Abstract
Poster Board I-619
Many studies have now demonstrated the prognostic utility of measuring lymphocyte counts before, during and after non-transplant therapy in a wide range of malignancies. In children and young adults with acute lymphoblastic leukemia (ALL), low absolute lymphocyte counts (ALC) during induction chemotherapy are a strong predictor of adverse outcome, however the role of ALC in the era of minimal residual disease (MRD) is not known.
We reviewed 171 pediatric patients with de novo ALL, age 1-21 years, treated at two institutions on the Children's Oncology Group P9900 series of trials from 2000-2006. Variables analyzed included ALC at diagnosis and days 15, 22 and 29 of induction chemotherapy; and other features including age, cytogenetics, WBC, absolute neutrophil count (ANC), platelets, therapeutic regimen, and minimal residual disease (MRD) status at day 29 (MRD-29). ALC at each time-point was evaluated for prognostic ability by univariate and multivariate analysis. Cut-point determined by Martingale residual analysis.
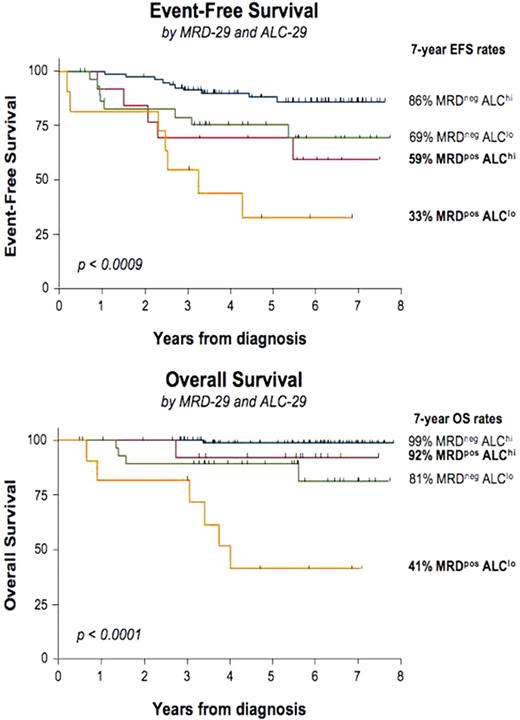
We found high ALC at induction day 29 (ALC-29) to be predictive of improved relapse-free survival (EFS) and overall survival (OS), with a cut-point of 1500 cells/mL demonstrating the greatest predictive power. Patients with ALC-29 > versus <1500 had a 5-year EFS of 83% versus 66% (hazard ratio (HR) 2.2, p=0.018) and a 5-year OS of 96% versus 79% (HR 7.0, p=0.001) respectively. When compared directly to MRD-29 in multivariate analysis, ALC-29 demonstrated independent prognostic significance in EFS (HR 2.4, p=0.017) with striking HR/p-value for OS compared to MRD-29 (HR 10.9 vs. 4.9 and p=0.002 vs. 0.007). Importantly, ALC-29 also remained significant in multi-parameter multivariate analysis which included MRD-29 >0.01%, age >10y, WBC >50k, and favorable/unfavorable cytogenetics (HR 6.8, p=0.022). We found that ALC-29 discriminated subgroups with distinct differences in outcome among patients categorized by MRD-29. Among patients with MRD-29 <0.01%, those with ALC-29 <1500 had an 75/89% EFS/OS while those with ALC-29 >1500 had an excellent EFS/OS of 88/99% (HR 2.7/13.2, p=0.038/0.021). Most strikingly, among patients who were MRD positive (MRD-29 >0.01%), those with ALC-29 <1500 had a dismal EFS/OS of 33/41% versus those with ALC-29 >1500 who had a markedly superior EFS/OS of 69/92% (HR 2.0/9.1, p=0.24/0.041), providing clinically meaningful differences of 36% EFS and 51% OS. At 7 years the combination of ALC-29 and MRD-29 identifies three prognostic groups: a favorable group containing 60% of patients with EFS/OS 86/99% (MRDneg/ALChi), an intermediate group containing 32% of patients with EFS/OS 59-69/81-92% (MRDpos/ALChi and MRDneg/ALClo), and a very poor prognosis group containing 8% of patients with EFS/OS 33/41% (MRDpos/ALClo).
These results suggest that ALC, a simple and readily obtainable test, constitutes a novel and powerful prognostic factor in children and young adults with ALL. ALC has prognostic significance that is independent of MRD and other known risk factors, and may refine MRD-based risk stratification, notably with the ability to identify a subset of MRD-positive patients with a good prognosis. Moreover, the association of higher ALC with improved outcome suggests an important role for host immune surveillance in mediating survival in childhood ALL.
No relevant conflicts of interest to declare.

This icon denotes an abstract that is clinically relevant.
Author notes
Asterisk with author names denotes non-ASH members.