Autologous stem cell transplantation as a platform for multiple myeloma treatment is the standard of care for patients who can safely withstand the procedure. Before novel agents were introduced, one-third to one-half of patients did not achieve partial response at transplantation. Previous medical literature has shown that in this past era, absence of initial response to induction therapy had no impact on progression-free survival and overall survival after high-dose therapy. Lack of response to initial induction did not preclude a good response after stem cell transplantation. With the introduction of novel agents—immunomodulatory drugs and proteasome inhibitors—response rates with initial therapy are now between 70% and 100%. This retrospective study analyzes progression-free survival and overall survival in patients who do not have a partial response (never responded or progressed during continuous therapy) after induction therapy with a regimen that contains thalidomide or lenalidomide. Unlike patients in reports published previously—before immunomodulatory drugs—patients who do not achieve partial remission have a significantly shorter overall survival from transplantation (73.5 vs 30.4 months) and a shorter progression-free survival (22.1 vs 13.1 months; P < .001). Absence of a response to induction therapy with thalidomide or lenalidomide predicts a poorer outcome after high-dose therapy.
MedscapeCME Continuing Medical Education online
This activity has been planned and implemented in accordance with the Essential Areas and policies of the Accreditation Council for Continuing Medical Education (ACCME) through the joint sponsorship of Medscape, LLC and the American Society of Hematology. Medscape, LLC is accredited by the ACCME to provide continuing medical education for physicians. Medscape, LLC designates this educational activity for a maximum of 0.5 AMA PRA Category 1 credits™. Physicians should only claim credit commensurate with the extent of their participation in the activity. All other clinicians completing this activity will be issued a certificate of participation. To participate in this journal CME activity: (1) review the learning objectives and author disclosures; (2) study the education content; (3) take the post-test and/or complete the evaluation at http://cme.medscape.com/journal/blood; and (4) view/print certificate. For CME questions, see page 2560.
Disclosures
Morie A. Gertz is a member of the Millennium Advisory Board, received research support from Genzyme, and received honoraria from Millennium, Easi, Celgene, and Amgen. Shaji Kumar is a member of the Genzyme Advisory Board and has received research support from Celgene, Millennium, Novartis, Bayer, and Genzyme. Martha Q. Lacy participated in clinical trials funded by Celgene, Millennium, and Genzyme. The remaining authors; Editor Cynthia E. Dunbar; and CME questions author Charles P. Vega, University of California, Irvine, CA, declare no competing financial interests.
Learning objectives
Upon completion of this activity, participants will be able to:
Describe best current options for treatment of multiple myeloma
List the factors that are associated with better results on induction therapy
Compare cancer-specific and survival outcomes between patients with and without a good response to induction therapy for multiple myeloma
Introduction
High-dose drug therapy is well established as an appropriate salvage regimen for patients with non-Hodgkin lymphoma but only when they have chemotherapy-sensitive disease at the time of first disease progression.1 Multiple myeloma is distinctly different from non-Hodgkin lymphoma because high-dose therapy and autologous transplantation, which are the preferred therapy for myeloma patients who are able to undergo the procedure, can be administered to patients who do not achieve a response before stem cell collection.2,,–5
The role of induction therapy in patients with multiple myeloma who are slated for high-dose therapy has been unclear. Alkylating agents such as melphalan have been traditionally avoided because of concerns regarding the ability to effectively collect stem cells. An advantage of initial therapy has not translated to improved posttransplantation outcome. Studies have suggested that patients with refractory myeloma do well with transplantation compared with other aggressive forms of chemotherapy.6,–8 In an M. D. Anderson Cancer Center study, 41 patients with refractory disease had high-dose therapy. Among them, 56% had a calculated tumor mass reduction of 75% when transplantation occurred early after resistance was recognized.6 When 50 patients with disease refractory to induction therapy received autologous stem cells after ablative chemotherapy, the overall response rate was 92%, with a complete remission (CR) rate of 20%. There was no significant difference in 1-year progression-free survival (PFS) among patients with disease refractory to induction therapy and those with disease sensitive to induction therapy.9 A Southwest Oncology Group trial of 54 transplant recipients with evaluable disease refractory to induction therapy reported a CR rate of 27% and partial response (PR) rate of 58%.10 Studies have shown similar outcomes among patients with multiple myeloma after high-dose therapy, without regard to whether they achieved a PR before transplantation. In one report, 130 patients who underwent transplantation had a 5-year overall survival independent of response to induction therapy with cyclophosphamide, vincristine, doxorubicin, and methylprednisolone—74% with disease sensitive to induction therapy versus 79% with disease refractory to induction therapy.11
Some experts have suggested that induction treatment may not be required at all if high-dose therapy is planned, because the clinical impact of pretransplantation cytoreduction was minimal. It was also possible to collect stem cells successfully without pretransplantation cytoreduction.12 However, all these data are from the era before the introduction of novel agents. Induction therapies were primarily corticosteroid based, such as doxorubicin, dexamethasone, and vincristine; doxorubicin-methylprednisolone; or the combination of cyclophosphamide, vincristine, doxorubicin, and methylprednisolone. At that time, response rates before transplantation hovered in the 50% range, with few complete responses. Currently, 30% to 60% of patients commonly have a very good partial remission (VGPR) or better after 4 cycles of induction with novel-agent therapy.13,–15 The purpose of this study was to report the outcomes of patients after high-dose therapy, stratified in accordance with whether a patient achieved PR or better after thalidomide- or lenalidomide-based induction therapy.
Methods
The protocol of this study involved patients who received a diagnosis of multiple myeloma between December 1998 and November 2008. To be included in this retrospective analysis, patients could have received no more than one prior therapy, and treatment induction must have contained thalidomide or lenalidomide. The exact number of induction cycles that each patient received before referral is not captured, but our referral base generally administers 4 cycles before referral for high-dose therapy. Patients were grouped into 3 categories. The first category contained patients with a disease response (ie, ≥ 50% decrease in M-protein level) to initial induction therapy. This category was labeled plateau. The second category contained patients who did not have at least a PR (ie, < 50% or a greater decrease in M-protein level with induction therapy); for these patients, the therapy was considered an initial failure and this category was labeled refractory. The third category was composed of patients who had a disease response with more than a 50% reduction in M component and then had a relapse, defined as a rise of M-protein by 25% during the continuation of induction therapy. These patients did not receive a second induction regimen but went immediately to transplantation after progressing during their induction therapy.
At our institution, data pertaining to patients who underwent transplantation are captured prospectively in a database that is updated continuously. No patients were lost to follow-up during the study. All patients gave written informed consent for use of their medical records, and the study was approved by the Mayo Clinic Institutional Review Board in accordance with federal regulations and the Declaration of Helsinki.
Stem cells were collected using 2 separate techniques. The first technique involved granulocyte colony-stimulating factor (G-CSF; 10 μg/kg) administered daily until the completion of collection, with apheresis beginning on day +5 of G-CSF treatment. The second technique was administration of cyclophosphamide (1.5 g/m2 per day) for 2 consecutive days, followed by G-CSF on day +3 of cyclophosphamide treatment and continuing until collection was complete, with apheresis beginning when a white blood cell count of more than 0.5 ×109/L (500/μL) and a peripheral blood CD34 count of more than 10/μL were achieved.
These 3 groups were balanced for chemotherapy plus growth factor mobilization and growth factor alone mobilization; even after it was shown that lenalidomide reduced stem cell yields,16 no statistically increased use of cyclophosphamide mobilization occurred for patients whose induction was lenalidomide based.17 To facilitate stem cell procurement, 83 patients (29%) received cyclophosphamide and 203 patients (71%) received growth factor alone. All patients underwent melphalan-based conditioning, which was generally given on day −2 and day −1 of transplantation, with half the melphalan dose administered each day. PFS was measured as time from transplantation to disease progression or to death if death occurred while the disease was still responding to treatment. Overall survival from transplantation was defined as the time from transplantation to the date of death or last follow-up.
Factors of interest were compared among the patient groups. These factors included age, serum β2-microglobulin level, sex, serum albumin level, number of bone marrow plasma cells, whether cyclophosphamide was used in mobilization, and patient status at transplantation. The χ2 and Fisher exact tests were used to compare differences among the patient groups for nominal variables, and the nonparametric Wilcoxon rank sum test was used for continuous variables. PFS and overall survival from the time of transplantation were evaluated with both Kaplan-Meier analysis and a Cox proportional hazards model. Differences in timed end points between these factors, as well as among the patient groups, were tested for statistical significance with 2-tailed log-rank testing. Multivariable analysis was performed using the Cox proportional hazards model. Data analysis was conducted by the senior author (M.A.G.) and data from the database were freely available to all authors of the paper.
Results
The study population consisted of 286 patients, of whom 159 (56%) were male and the median age was 59 years (Table 1). Tandem transplantation was performed in 45 patients (16%). Except where specified in Table 1, melphalan alone was used for conditioning (94%). There were no significant differences in the demographic characteristics among the 3 groups in terms of sex or presence or absence of myeloma bone disease. The proportions of patients in the 3 groups of thalidomide or lenalidomide induction were determined by available protocols at Mayo Clinic over the study period, as well as decisions made by referring physicians on induction therapy selection. The number of patients receiving bortezomib-based induction was only 18 and was too small to provide meaningful information, and hence their data were not included. The patients who were not in a plateau at the time of transplantation had a significantly greater serum β2-microglobulin value (2.90 vs 2.19 mg/L), labeling index (1% vs 0), and percentage of bone marrow plasma cells (22% vs 6%) at transplantation (Table 2), as would be expected because of the lack of response to induction treatment. In addition, the median time from diagnosis to day 0 of bone marrow transplantation was significantly longer in those patients who were not in plateau (6.8 vs 6.2 months; P = .02). A possible explanation for this longer time to transplantation is that the initial intent of the referring physician was not to consider transplantation but rather to focus on long-term induction with a novel agent and its ongoing use as maintenance. However, when it became clear that these patients were nonresponders to induction therapy, they were referred for stem cell transplantation. Age and serum creatinine level did not differ between the 2 groups.
Unlike in pretransplantation induction before the era of novel agents, most patients responded to induction treatment, and a pretreatment PR was present in 232 (81%). Patients considered primary refractory numbered 29 (10%) and those considered relapse on therapy numbered 25 (9%). Analysis showed that the outcomes for the 2 groups of nonresponders with relapse or refractory disease were essentially identical in PFS. These 2 groups were combined into a single category labeled relapsed-refractory to improve the statistical power of comparisons between baseline characteristics at transplantation and PFS after transplantation. Table 3 gives the response rates for all patients after transplantation. There are significantly higher CR and VGPR rates for patients who before transplantation were in the plateau group (50%) compared with patients in the relapsed-refractory group (22%) (P < .001). If the patients with relapse and refractory disease are combined in a single cohort, the percentages of CR, better than VGPR, better than PR, and no response are 13%, 22%, 79%, and 21%, respectively, compared with the patients in the plateau group, whose respective response rates were 38%, 50%, 96%, and 4% (P < .001).
Survival
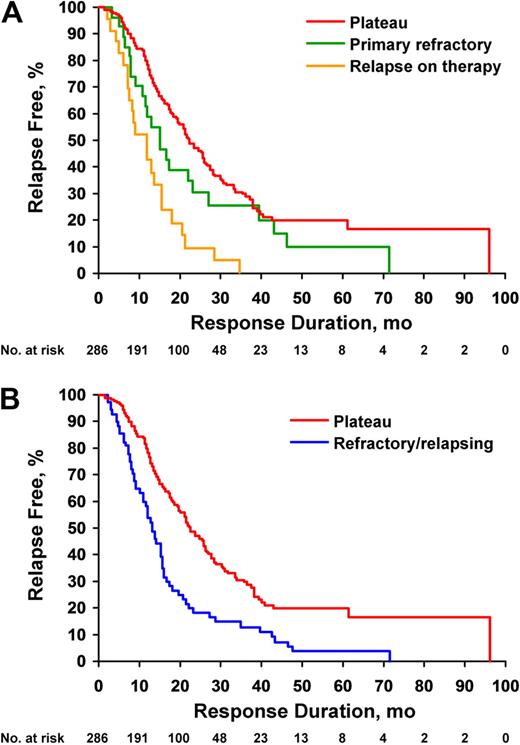
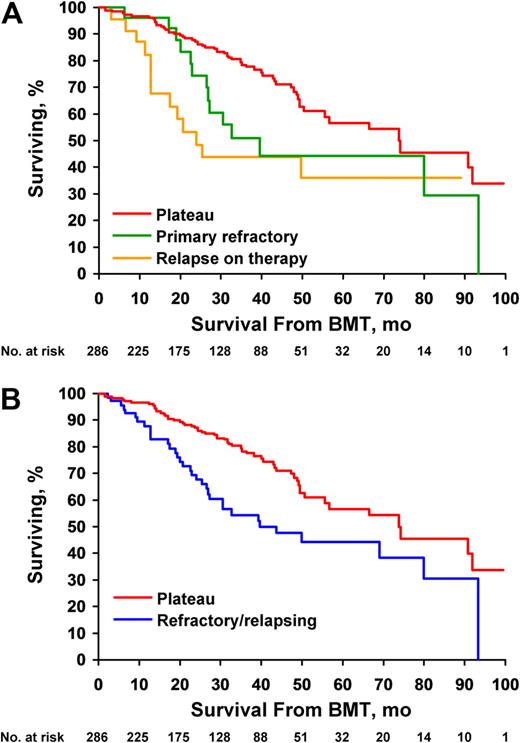
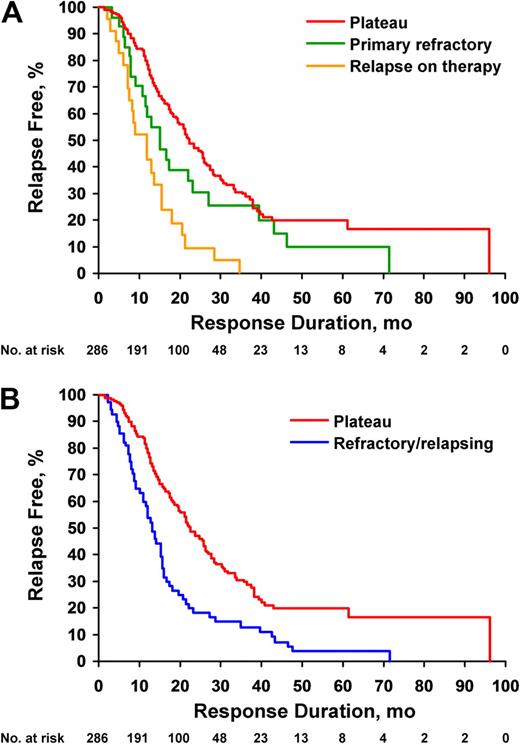
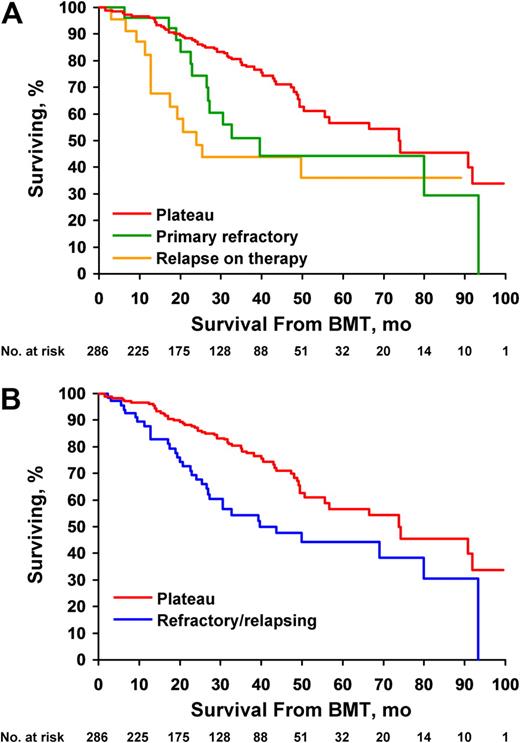
At the time of our analysis, 50% of patients in the relapsed-refractory group had died, compared with 24% in the plateau group. In addition, the multiple myeloma of 83% of the relapsed-refractory group had progressed, compared with 56% of the plateau group. Figure 1A gives the PFS of all 3 groups. The increased length of PFS in the plateau group is statistically significant: 22.1 months versus 15.2 months (95% confidence interval [CI], 9.1-23.3 months), and 12.0 months (95% CI, 7.4-15.4 months) for the primary refractory and relapse on therapy groups, respectively. These latter 2 groups were identical statistically and were combined for the univariable and multivariable analyses of factors that impacted the duration of PFS. Figure 1B shows the PFS from stem cell transplantation collapsing the 2 nonplateau groups, with median PFS of 22.1 versus 13.1 months (P < .001). A statistically significant difference was seen in overall survival when all 3 groups were compared (Figure 2A). A significant difference in survival was seen when all patients with refractory and relapsing disease were combined into a single group (73.5 vs 30.4 months).
Failure to respond to thalidomide or lenalidomide induction leads to shorter posttransplantation progression-free survival (PFS). (A) PFS from day 0 of transplantation, based on response status at transplantation. Medians are 22.1, 15.1, and 12.0 months for plateau (n = 232), refractory (n = 29), and relapse on therapy (n = 25), respectively (P < .001). (B) PFS from day 0 of transplantation, based on response status at transplantation and comparing plateau with refractory and relapsing combined. Medians are 22.1 months for plateau (n = 232) and 13.1 months for refractory or relapsing (n = 54) (P < .001).
Failure to respond to thalidomide or lenalidomide induction leads to shorter posttransplantation progression-free survival (PFS). (A) PFS from day 0 of transplantation, based on response status at transplantation. Medians are 22.1, 15.1, and 12.0 months for plateau (n = 232), refractory (n = 29), and relapse on therapy (n = 25), respectively (P < .001). (B) PFS from day 0 of transplantation, based on response status at transplantation and comparing plateau with refractory and relapsing combined. Medians are 22.1 months for plateau (n = 232) and 13.1 months for refractory or relapsing (n = 54) (P < .001).
Failure to respond to thalidomide or lenalidomide induction leads to shorter posttransplantation overall survival. (A) Overall survival from day 0 of transplantation, based on response status at transplantation. Medians are 73.5, 32.7, and 23.8 months for plateau (n = 232), refractory (n = 29), and relapse on therapy (n = 25), respectively (P < .002). (B) Overall survival from day 0 of transplantation, based on response status at transplantation and comparing plateau with refractory and relapsing combined. Medians are 73.5 months for plateau (n = 232) and 30.4 months for refractory or relapsing (n = 54) (P < .001). BMT indicates bone marrow transplantation.
Failure to respond to thalidomide or lenalidomide induction leads to shorter posttransplantation overall survival. (A) Overall survival from day 0 of transplantation, based on response status at transplantation. Medians are 73.5, 32.7, and 23.8 months for plateau (n = 232), refractory (n = 29), and relapse on therapy (n = 25), respectively (P < .002). (B) Overall survival from day 0 of transplantation, based on response status at transplantation and comparing plateau with refractory and relapsing combined. Medians are 73.5 months for plateau (n = 232) and 30.4 months for refractory or relapsing (n = 54) (P < .001). BMT indicates bone marrow transplantation.
A landmark analysis was performed at 3 months to evaluate differences among patients in plateau and patients with relapse, because response is a time-dependent variable. The survival advantage of early response to novel agents was maintained for 73.7 months versus 32.0 months (P < .001). A landmark analysis was also performed to look at depth of response. Patients achieving VGPR or better had a better overall survival (75% vs 54% at 48 months; P < .001). However, when survival was compared among those patients achieving VGPR or better after transplantation, there was no survival advantage of a pretransplantation response to novel agents (75% vs 73% at 48 months; P = .67). This interesting result is limited by the fact that only 12 patients in the relapsed-refractory group achieved better than VGPR (Table 3) and the number of “failures” was only 3; therefore, reconfirmation with a longer follow-up period is required.
When a univariable statistical analysis was performed of 9 risk factors for PFS (Table 4), serum albumin level, sex, and age were all nonsignificant. A multivariable analysis of the 6 factors significant in the univariable analysis was performed. The patient status at transplantation—plateau versus relapsed-refractory—was significant for PFS (P = .04; hazard ratio, 1.72), as were the labeling index (P < .001; hazard ratio, 1.21) and cytogenetics (P < .02; hazard ratio, 2.0). Cytogenetic abnormalities were present in 39 (14%) of 284 patients tested. Abnormalities of chromosome 13 (either −13 or −13q) were seen in 29; deletion of chromosome 17, in 6; hypodiploidy unrelated to chromosomes 13 and 17, in 1; chromosome 1 abnormalities, in 6; and other complex abnormalities, in 15.
Figure 2B compares overall survival of the 232 patients in the plateau group with the 54 patients in the relapsed-refractory group. When the data of these patients were reanalyzed from the date of diagnosis, the median survival of patients who received the transplant during plateau was 81.8 months compared with those who had refractory disease and relapse on therapy, whose median survival was 47.2 months (P = .01).
Discussion
High-dose melphalan therapy followed by stem cell replacement can overcome drug resistance in myeloma cells.18 A clear-cut survival advantage exists for myeloma patients receiving high-dose therapy compared with conventional therapy.19 However, the nature of the conventional therapy for multiple myeloma has undergone a dramatic change in the past decade20,21 and has moved from being based on corticosteroids to being based on novel agents,22,23 with a reduction in the intensity of the corticosteroids used24 and increased reliance on proteasome inhibition25 and immunomodulatory drugs.26 Previously, the administration of high-dose therapy was performed whether or not a response to induction therapy occurred, with no compromise in PFS or overall survival.27 In one study, those patients achieving a complete response after transplantation had significantly improved overall and event-free survival (P < .01) compared with near-complete responders, who in turn did better than partial responders.28 These outcomes were independent of age. Pretransplantation response was also predictive of overall and event-free survival in complete responders compared with near-complete and partial responders. However, none of these patients received a novel agent at induction after initial diagnosis.
In this study, we evaluated a group of patients who had thalidomide- or lenalidomide-containing induction and were then classified as either responsive, unresponsive, or responsive then relapsed before the administration of high-dose therapy. Previously, no more than 50% of patients achieved a partial response before high-dose therapy; however, with the introduction of immunomodulatory agents (IMiDs), PR rates of 81% were seen in this study and have recently been reported to be as high as 100%.29
The role of stem cell transplantation for patients who never achieve PR or have disease relapse immediately before high-dose therapy is not well defined in the era of novel agents. As expected, patients whose myeloma is unresponsive or who have relapse before transplantation have a greater tumor mass. Our data show that patients with refractory disease and relapse have a median time to progression after transplantation of 12.0 to 15.2 months (Figure 1A); when both groups were combined, the median time to progression was 13.1 months (Figure 1B), which is approximately half the response duration in patients receiving high-dose therapy in the plateau stage. After high-dose therapy, neither group received maintenance therapy after transplantation, and the differences in PFS cannot be attributed to posttransplantation maintenance or consolidation in the induction responsive group. Overall survival was shorter between plateau and refractory and relapsing groups, but this outcome would be expected because if the patient had no response to an IMiD at induction, then the salvage options at relapse are far fewer; as a consequence, a reduced overall survival would be predictable. These poor outcomes highlight the need for better conditioning, effective posttransplantation maintenance regimens, consolidation, and redefinition of ways to use tandem transplantation through either a second autologous therapy or nonmyeloablative allogenic transplantation.
Not inherently obvious is that our data suggest that patients who have induction failures to thalidomide or lenalidomide appear to have inherent biologic characteristics that lead to a more rapid regrowth of the myeloma cell population after high-dose melphalan therapy. If there were no differences between the myeloma cells in induction failures to novel agents and those that achieve a plateau, one would expect the PFS after high-dose therapy to be identical in the 2 groups. The shorter PFS in the induction failure group suggests that patients whose disease does not respond to novel-agent induction not only have drug resistance but also have different growth kinetics and appear to recover and resume immunoglobulin synthesis much sooner than patients who have chemotherapy-sensitive disease before high-dose therapy.
Fortunately, the number of patients in the nonplateau group represents less than a quarter of all our myeloma patients. We had previously reported that the progression-free survival in a corticosteroid-refractory population of patients was 2 years9,30 compared with this paper's 13 months in a novel agent–refractory population of patients. Clearly, the relevance of induction failure is different when induction is corticosteroid based versus IMiD based. Where previously the response to high-dose therapy did not predict the outcome after stem cell transplantation, with the introduction of IMiDs the result has changed, and the evidence in support of stem cell transplantation providing durable benefit in this refractory population is not as strong.
The shorter PFS in the induction failure group does not suggest that stem cell transplantation has no utility because the outcome of these patients in the absence of stem cell transplantation cannot be interpreted; in light of the failure of response to novel-agent therapy, their salvage options are limited and perhaps stem cell transplantation continues to be a treatment of choice because no clear-cut alternatives exist for this poor-risk population. Moreover and as Table 3 indicates, among the patients whose disease was refractory or relapsing before transplantation, 79% (42/53) achieved a PR or better after transplantation, suggesting the valuable salvage role that high-dose therapy provides, albeit with a significantly shortened response duration.
Of 25 patients who had relapse but previously had chemotherapy responsiveness, a response was shown in 22 patients (88%), which reflects the ability of high-dose melphalan to result in tumor cytoreduction when prior chemotherapy sensitivity existed. This is less likely to provide durable benefit (median PFS, 12 months) in those patients who have relapse but have never been exposed to melphalan. High-dose melphalan is capable of overcoming resistance to corticosteroid-based therapy, but its ability to provide durable benefit in a cohort that had thalidomide or lenalidomide induction is much less. This observation suggests that resistance to IMiD therapies is mediated by mechanisms that parallel resistance to high-dose melphalan.
The fact that patients in the relapsed-refractory group had a slightly longer time from diagnosis to transplantation (6.8 vs 6.2 months) suggests potential referral bias in this reported population. The longer time from diagnosis to transplantation in an IMiD-refractory population also suggests that there may be selection for the patients for whom initial intent to treat did not include high-dose therapy but was considered only posthoc when the patients' novel-agent induction failed. This retrospective rather than intent-to-treat analysis has the potential to make the results in a refractory population look poorer. Our data also suggest that disease that fails to respond to novel-agent induction has increased activity kinetically, resulting in more rapid regrowth after cytoreduction with high-dose melphalan. This kinetic difference is suggested by the higher labeling index in the relapsed-refractory group compared with the plateau group and the fact that the labeling index remains a significant predictor of PFS in the multivariable model. On the basis of this report, we hope that other groups will begin to report their results of high-dose therapy after novel-agent induction stratified by induction response.
An Inside Blood analysis of this article appears at the front of this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: M.A.G., S.K., M.Q.L., and S.R.H. analyzed and interpreted data and wrote the paper; A.D. participated in patient accrual, data review, and paper review; D.D. participated in patient accrual and performed critical review of the paper; and F.K.B. and W.J.H. participated in patient accrual.
Conflict-of-interest disclosure: M.A.G. is a member of the Millennium Advisory Board, received research support from Genzyme, and received honoraria from Millennium, Easi, Celgene, and Amgen. S.K. received research support from Celgene, Millennium, Novartis, Bayer, and Genzyme, and is a member of the Genzyme Advisory Board. M.Q.L. participated in clinical trials funded by Celgene, Millennium, and Genzyme. A.D., D.D., S.R.H., F.K.B., and W.J.H. declare no competing financial interests.
Correspondence: Morie A. Gertz, Division of Hematology, Mayo Clinic, 200 First St SW, Rochester, MN 55905; e-mail: gertz.morie@mayo.edu.