Abstract
Abstract 3323
Poster Board III-211
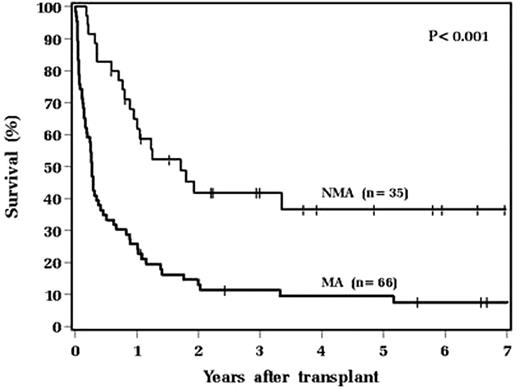
Allogeneic hematopoietic stem cell transplantation (SCT) for patients who have previously undergone allogeneic or autologous SCT is potentially curative, but dangerous. In order to identify patient, disease and treatment characteristics associated with outcome, we analyzed prognostic factors in 101 consecutive patients who underwent second transplants using allogeneic donors at the Cleveland Clinic between May 1987 and October 2008. Inclusion criteria included age ≥ 18, first SCT either autologous or allogeneic, and second SCT allogeneic. The second transplant was myeloablative (MA) in 65.3% of patients and non-myeloablative (NMA) in 34.7%. Relative to NMA second transplants, patients who underwent MA second transplants were younger (median 34 vs. 45 years, P<0.001), were more likely to have undergone autologous first transplant (34.8% vs. 71.4%, P<0.001), and were more likely to have undergone their second transplant for a diagnosis of acute leukemia (56.1% vs. 17.1%, P<0.001). Patients whose second transplant was MA had higher rates of non-relapse mortality (NRM) (63.5% vs. 28.6%, P=0.008) and shorter survival than patients whose second transplant was NMA (median 3.2 vs. 20.5 months, P<.001; figure). Using recursive partitioning analysis, we found that 17 patients transplanted within 3 months of first transplant had higher NRM (hazard ratio [HR] 4.28, P<0.001) and worse survival (HR 3.03, P<0.001) than those transplanted >3 months after first transplant. 16 of these 17 patients underwent MA second transplant. Among all 17 patients transplanted within 3 months of first transplant, 1 year mortality was 91.4% and median survival was 2.3 months. Death was almost exclusively due to non-relapse causes. In multivariable analysis, we found that relative to undergoing second transplant more than 3 months after first transplant, transplant within 3 months of first transplant carried a higher rate of death and NRM (HR 2.97, P=0.001 and HR 4.58, P<0.001, respectively). Relative to NMA second transplant, MA second transplant carried higher risk of death and NRM (HR 3.69, P<0.001 and HR 4.81, P<0.001, respectively). This difference was also significant for patients transplanted more than 3 months after first transplant (HR 2.68, P<0.001 for death, and HR 3.24, P = 0.002 for NRM). Relative to autologous first transplant, having undergone myeloablative allogeneic first transplant was also prognostic for both death and NRM in multivariable analysis (HR 1.95, P = 0.024 and HR, 2.48, P = 0.018, respectively). Age, gender, diagnosis, disease status, and donor relationship were not prognostic for survival or NRM.
Kaplan-Meier estimates of overall survival for patients after MA allogeneic second transplant (thick line) or NMA allogeneic second transplant (thin line).
We conclude that MA transplantation within 3 months of prior SCT carries an unacceptably high rate of NRM and should not be performed. Despite a lower incidence of relapse, MA second transplants were associated with substantially more NRM and significantly worse survival than NMA second transplants.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.