for 10 days, and in 10-day FV-infected DEREG mice that were treated with DT. The figure shows the percentage of target cell killing in lymph nodes, spleen, and bone marrow. Each dot represents an individual mouse. Two independent experiments with similar results were performed. Differences between nondepleted and Treg-depleted groups were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure. (E) Granzyme expression by effector CD8+ CD43+ T cells from the bone marrow of FV-infected Treg-depleted and nondepleted DEREG mice is shown at 15 dpi. The mean percentages of CD8+ T cells that were positive for granzyme A or granzyme B are given in the top right quadrants. A representative mouse from a group of 6 animals is shown. The experiment was repeated twice with similar results.
CD8+ T-cell responses of DEREG mice, which were depleted of Foxp3+ Treg at different time points post-FV infection. (A-C) FV-infected DEREG mice were treated with DT to deplete Foxp3+ Treg at different time points during infection (0-4, 4-8, or 8-12 dpi). Control mice were FV infected, but received PBS instead of DT (no DT). Flow cytometry was used to determine the absolute numbers of CD8+ T cells expressing intracellular granzyme B (GzmB) per 1 million nucleated cells in lymph nodes, spleen, and bone marrow at the peak of the FV-specific CD8+ T-cell response (12 dpi). Each dot represents an individual mouse. Data were pooled from 2 independent experiments with similar results. Differences between the groups were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure.
CD8+ T-cell responses of DEREG mice, which were depleted of Foxp3+ Treg at different time points post-FV infection. (A-C) FV-infected DEREG mice were treated with DT to deplete Foxp3+ Treg at different time points during infection (0-4, 4-8, or 8-12 dpi). Control mice were FV infected, but received PBS instead of DT (no DT). Flow cytometry was used to determine the absolute numbers of CD8+ T cells expressing intracellular granzyme B (GzmB) per 1 million nucleated cells in lymph nodes, spleen, and bone marrow at the peak of the FV-specific CD8+ T-cell response (12 dpi). Each dot represents an individual mouse. Data were pooled from 2 independent experiments with similar results. Differences between the groups were analyzed by the unpaired Student t test. Statistically significant differences between the groups are indicated in the figure.
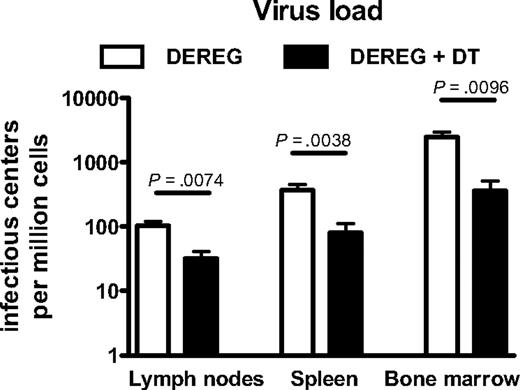
To determine whether augmented CD8+ T-cell responses in Treg-depleted mice (depletion from 0 to 10 dpi) resulted in superior control of viral replication, viral loads of FV-infected depleted versus nondepleted DEREG mice were compared at 10 dpi. In all 3 organs investigated, viral loads were significantly reduced in Treg-depleted mice (Figure 6). These results indicate that the suppression of CD8+ T-cell responses by Treg negatively influences the control of viral replication during an acute retroviral infection. However, even CD8+ T-cell responses that were not suppressed by Treg were not sufficient to completely eliminate the virus (Figure 6). In addition, DEREG mice that were depleted for Treg during acute infection were not resistant against development of chronic FV infection (data not shown).
Viral loads in Foxp3+ Treg-depleted and nondepleted DEREG mice. Lymph nodes, spleen, and bone marrow from nondepleted (□) and Foxp3+ Treg-depleted (+DT; ■) DEREG mice were assayed for viral loads at 10 dpi. Each column represents a mean number + SEM of infected cells per 1 million nucleated cells for a group of 5 to 7 mice. Data were pooled from 2 independent experiments with similar results. Differences between the groups were analyzed using Student t test. Statistically significant differences between the groups are indicated in the figure.
Viral loads in Foxp3+ Treg-depleted and nondepleted DEREG mice. Lymph nodes, spleen, and bone marrow from nondepleted (□) and Foxp3+ Treg-depleted (+DT; ■) DEREG mice were assayed for viral loads at 10 dpi. Each column represents a mean number + SEM of infected cells per 1 million nucleated cells for a group of 5 to 7 mice. Data were pooled from 2 independent experiments with similar results. Differences between the groups were analyzed using Student t test. Statistically significant differences between the groups are indicated in the figure.
The question remained whether the negative effect of Treg on antiviral immunity was accepted by the host to avoid immunopathology mediated by massive CD8+ T-cell responses. To test this hypothesis, we depleted FV-infected DEREG mice for 10 days and performed extensive histology of several different organs at 15 dpi. Similar to FV-infected wild-type B6 mice, DEREG mice developed a mild splenomegaly after FV infection. The severity to splenomegaly was not affected by the depletion of Treg after DT injection (data not shown). However, lymph nodes from FV-infected DEREG mice showed a severe hyperplasia when Treg were depleted, whereas lymph nodes from nondepleted, infected DEREG mice showed no or only mild hyperplasia (supplemental Figure 3A). The hyperplasia was mediated by a massive increase in CD3+ T-cell numbers, but also increased B220+ B-cell numbers in lymph nodes after Treg ablation in FV-infected mice (supplemental Figure 3B).
However, the massive virus-specific CD8+ T-cell response after Treg depletion did not result in severe immunopathology during acute infection. Intensive pathohistologic analysis of the kidney, liver, gut, and joints did not reveal any signs of emerging autoimmune diseases within the first 15 dpi (data not shown). Thus, it might be possible to deplete Treg in certain acute viral infections as a new therapeutic approach without dramatic pathologic consequences for the host.
Discussion
To survive an infection, a host needs to generate an efficient immune response against the invading pathogen, but at the same time needs to limit possible immunopathology induced by exuberant lymphocyte responses. Treg play a very important role in balancing these 2 contradictory effects occurring in most infectious diseases. They prevent immunopathology by dampening pathogen-specific immune responses. However, this might lead to enhanced pathogen survival.33 In the current study, we used a transgenic mouse model, in which Treg could be specifically depleted, to show that indeed the Treg response tidily controls the antiviral CD8+ T-cell response during an acute retroviral infection.
In previous studies using the FV model, we showed that this retrovirus induces an expansion of Treg during acute infection,12 which correlates with significant impairment of the antiviral effector functions of CD8+ T cells.5,12 To avoid a generalized immunosuppression after an infection, a compartmentalization of Treg responses to the sites of inflammation would be desirable for an infected host. Siegmund et al have shown that inflamed tissues are, indeed, the sites of active Treg-mediated suppression of immune responses in vivo.34 Along these lines, in ocular herpes viral infections, Treg accumulate at the site of infection, the conjunctiva, but not in other organs, such as the spleen or blood.35,36 In leishmaniasis, it has been shown that Treg exclusively expand at the site of a primary infection, and that immunity to secondary infections is negatively influenced only at these sites of previous inflammation.37 In our current study, we clearly demonstrate that the Treg response during retroviral infection is also highly compartmentalized, and that Treg expansion is only found in organs with high viral replication and subsequent inflammation. A series of studies suggests that this might also be the case in HIV-infected patients. The first reports on the role of Treg in HIV infection were performed with blood samples from HIV-infected persons. Although these studies demonstrated increased numbers of Treg in the blood of HIV patients compared with uninfected controls, no clear correlation with viral loads and disease progression was found.38,39 However, when lymph nodes, the main reservoir of HIV replication, were analyzed, a correlation between the prevalence of Treg and viral loads, as well as disease progression, was found.40-42 These studies imply that the Treg response is locally restricted in retroviral infections and increases the level of viral replication at sites of inflammation. Our current study using FV-infected Foxp3 DT receptor transgenic mice provides first direct experimental evidence that this concept is correct. This leads to the question for the cells or the factor(s) involved in expansion of Treg and whether recruitment/retention, proliferation, or de novo induction of Treg is the predominant reason for the increased numbers of Treg in virus-infected tissue. Suffia et al showed in a very elegant study that αEβ7 integrin (CD103) is necessary for the retention of Treg at the site of Leishmania major infection.43 In FV-infected mice, nearly all Foxp3+ cells that expand during infection express CD103.12 Thus, it is very likely that this integrin also plays a major role in Treg compartmentalization in FV infection. In addition, we have previously shown that FV-infected DC can expand the population of Foxp3+ cells in vitro upon presentation of antigen to naive T cells.44 Because FV-infected DC were also found in spleens of infected mice,44 it remains possible that virus-infected DC induce the proliferation of Treg at the site of infection. However, our current results show that CD8+ T cells play a vital role in Treg expansion (Figure 3). In FV-infected mice without CD8+ T cells, no expansion of Treg was observed in any of the investigated organs, although viral loads were even higher in FV-infected, CD8+ T cell–depleted mice compared with infected, nondepleted controls.30 These results are in agreement with data from Antunes et al, who showed that suppression of bone marrow pathology in FV-infected mice was mediated by Treg and that the expansion of these Treg exclusively depended on the presence of virus-specific effector CD4+ T cells.31 Thus, the 2 studies indicate that Treg expansion in viral infection is driven by virus-specific effector T cells rather than viral replication itself or presentation of antigens to virus-specific Treg.
It is still a matter of debate whether Treg that suppress pathogen-specific T-cell responses have to be pathogen specific themselves. In several infectious diseases, such as Leishmania9 or hepatitis C virus,45 pathogen-specific Treg have been found. Furthermore, in some autoimmune diseases, only antigen-specific Treg were able to suppress autoreactive T cells, whereas nonspecific Treg were ineffective.46 These reports may imply that only antigen-specific Treg play a significant role in infectious diseases. However, in the current study, we were unable to demonstrate the presence of FV-specific Treg in FV-infected mice using FV-specific class II tetramers or performing adoptive transfer experiments with FV-specific CD4+ T cells from T-cell receptor transgenic mice (data not shown). This is supported by a study from Antunes et al, who used the FV model to show that bone marrow pathology induction by virus-specific, IFNγ-producing CD4+ T cells was efficiently suppressed by virus-nonspecific Treg.31 These data strongly suggest that poly-specific Treg that are efficiently recruited to or proliferate in organs with virus-induced inflammation can suppress virus-specific T-cell responses. Nonspecific proliferation might play a very important role in local expansion of Treg, as Figure 2C shows that in organs of strong virus-induced inflammation, Treg undergo significant proliferation. However, no experimental evidence was found that conversion of Foxp3-negative cells to Treg (supplemental Figure 2) or increased survival of Treg (data not shown) contributed to the expansion of Treg at sites of retroviral infection.
In a very recent study, Lund et al reported their surprising results that ablation of Treg in herpes simplex virus-2–infected mice resulted in an accelerated fatal infection with increased viral loads instead of enhanced immunity to the virus.47 They also used a mouse model in which they could deplete Treg by DT injection. Treg depletion amplified the immune responses in draining lymph nodes at the site of infection, but delayed the entry of the immune cells into the herpes simplex virus–infected tissue. Thus, the authors postulated an immune response–promoting role for Treg in acute infections in which the site of pathogen replication is in nonlymphoid tissues. In contrast to these findings, our current results show for the first time that the suppressive activity of Treg on antiviral immunity seems to be the predominant effect in viral infections in which the primary targets of the virus are cells of the lymphoid organs. This suggests that the biologic effect of Treg in different viral infections can be quite diverse, ranging from a promoting to a suppressing role in antiviral immune responses.
Thus, suppressing Treg responses during infections with lymphotropic viruses might still be an interesting therapeutic approach. We were able to show that this can indeed result in augmented antiviral T-cell responses and superior control of viral replication. Prolonged deletion of Treg has been reported to result in autoimmune diseases in newly born and adult mice,20,48 putting a therapy based on suppressing Treg or their function into question. However, the short-term depletion of Treg that we applied in the current study did not result in severe immunopathology even during an ongoing antiviral immune response. This should encourage researchers to develop new reagents to manipulate Treg in vivo, which may be used for the therapy of infections with lymphotropic viruses.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Markus Simon (Max-Plank-Institut für Immunbiology) for providing the anti–granzyme A antibodies. We are grateful to the National Institutes of Health tetramer facility for providing MHC class II tetramers.
This work was supported by a grant to U.D. and G.Z. from the Deutsche Forschungsgemeinschaft (Di 714/8-2 and TRR60 Project B4).
National Institutes of Health
Authorship
Contribution: G.Z. and K.K.D. designed and performed research, analyzed data, and wrote the paper; Y.P.H. performed research and analyzed data; S.S., S.N., and T.W. performed research; K.G. and O.K. performed research and analyzed data; A.D.G. analyzed data; T.S. provided material and wrote the paper; and U.D. designed research, analyzed data, and wrote the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ulf Dittmer, Institut für Virologie, Universitätsklinikum Essen, Hufelandstrasse 55, 45122 Essen, Germany; e-mail: ulf.dittmer@uni-due.de.
References
Author notes
*G.Z. and K.K.D. contributed equally to this work.