Abstract
Abstract 2906
Poster Board II-882
The World Health Organization (WHO) classification system recognizes indolent SM (ISM) as an entity characterized by low systemic mast cell (MC) burden but frequent skin involvement. The WHO system also recognizes 2 provisional ISM sub-variants: smoldering SM (SSM) and bone marrow (BM) mastocytosis (BMM). The two are respectively characterized by increased systemic MC burden (presence of ≥ 2 ‘B-findings') and BM MC infiltration in the absence of skin or multiorgan visceral lesions. The prognostic relevance of this sub-classification remains unclear.
The study population was drawn from a larger cohort of 342 adult SM patients (Blood. 2009 Jun 4;113(23):5727). Clinical data and BM histology were reviewed, and the diagnosis of ISM and its subclassification confirmed per the 2008 WHO proposal. The primary objectives of the study were to: (i) describe the clinical characteristics of a large cohort of ISM patients, within the context of the WHO classification; (ii) evaluate the prevalence of molecular and cytogenetic abnormalities; (iii) evaluate whether ISM subclassification is prognostically relevant on the basis of survival and risk of transformation to acute leukemia or aggressive SM (ASM).
159 ISM patients were evaluated (69 males; median age 49 years, range 19-84); 22 (14%) had SSM, 36 (23%) BMM, and 101 (63%) ‘ISM-other' (ISMo). By definition, ‘B-findings' were absent in BMM patients. ‘B-findings' in SSM (and ISMo) patients was as follows: hepatosplenomegaly and/or lymphadenopathy 91% (21%), BM MC >30% or serum tryptase level >200ng/mL 68% (8%), and hypercellular BM or dysmyelopoiesis without cytopenias 50% (2%). SSM patients were older (p<0.01) and more frequently displayed constitutional symptoms (p<0.01), and anemia (p<0.01). MC mediator-release symptoms (p=0.01), including anaphylaxis (p<0.01), were more frequent in BMM. The following MC-mediators were studied: serum tryptase (57%), beta prostaglandin F2alpha (45%), urine methylhistamine (32%), and urine histamine (21%) – significant differences were noted amongst the ISM subgroups with the following relationship: SSM>ISMo>BMM (p<0.01).
Complete karyotype information was available for 55 patients; only 1 patient (with ISMo) had an abnormal karyotype. Fifty nine patients were screened for KITD816V and JAK2V617F; JAK2V617F was universally absent, and distribution of KITD816V was not significantly different amongst the ISM subgroups: SSM (100%), BMM (92%), and ISMo (69%).
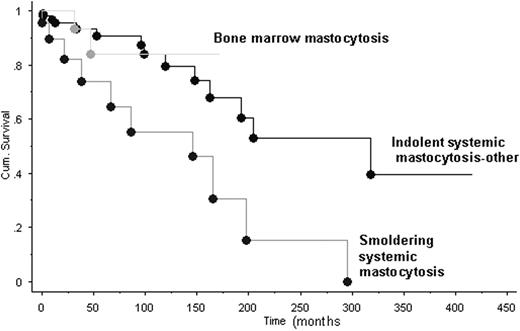
At a median follow of 27 months (range <1-417), 26 deaths were recorded (ISMo 14, SSM 10, and BMM 2), and the combined median survival was 198 months: ISMo 301 months, SSM 120 months, and BMM (not reached) (p<0.01; Figure). Transformation to acute leukemia and ASM was seen in 1 patient (SSM) and 3 patients (2 SSM and 1 ISMo), respectively.
Among WHO-defined ISM patients, SSM is associated with significantly shorter survival whereas BMM and ISMo are prognostically similar. If these observations are confirmed by others, consideration may be given to classifying SSM as a distinct subcategory of SM, instead of a sub-variant of ISM as it currently stands.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.