Abstract
In humans, interleukin-1β (IL-1β) has been suggested as an essential cytokine for developing IL-17– or IL-17A–producing CD4+ T helper 17 (Th17) cells. However, little is known about the relationship of IL-1 receptor expression and Th17 cell differentiation. We report here the presence of 2 distinct CD4+ T-cell populations with and without expression of IL-1RI that correlates with the capacity to produce IL-17 in naive and memory CD4+ T cells of human peripheral blood. IL-1RI+ memory CD4+ T cells had increased gene expression of IL17, RORC, and IRF4 even before T-cell receptor triggering, indicating that the effect of IL-1β is programmed in these cells via IL-1RI. Although CD4+ T cells from umbilical cord blood did not express IL-1RI, the cytokines IL-7, IL-15, and transforming growth factor-β (TGF-β) up-regulated IL-1RI expression on naive CD4+ T cells, suggesting that IL-1RI+ naive CD4+ T cells develop in periphery. Furthermore, IL-17 production from the cytokine-treated naive CD4+ T cells was induced by IL-1β and this induction was blocked by IL-1R antagonist. These results indicate that human Th17 cell differentiation is regulated via differential expression of IL-1RI, which is controlled by IL-7 and IL-15.
Introduction
Interleukin-17 (IL-17; IL-17A) is a potent proinflammatory cytokine that has an important role in host defense against extracellular microorganisms.1 IL-17 is produced largely by a unique CD4+ T-cell subset called T helper 17 (Th17) cells. Cytokines have critical roles in controlling the development and expansion of Th17 cells.2-5 In humans, IL-1β, a proinflammatory cytokine produced predominantly by macrophages, monocytes, and dendritic cells (DCs), is essential for developing Th17 cells along with IL-6, transforming growth factor-β (TGF-β), and IL-21.6-11 IL-23, which is also produced by innate immune cells, amplifies the Th17 population by promoting IL-21 production from Th17 cells and enhancing their expression of the IL-23 receptor (IL-23R).8,10,12,13 Indeed, human CD4+ T cells expressing the IL-23R produced higher levels of IL-17 compared with CD4+ T cells not expressing this receptor.8 Human Th17 cells can also produce IL-17F, IL-22, and IL-26.8,9,14 Th17 cell development is controlled by transcription factors RORγt (human ortholog is RORC), RORα,15,16 and IRF4.17 It is well known that Th1 and Th2 cells have distinct expression patterns of chemokine receptors. Similarly, Th17 cells have increased expression of CCR4 and CCR6.18
IL-1β is the one of the first-generation cytokines discovered and has pluripotent effects on the immune system.19 IL-1β binds to the receptor complex composed of IL-1 receptor type I (IL-1RI) and IL-1 receptor accessory protein (IL-1RAcP or RIII) (reviewed in Boraschi and Tagliabue20 ). Although IL-1RAcP does not bind to IL-1β directly, binding of IL-1β to the IL-1RI chain leads to recruiting the IL-1RAcP to form a high-affinity receptor complex.21 In addition, IL-1β can bind to IL-1 receptor type II (IL-1RII), which serves as a decoy receptor.22 IL-1β binding to the IL-1RII recruits the IL-1RAcP but forms a nonsignaling complex.23
IL-1 can stimulate T cells that express IL-1 receptors.24,25 T cells can modify their responses to cytokines through regulating the expression of the cytokine receptors. For example, T cells down-regulate the expression of the IL-7 receptor alpha chain that is essential for IL-7–mediated cell survival in response to T-cell receptor (TCR) triggering and IL-7.26 However, little is known about the relationship of IL-1 receptor expression and Th17 cell differentiation, although this cytokine is critically involved in developing Th17 cells in humans.6-8,11 We have addressed this issue. Here we identified 2 distinct subsets of CD4+ T cells with and without expression of IL-1RI (hereafter called IL-1RI+ and IL-1RI− CD4+ T cells, respectively) in naive and memory CD4+ T cells in healthy human peripheral blood. The differential expression of IL-1RI on human CD4+ T cells confers distinct capacities in producing IL-17 and such cytokine receptor expression is dynamically regulated via TCR triggering and cytokines including IL-7, IL-15, and TGF-β.
Methods
Cells and flow cytometry
This work was approved by the institutional review committee of Yale University. Human peripheral blood was obtained from the New York Blood Center or drawn from healthy adult donors after obtaining informed consent in accordance with the Declaration of Helsinki. Mononuclear cells were prepared from peripheral blood or medical waste umbilical cord blood on FicollPAQUE (GE Healthcare) gradients. Cells were stained with antibodies to AmCyan-CD3, Pacific Blue–CD8α, phycoerythrin (PE)–CCR6, PE-CXCR3, PE-CCR4, PE–cyanin 5 (Cy5)–CD45RA, PE-Cy7-CCR7, allophycocyanin (APC)–Cy7– or Alexa Fluor 700–CD4, fluorescein isothiocyanate (FITC)–CD31, FITC- or APC-CD161 (all from BD Biosciences), FITC– or PE–IL-1RI, PE–IL-21R (all from R&D Systems), FITC-CD28, APC-CD27, and APC-Cy7-CD62L (all from eBioscience). Some cells were stained with biotinylated anti–IL-23R antibodies (R&D Systems) and streptavidin–Alexa Fluor 647 (Invitrogen). Cells were analyzed using an LSRII flow cytometer (BD Biosciences) and FlowJo software (TreeStar).
Cell sorting
Peripheral blood mononuclear cells were stained with antibodies to PE–IL-1RI, PE–Cy5-CD45RA, PE–Cy7-CCR7, and APC–Cy7-CD4. Stained cells were sorted into IL-1RI+ and IL-1RI− naive (CD45RA+CCR7+) CD4+ T cells as well as IL-1RI+ and IL-1RI− memory (CD45RA−CCR7+/−) CD4+ T cells using a FACSAria (BD Biosciences). Sorted cells were treated with RPMI 1640 medium (pH 3) supplemented with 10% (vol/vol) fetal calf serum for 30 seconds to strip off anti–IL-1RI antibodies. Cells were then washed with 30 mL of 4°C medium and rested at 37°C overnight.27 The efficacy and effect of the stripping on cell viability were tested by measuring fluorescence in the FL2 channel and staining cells with 7-aminoactinomycin D (supplemental Figure 1, available on the Blood website; see the Supplemental Materials link at the top of the online article).
Cell culture
Sorted cells were cultured in serum-free X-VIVO-15 medium (Lonza) for CD4+ naive T cells or in RPMI 1640 medium supplemented with 10% fetal calf serum for CD4+ memory T cells. Cells were seeded at 2.5 × 104 in U-bottomed 96-well plates and stimulated with beads coated with anti-CD3 and anti-CD28 antibodies (1 bead per 20 cells; Invitrogen). When indicated, IL-1β (25 ng/mL), IL-6 (10 ng/mL), IL-23 (25 ng/mL), TGF-β (5 ng/mL; all from R&D Systems), IL-21 (25 ng/mL; eBioscience), and/or IL-1 receptor antagonist (IL-1Ra, 125 ng/mL; R&D Systems) were added into the culture. Some sorted IL-1RI+ CD4+ memory T cells were incubated for 2 hours with mouse anti–human IL-1RII or mouse IgG2a antibodies (20 μg/mL; both from R&D Systems) and stimulated with anti-CD3/CD28 antibody-coated beads in the presence or absence of lL-1β. In inducing IL-1RI on CD4+ naive T cells, sorted IL-1RI− CD4+ naive CD4+ T cells were incubated for 6 days with different combinations of cytokines (IL-2, IL-7, IL-15, IL-21, IL-1β, IL-6, IL-21, and IL-23; all 25 ng/mL) in the presence or absence of TGF-β (5 ng/mL). When indicated, an inhibitor for AKT (SH-5, 25 μM), Janus kinase 1 (JAK1)/signal transducer and activator of transcription 5 (STAT5; AG-490, 50 μM), phosphoinositide-3 kinase (PI3K; LY294002, 4 μM), mitogen-activated protein kinase 1/2 (MEK1/2; PD980599, 10 μM; all from Calbiochem), or soluble TGF-β receptor type II (5 μg/mL; R&D Systems) was added. In some experiments, cells were harvested on day 6, placed in tissue culture media containing IL-1Ra (125 ng/mL; R&D Systems), and stimulated for an additional 7 days with anti–CD3/CD28 antibody–coated beads in the presence or absence of IL-1β.
ELISA and intracellular staining
Cytokines in culture supernatant were analyzed using an enzyme-linked immunosorbent assay (ELISA) kit (R&D Systems) or a multiplex cytokine assay kit (BioRad). For intracellular staining, cells were stimulated for 4 hours with phorbol myristate acetate (PMA; 50 ng/mL; Sigma-Aldrich) and ionomycin (1 μg/mL; Sigma-Aldrich) in the presence of Golgiplug (BD Biosciences) and stained with antibodies to PE–IL-1RI and/or APC-CD161 when indicated. Cells were fixed, permeabilized, and stained with antibodies to IL-17 (eBioscience) and interferon-γ (IFN-γ; BD Biosciences) followed by analysis on an LSRII.
Quantitative RT-PCR
Total RNA was extracted from cells using TRIzol (Invitrogen) or RNeasy Plus Midi kit (QIAGEN) and cDNA was synthesized. Real-time quantitative reverse-transcription–polymerase chain reaction (RT-PCR) was performed in triplicates on an Mx3005P QPCR system (Stratagene) using the 2× Brilliant SYBR green master mix (Stratagene). Primers were designed using the OligoPerfect Designer (Invitrogen; sequences in supplemental Data) or adopted from previously described primer sequences.9 The levels of gene expression were normalized to the expression of ACTINB. The comparative CT method (ΔΔCT) was used for quantification of gene expression.
Statistical analysis
A paired t test was done to analyze data using SPSS 15.0 (SPSS Inc). P values of less than .05 were considered statistically significant.
Results
Identification of CD4+ T cells with and without IL-1RI expression in human peripheral blood
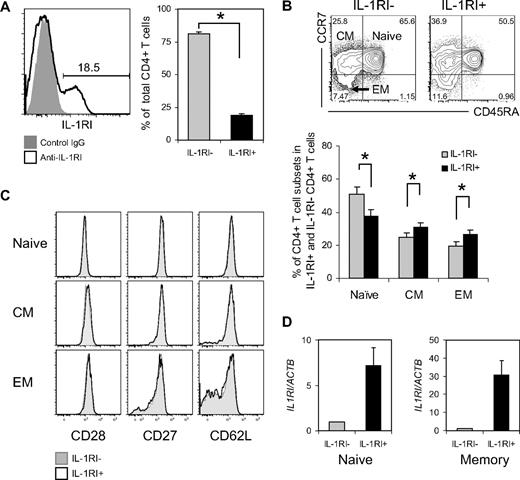
The expression of IL-1 receptors on T cells has been reported in humans and mice.24,25 It is not known, however, whether human CD4+ T cells are uniformly expressing IL-1RI or have distinct cell subsets expressing different levels of IL-1RI. We therefore first measured expression of IL-1RI on human CD4+ T cells in peripheral blood using flow cytometry. Approximately 20% of CD4+ T cells expressed IL-1RI (Figure 1A), indicating the presence of 2 distinct CD4+ T-cell subsets with and without IL-1RI expression. IL-1RI+ and IL-1RI− CD4+ T cells were not homogeneous and could be further subdivided into populations with the phenotypic markers for naive (CD45RA+CCR7+), central memory (CM, CD45RA−CCR7+), and effector memory (EM; CD45RA−CCR7−) CD4+ T cells (Figure 1B). The frequency of cells with the naive phenotype was lower in IL-1RI+ cells than in IL-1RI− cells, whereas the frequency of cells with the CM and EM phenotypes was higher in the IL-1RI+ cells than in the IL-1RI− cells (Figure 1B). We also measured expression of CD27 and CD28, as well as the lymphoid tissue homing molecule CD62L, which are down-regulated upon CD4+ T-cell activation. The 2 cell subsets had similar expression levels of these molecules (Figure 1C). We next measured IL1RI mRNA expression by IL-1RI+ and IL-1RI− CD4+ T cells with the naive (CD45RA+) and memory (CD45RA−CCR7+/−) phenotypes. The mRNA levels of the IL1RI gene were higher in IL-1RI+ cells than in IL-1RI− cells in both naive and memory CD4+ T cells (Figure 1D). The frequency of IL-1RI+ cells was higher in the memory CD4+ T-cell subset than in the naive CD4+ T-cell subset (mean ± SEM, 25.7% ± 2.32% vs 14.9% ± 1.72%, P < .001) although the mean fluorescent intensity (MFI) of IL-1RI in IL-1RI+ cells was similar between the 2 cell subsets (MFI ± SEM, 1790.3 ± 126.73 vs 1800.3 ± 113.66). Our findings indicate that 2 distinct CD4+ T-cell subsets with and without IL-1RI expression are present in human peripheral blood, and such cell subsets have similar cell differentiation phenotypes as measured by cell surface markers.
Ex vivo identification of CD4+ T cells with and without IL-1RI expression in healthy human peripheral blood. (A) Flow cytometric analysis of IL-1RI expression on CD4+ T cells. The number on the histogram plot indicates the frequency (%) of IL-1RI+ cells in total CD4+ T cells. (B) Flow cytometric measurement of the frequency (%) of naive (CD45RA+CCR7+), central memory (CM; CD45RA−CCR7+), and effector memory (EM; CD45RA−CCR7−) cells in IL-1RI+ and IL-1RI− CD4+ T cells. Numbers in quadrants indicate the frequency of cells for each quadrant. (C) Flow cytometry of CD28, CD27, and CD62L expression on IL-1RI+ and IL-1R− naive, CM, and EM CD4+ T cells. (D) RT-PCR analysis of IL1RI expression in sorted IL-1RI+ and IL-1RI− naive and memory (CD45RA−CCR+/−) CD4+ T cells. Results are relative to the level of expression of β-actin. Data represent the mean ± SEM of 15 (A-B) and 5 (D) donors or 8 separate experiments (C, 1 experiment per donor). *P < .05 using the paired t test.
Ex vivo identification of CD4+ T cells with and without IL-1RI expression in healthy human peripheral blood. (A) Flow cytometric analysis of IL-1RI expression on CD4+ T cells. The number on the histogram plot indicates the frequency (%) of IL-1RI+ cells in total CD4+ T cells. (B) Flow cytometric measurement of the frequency (%) of naive (CD45RA+CCR7+), central memory (CM; CD45RA−CCR7+), and effector memory (EM; CD45RA−CCR7−) cells in IL-1RI+ and IL-1RI− CD4+ T cells. Numbers in quadrants indicate the frequency of cells for each quadrant. (C) Flow cytometry of CD28, CD27, and CD62L expression on IL-1RI+ and IL-1R− naive, CM, and EM CD4+ T cells. (D) RT-PCR analysis of IL1RI expression in sorted IL-1RI+ and IL-1RI− naive and memory (CD45RA−CCR+/−) CD4+ T cells. Results are relative to the level of expression of β-actin. Data represent the mean ± SEM of 15 (A-B) and 5 (D) donors or 8 separate experiments (C, 1 experiment per donor). *P < .05 using the paired t test.
IL-1RI+ memory (CD45RA−) CD4+ T cells produce higher levels of IL-17 in response to TCR triggering compared with IL-1RI− memory CD4+ T cells
We next determined whether IL-1RI+ and IL-1RI− CD4+ T cells had different capacities for producing IL-17. We hypothesized that IL-1RI+ CD4+ T cells were cells that had already experienced IL-1β, which is known to promote IL-17 production from CD4+ T cells.6-8,11 IL-1RI+ CD4+ T cells were the predominant producers of IL-17 in peripheral blood cells that were stimulated with PMA/ionomycin (Figure 2A). To further analyze IL-17 production from IL-1RI+ and IL-1RI− memory CD4+ T cells, we sorted CD4+ T cells into IL-1RI+ and IL-1RI− memory (CD45RA−CCR7+/−) CD4+ T-cell subsets, and stimulated them with anti-CD3 and anti-CD28 antibodies. The frequency of IL-17+ and IL-17+IFN-γ+ cells was higher in IL-1RI+ memory cells than in IL-1RI− memory cells (Figure 2B). Similarly, IL-17 levels were higher in tissue culture media from different time points in the former cells than in the latter cells (Figure 2C). The IL-1RI+ memory CD4+ T-cell fraction, however, had a lower frequency of IFN-γ+ cells than the IL-1RI− memory CD4+ T cells (Figure 2B). The IFN-γ levels in tissue culture media, which reflect the total amounts of IFN-γ produced by both IFN-γ+ and IL-17+IFN-γ+ cells were similar between the 2 subsets, as anticipated (supplemental Figure 2). We next measured the gene expression of RORC, RORA, and IRF4 transcription factors controlling IL17 gene expression, as well as other molecules expressed by Th17 cells in IL-1RI+ and IL-1RI− memory CD4+ T cells that were stimulated for 7 days. RORC, RORA, IRF4, IL17F, IL26, and IL23R gene expression levels were all higher in IL-1RI+ cells than in IL-1RI− cells (Figure 2D). The 2 subsets, however, had similar expression levels of IL21, a cytokine produced by Th17 cells.10 This finding can be explained by the absence of IL-23 in our tissue culture system because IL-23 is essential for IL-21 production by Th17 cells.10 To determine whether IL-1RI+ memory CD4+ T cells are committed to produce IL-17 even before TCR triggering, we measured the gene expression of IL17, RORC, and IRF4 in freshly isolated IL-1RI+ and IL-1RI− memory CD4+ T cells. The IL-1RI+ cells had higher expression levels of the 3 genes than the IL-1RI− cells even before TCR stimulation (Figure 3A), suggesting that the effect of IL-1β is programmed in memory CD4+ T cells via expression of IL-1RI. In fact, IL-1RI+ memory CD4+ T cells had higher expression levels of CCR4, CCR6, IL-23R, and CD161 (Figure 3B-D), molecules that were previously reported to be expressed on IL-17–producing human CD4+ T cells,8,18,28 compared with IL-1RI− CD4+ T cells. Taken together, our data demonstrate that IL-1RI+ memory CD4+ T cells in human peripheral blood have the capacity to produce large amounts of IL-17 and other Th17-associated cytokines.
IL-1RI+ memory CD4+ T cells produce higher levels of IL-17 in response to TCR triggering compared with IL-1RI− memory CD4+ T cells. (A) Flow cytometric analysis of IL-1RI expression on IL-17–producing CD4+ T cells. Peripheral blood mononuclear cells were stimulated for 4 hours with PMA and ionomycin (A). Mean fluorescent intensity (MFI) of IL-1RI expression on IL-17+CD4+ (IL-17+) and IL-17−CD4+ (IL-17−) T cells (A, right). (B-C) Sorted IL-1RI+ and IL-1RI− memory CD4+ T cells were stimulated for 7 days (B) or indicated times (C) with anti-CD3/anti-CD28 antibody-coated beads. Cytokine production was determined using intracellular flow cytometry after 4 hours of PMA/ionomycin stimulation (B) or ELISA (C). (D) RT-PCR analysis of Th17-related genes in IL-1RI+ and IL-1RI− memory CD4+ T cells that were treated for 7 days as in panel C. Numbers indicate the frequency of cells for each quadrant (B). Data represent the mean ± SEM of 10 (A), 9 (B), and 5 (C-D) donors. *Below the lower limit of detection (15 pg/mL of IL-17). P values were obtained by the paired t test.
IL-1RI+ memory CD4+ T cells produce higher levels of IL-17 in response to TCR triggering compared with IL-1RI− memory CD4+ T cells. (A) Flow cytometric analysis of IL-1RI expression on IL-17–producing CD4+ T cells. Peripheral blood mononuclear cells were stimulated for 4 hours with PMA and ionomycin (A). Mean fluorescent intensity (MFI) of IL-1RI expression on IL-17+CD4+ (IL-17+) and IL-17−CD4+ (IL-17−) T cells (A, right). (B-C) Sorted IL-1RI+ and IL-1RI− memory CD4+ T cells were stimulated for 7 days (B) or indicated times (C) with anti-CD3/anti-CD28 antibody-coated beads. Cytokine production was determined using intracellular flow cytometry after 4 hours of PMA/ionomycin stimulation (B) or ELISA (C). (D) RT-PCR analysis of Th17-related genes in IL-1RI+ and IL-1RI− memory CD4+ T cells that were treated for 7 days as in panel C. Numbers indicate the frequency of cells for each quadrant (B). Data represent the mean ± SEM of 10 (A), 9 (B), and 5 (C-D) donors. *Below the lower limit of detection (15 pg/mL of IL-17). P values were obtained by the paired t test.
IL-1RI+ memory CD4+ T cells are committed to produce IL-17 even before TCR triggering. (A) RT-PCR analysis of IL17, RORC, and IRF4 expression in sorted and unstimulated (resting) IL-1RI+ and IL-1RI− memory CD4+ T cells. RT-PCR results are relative to the number of transcripts encoding β-actin. Data represent the mean ± SEM of 5 donors. (B-D) Flow cytometric analysis of CCR4, CCR6, IL-23R, IL-21R, and CD161 expression on IL-1RI+ and IL-1RI− memory CD4+ T cells. Representative data from 10 (B-C), or 4 (D) separate experiments (1 experiment per donor).
IL-1RI+ memory CD4+ T cells are committed to produce IL-17 even before TCR triggering. (A) RT-PCR analysis of IL17, RORC, and IRF4 expression in sorted and unstimulated (resting) IL-1RI+ and IL-1RI− memory CD4+ T cells. RT-PCR results are relative to the number of transcripts encoding β-actin. Data represent the mean ± SEM of 5 donors. (B-D) Flow cytometric analysis of CCR4, CCR6, IL-23R, IL-21R, and CD161 expression on IL-1RI+ and IL-1RI− memory CD4+ T cells. Representative data from 10 (B-C), or 4 (D) separate experiments (1 experiment per donor).
IL-1β promotes IL-17 production from both IL-1RI+ and IL-1RI− memory CD4+ T cells
Previous studies reported an essential role for IL-1β in differentiating Th17 cells from naive CD4+ T cells as well as in promoting IL-17 production from memory CD4+ T cells.6-8,11 Thus, we measured IL-17 production from IL-1RI+ and IL-1RI− memory CD4+ T cells after stimulating them with anti-CD3 and anti-CD28 antibodies in the presence of IL-1β. As anticipated IL-1β promoted production of IL-17 from IL-1RI+ memory CD4+ T cells as measured by ELISA (Figure 4A). Of interest, the frequency of IL-17+ cells increased modestly as measured by flow cytometry (Figure 4B), which suggests that IL-1β promotes IL-17 production from precommitted Th17 cells rather than inducing new Th17 cells in the memory CD4+ T-cell population. Surprisingly, IL-1β also increased IL-17 production from IL-1RI− memory CD4+ T cells, and such an effect on the latter cells, as measured by relative change, was greater than on IL-1RI+ memory CD4+ T cells (Figure 4A-B). At day 7 of stimulation, IL-17 production from IL-1RI− memory CD4+ T cells in response to a combination of IL-1β and TCR triggering was approximately 10 times higher than that from the same cells stimulated with TCR triggering alone (Figure 4A), whereas IL-17 production from IL-1RI+ memory CD4+ T cells stimulated with the same combination was only approximately 2-fold higher than that from the same cells stimulated with TCR triggering alone (Figure 4A). However, the total amounts of IL-17 were still much higher in IL-1RI+ cells than in IL-1RI− cells even in the presence of IL-1β (Figure 4A-B). The increased IL-17 production resulting from the addition of IL-1β to TCR triggering was not secondary to increased cell proliferation because IL-β did not enhance proliferation of IL-1RI+ and IL-1RI− memory CD4+ T cells in the presence of TCR triggering (supplemental Figure 3). We also measured potential additive effects of IL-1β and other Th17-polarizing cytokines on IL-17 production from IL-1RI+ memory CD4+ T cells. Although the frequency of IL-17+ cells increased in IL-1RI+ memory CD4+ T cells by the addition of IL-23 to IL-1β and TCR triggering, neither IL-6 nor IL-21 provided additive effects (supplemental Figure 4). TGF-β suppressed the effect of IL-1β (supplemental Figure 4, IL-21 data not shown).
IL-1β promotes IL-17 production from IL-1RI+ and IL-1RI− memory CD4+ T cells. (A) ELISA of IL-17 production from sorted IL-1RI+ and IL-1RI− memory CD4+ T cells that were incubated for 7 days with anti-CD3 and anti-CD28 antibody-coated beads in the presence or absence of IL-1β. (B) Flow cytometric analysis of intracellular IL-17 and IFN-γ in sorted IL-1RI+ and IL-1RI− memory CD4+ T cells that were incubated and stimulated as in panel A followed by 4 hours of PMA and ionomycin stimulation. Numbers in quadrants indicate the frequency of cells for each quadrant. Data represent the mean ± SEM of 5 donors (A) or 7 separate experiments (B, 1 experiment per donor). P values were obtained by the paired t test.
IL-1β promotes IL-17 production from IL-1RI+ and IL-1RI− memory CD4+ T cells. (A) ELISA of IL-17 production from sorted IL-1RI+ and IL-1RI− memory CD4+ T cells that were incubated for 7 days with anti-CD3 and anti-CD28 antibody-coated beads in the presence or absence of IL-1β. (B) Flow cytometric analysis of intracellular IL-17 and IFN-γ in sorted IL-1RI+ and IL-1RI− memory CD4+ T cells that were incubated and stimulated as in panel A followed by 4 hours of PMA and ionomycin stimulation. Numbers in quadrants indicate the frequency of cells for each quadrant. Data represent the mean ± SEM of 5 donors (A) or 7 separate experiments (B, 1 experiment per donor). P values were obtained by the paired t test.
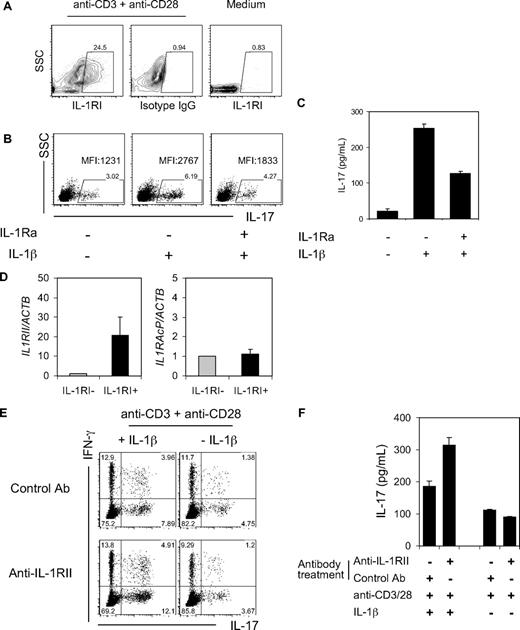
We next explored possible explanations for why IL-1RI− memory CD4+ T cells responded to exogenous IL-1β and how the degree of such a response, as measured by relative changes, was greater in these cells than in IL-1RI+ memory CD4+ T cells (Figure 4A). Given the possibility of IL-1RI up-regulation by TCR triggering, we measured expression of IL-1RI on IL-1RI− memory CD4+ T cells that were stimulated with TCR triggering. Indeed, the stimulated cells had substantial up-regulation of IL-1RI (Figure 5A and supplemental Figure 5), suggesting that the response to IL-1β in IL-1RI− memory CD4+ T cells was likely secondary to TCR-mediated up-regulation of IL-1RI. To further confirm this notion, we first induced IL-1RI expression on IL-1RI− memory CD4+ T cells with TCR triggering and then treated them with IL-1β in the presence or absence of IL-1 receptor antagonist (IL-1Ra). Cells stimulated in the presence of this molecule had reduced IL-17 production (Figure 5B-C).
IL-17 production from memory CD4+ T cells can be modulated by the expression of IL-1RI and IL-RII. (A) Flow cytometric analysis of IL-1RI up-regulation on sorted IL-1RI− memory CD4+ T cells that were incubated for 3 days in the presence or absence of anti-CD3/CD28 antibody-coated beads. (B) Flow cytometric measurement of intracellular IL-17 in sorted IL-1RI− memory CD4+ T cells that were incubated for 2 days with anti-CD3/CD28 antibody-coated beads followed by adding IL-1β and/or IL-1R antagonist (IL-1Ra, 125 ng/mL) and culturing for an additional 5 days. Cells were stimulated for 4 hours with PMA and ionomycin before cytokine analysis. Numbers above boxes in dot plots indicate the frequency of IL-17 cells. MFI indicates the mean fluorescent intensity. (C) ELISA of IL-17 production from sorted IL-1RI− memory CD4+ T cells that were incubated and treated as in panel B except for PMA and ionomycin stimulation. (D) RT-PCR of IL1RII and IL1RACP expression in sorted and unstimulated IL-1RI+ and IL-1RI− memory CD4+ T cells. Results are relative to the number of transcripts encoding β-actin. (E) Sorted IL-1RI+ memory CD4+ T cells were treated for 2 hours with anti–IL-1RII or isotype control antibodies (20 μg/mL) and incubated for 7 days with anti-CD3/CD28 antibody-coated beads in the presence or absence of IL-1β. Intracellular IL-17 and IFN-γ were assessed using flow cytometry after 4 hours of PMA and ionomycin stimulation. Numbers indicate the frequency of cells for each quadrant. (F) ELISA of IL-17 production from sorted IL-1RI+ memory CD4+ T cells that were treated as in panel E. Data represent 5 (A) and 4 (B,E) independent experiments (1 experiment per donor), mean ± SD of triplicates from 4 independent experiments (C,F) or the mean ± SEM of 5 donors (D).
IL-17 production from memory CD4+ T cells can be modulated by the expression of IL-1RI and IL-RII. (A) Flow cytometric analysis of IL-1RI up-regulation on sorted IL-1RI− memory CD4+ T cells that were incubated for 3 days in the presence or absence of anti-CD3/CD28 antibody-coated beads. (B) Flow cytometric measurement of intracellular IL-17 in sorted IL-1RI− memory CD4+ T cells that were incubated for 2 days with anti-CD3/CD28 antibody-coated beads followed by adding IL-1β and/or IL-1R antagonist (IL-1Ra, 125 ng/mL) and culturing for an additional 5 days. Cells were stimulated for 4 hours with PMA and ionomycin before cytokine analysis. Numbers above boxes in dot plots indicate the frequency of IL-17 cells. MFI indicates the mean fluorescent intensity. (C) ELISA of IL-17 production from sorted IL-1RI− memory CD4+ T cells that were incubated and treated as in panel B except for PMA and ionomycin stimulation. (D) RT-PCR of IL1RII and IL1RACP expression in sorted and unstimulated IL-1RI+ and IL-1RI− memory CD4+ T cells. Results are relative to the number of transcripts encoding β-actin. (E) Sorted IL-1RI+ memory CD4+ T cells were treated for 2 hours with anti–IL-1RII or isotype control antibodies (20 μg/mL) and incubated for 7 days with anti-CD3/CD28 antibody-coated beads in the presence or absence of IL-1β. Intracellular IL-17 and IFN-γ were assessed using flow cytometry after 4 hours of PMA and ionomycin stimulation. Numbers indicate the frequency of cells for each quadrant. (F) ELISA of IL-17 production from sorted IL-1RI+ memory CD4+ T cells that were treated as in panel E. Data represent 5 (A) and 4 (B,E) independent experiments (1 experiment per donor), mean ± SD of triplicates from 4 independent experiments (C,F) or the mean ± SEM of 5 donors (D).
To address why IL-17 production was increased only by 2-fold in IL-1RI+ memory CD4+ T cells stimulated with IL-1β whereas it was increased by 10-fold in IL-1RI− memory CD4+ T cells, we measured gene expression of the decoy IL1RII in both subsets of memory CD4+ T cells because the decoy receptor can block the effect of IL-1β.20 The gene expression of IL1RII was higher in IL-1RI+ cells than in IL-1RI− memory CD4+ T cells, although both cell subsets had similar levels of IL1RAcP gene expression (Figure 5D). This finding suggests a role for IL-1RII in limiting the response to IL-1β in IL-1RI+ memory CD4+ T cells. Such a notion was confirmed by measuring IL-17 production from IL-1RI+ memory CD4+ T cells in response to IL-1β and TCR triggering after blocking IL-1RII using anti–IL-1RII antibodies. Indeed, such cells had increased IL-17 production (Figure 5E-F).
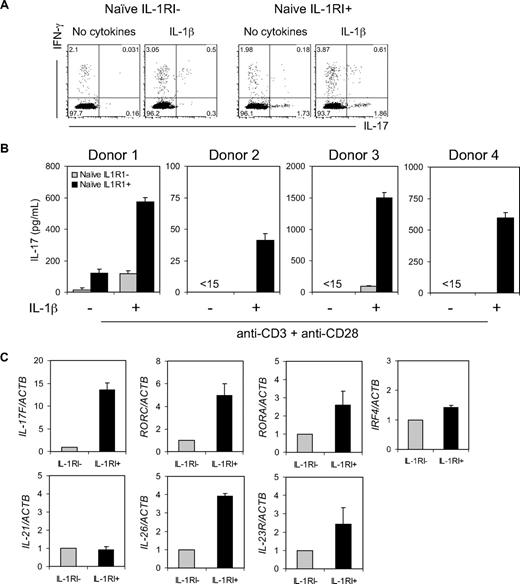
IL-1RI+ naive CD4+ T cells produce higher levels of IL-17 in response to a combination of IL-1β and TCR triggering compared with IL-1RI− naive CD4+ T cells
We could not detect IL-17 production from IL-1RI+ and IL-1RI− naive CD4+ T cells in response to anti-CD3 and anti-CD28 antibodies in any but one tested blood sample (Figure 6A-B). However, adding IL-1β to TCR triggering promoted production of IL-17 from IL-1RI+ naive CD4+ T cells (Figure 6A-B), although the same stimulation failed to induce detectable levels of IL-17 production from IL-1RI− naive CD4+ T cells in most cases (Figure 6B). In line with this finding, IL17F, RORC, RORA, IRF4, IL26, and IL23R gene expression levels were higher in IL-1RI+ cells than in IL-1RI− cells in response to IL-1β and TCR triggering (Figure 6C). However, we could not detect IL17 and RORC gene expression in unstimulated IL-1RI+ and IL-1RI− naive CD4+ T cells (data not shown). Adding a combination of other Th17-polarizing cytokines including IL-23, IL-6, IL-21, and TGF-β to IL-1β further increased production of IL-17 from IL-1RI+ naive CD4+ T cells (supplemental Figure 6). A recent study reported that CD161+CD4+ T cells in human umbilical cord blood had the capacity to differentiate into Th17 cells.28 Thus, we measured expression of CD161 on IL-1RI+ and IL-1RI− naive CD4+ T cells. CD161 expression was hardly found on naive CD4+ T cells regardless of IL-1RI expression (supplemental Figure 7), which is consistent with the results of a previous study.28
IL-1RI+ naive CD4+ T cells produce higher levels of IL-17 in response to a combination of IL-1β and TCR triggering. (A) Flow cytometric analysis of intracellular IL-17 and IFN-γ in sorted IL-1RI+ and IL-1RI− naive CD4+ T cells that were stimulated for 7 days in serum-free media with anti-CD3/anti-CD28 antibody-coated beads in the presence or absence of IL-1β followed by 16 hours of PMA and ionomycin stimulation. (B) ELISA of IL-17 production from sorted IL-1RI+ and IL-RI− naive CD4+ T cells that were stimulated as described in panel A. (C) RT-PCR analysis of Th17-related genes in sorted IL-1RI+ and IL-1RI− naive CD4+ T cells that were stimulated as in panel A. Results are relative to the number of transcripts encoding β-actin. Data represent 4 separate experiments (A, 1 experiment per donor) or are from 4 (B) and 3 (C) donors; error bars, mean ± SD (B) or ± SEM (C) of triplicates.
IL-1RI+ naive CD4+ T cells produce higher levels of IL-17 in response to a combination of IL-1β and TCR triggering. (A) Flow cytometric analysis of intracellular IL-17 and IFN-γ in sorted IL-1RI+ and IL-1RI− naive CD4+ T cells that were stimulated for 7 days in serum-free media with anti-CD3/anti-CD28 antibody-coated beads in the presence or absence of IL-1β followed by 16 hours of PMA and ionomycin stimulation. (B) ELISA of IL-17 production from sorted IL-1RI+ and IL-RI− naive CD4+ T cells that were stimulated as described in panel A. (C) RT-PCR analysis of Th17-related genes in sorted IL-1RI+ and IL-1RI− naive CD4+ T cells that were stimulated as in panel A. Results are relative to the number of transcripts encoding β-actin. Data represent 4 separate experiments (A, 1 experiment per donor) or are from 4 (B) and 3 (C) donors; error bars, mean ± SD (B) or ± SEM (C) of triplicates.
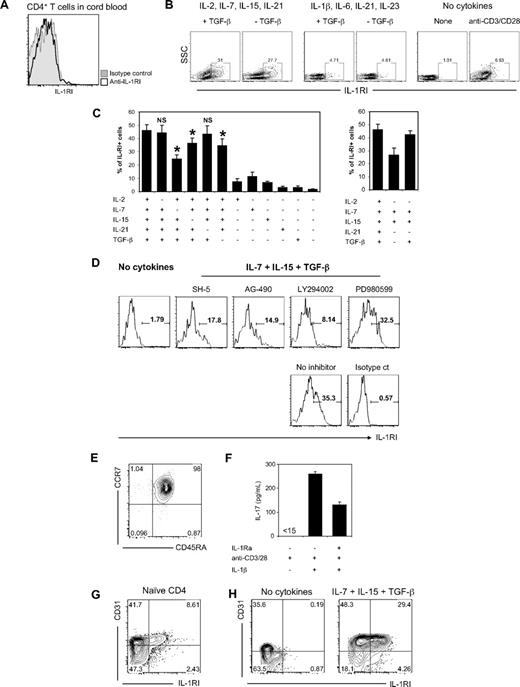
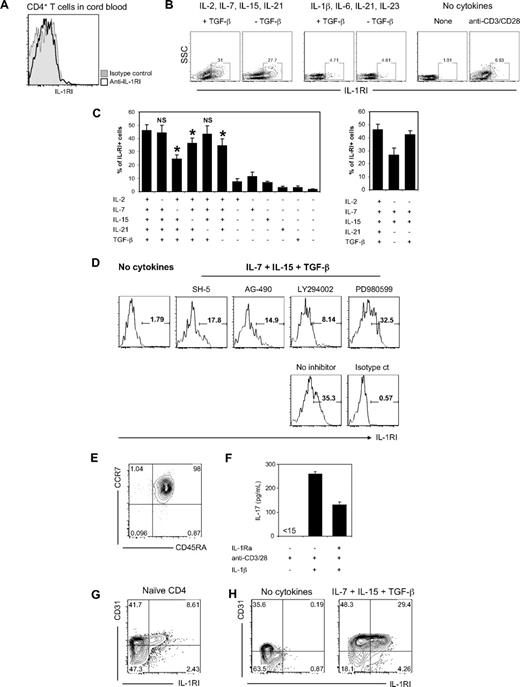
IL-7, IL-15, and TGF-β potently up-regulate IL-1RI on naive CD4+ T cells
We explored a possible mechanism for the existence of IL-1RI+ naive CD4+ T cells in human peripheral blood. First, we measured IL-1RI expression on CD4+ T cells in human umbilical cord blood. No IL-1RI expression was found on these cells (Figure 7A), suggesting that IL-1RI+ CD4+ T cells with the naive phenotype in human peripheral blood are likely generated in the periphery. Hypothesizing that IL-1RI+ naive CD4+ T cells were generated via exposure to a cytokine(s) while maintaining the characteristics of naive cells, we investigated a role for cytokines in up-regulating IL-1RI expression on naive CD4+ T cells. We first determined the effect of 2 cytokine groups: (1) common γ chain (γC) cytokines including IL-2, IL-7, and IL-15 that are involved in T-cell homeostasis29 ; and (2) proinflammatory cytokines including IL-1β, IL-6, and IL-23 that induce Th17 cell differentiation and expansion.3,4 IL-1RI− naive CD4+ T cells were incubated in the presence of cocktails of the cytokines with and without TGF-β, which is essential for Th17 cell differentiation.9-11 IL-21 was also added during the incubations because this γC cytokine is known to promote survival of naive CD4+ T cells30 and enhance IL-17 production from Th17 cells.11 IL-1RI− naive CD4+ T cells that were incubated in the presence of the γC cytokine cocktail had substantial up-regulation of IL-1RI, which was modestly enhanced by adding TGF-β (Figure 7B). However, IL-1RI− naive CD4+ T cells that were incubated in the presence of the proinflammatory cytokine cocktail had minimal up-regulation of IL-1RI, even with the addition of TGF-β (Figure 7B). To further analyze the effect of each cytokine, we removed individual cytokines from the homeostasis cytokine cocktail. The absence of IL-7 significantly reduced up-regulation of IL-1RI on IL-1RI− naive CD4+ T cells even in the presence of other γC cytokines and TGF-β (Figure 7C). Although the removal of IL-15 or TGF-β also reduced the up-regulation of IL-1RI, such reductions were not as large as with the absence of IL-7 (Figure 7C). The removal of IL-2 had no effect on up-regulating IL-1RI. Indeed, a combination of IL-7, IL-15, and TGF-β up-regulated IL-1RI on IL-1RI− naive CD4+ T cells as much as the cocktail of γC cytokines and TGF-β did (Figure 7C). Treatment with IL-7, IL-15, and TGF-β induced cell proliferation in IL-1RI− naive CD4+ T cells. However, such cell proliferation occurred equally in both cell subsets, those up-regulating and not up-regulating IL-1RI (supplemental Figure 8), indicating that the emergence of IL-1RI+ cells in response to these cytokines was not secondary to selective expansion of a small fraction of IL-1RI+ T cells. To block the effect of IL-7 and IL-15, IL-1RI− naive CD4+ T cells were treated with inhibitors for AKT (SH-5), JAK1/STAT5 (AG-490), and PI3K (LY294002) that are involved in the signaling pathways of these cytokines during the culture (Figure 7D). These inhibitors, but not MEK1/2 inhibitor PD980599, reduced the expression of IL-1RI. In addition, TGF-β neutralizing soluble TGF-β receptor II modestly suppressed the expression of IL-1RI (supplemental Figure 9). IL-1RI− naive CD4+ T cells treated with IL-7, IL-15, and TGF-β had no alteration in CD45RA and CCR7 expression (Figure 7E). Of interest, a combination of IL-7, IL-15, and TGF-β also up-regulated IL-1RI expression on IL-1RI− memory CD4+ T cells, although the effect was modest (supplemental Figure 10).
IL-7, IL-15, and TGF-β up-regulate IL-1RI expression on naive CD4+ T cells, leading to enhanced IL-17 production in response to IL-1β and TCR triggering. (A) Flow cytometric analysis of IL-1RI expression on CD4+ T cells in human umbilical cord blood. (B) Flow cytometric analysis of IL-1RI expression on peripheral IL-1RI− naive CD4+ T cells that were incubated for 6 days with the common γ chain cytokine cocktail (IL-2, IL-7, IL-15, IL-21) or IL-17 promoting cytokine cocktail (IL-1β, IL-6, IL-21, IL-23) in the presence or absence of TGF-β as well as with anti-CD3 and anti-CD28 antibody-coated beads. (C) Flow cytometric analysis of the induction of IL-1RI expression on IL-1RI− naive CD4+ T cells that were incubated for 6 days with different combinations of cytokines in the common γ chain cytokine cocktail and TGF-β. The presence and absence of each cytokine are indicated by + and −, respectively. NS indicates not significant; *P < .05, respectively, by paired t test in comparison of cells treated with the common γC cytokine cocktail. (D) Flow cytometric analysis of IL-1RI expression on IL-1RI− naive CD4+ T cells that were treated for 6 days with an inhibitor for AKT (SH-5), JAK1/STAT5 (AG-490), PI3K (LY294002), or MEK1/2 (PD980599) in the presence of IL-7, IL-15, and TGF-β. (E) Flow cytometry of CD45RA and CCR7 expression on IL-1RI− naive CD4+ T cells that were incubated with IL-7, IL-15, and TGF-β as in panel C. (F) ELISA of IL-17 production from sorted IL-1RI− memory CD4+ T cells that were incubated for 6 days with IL-7, IL-15, and TGF-β followed by washing off the cytokines and an additional 7-day stimulation with anti-CD3 and anti-CD28 antibody-coated beads with or without IL-1β in the presence or absence of IL-1R antagonist (IL-1Ra). (G) Flow cytometric analysis of CD31 and IL-1RI expression on naive CD4+ T cells. (H) Flow cytometric analysis of IL-1RI and CD31 expression on IL-1RI− naive CD4+ T cells treated for 6 days with or without IL-7, IL-15, and TGF-β. Data represent 6 (A), 2 (B,D,H) and 4 (E-G) separate experiments (1 experiment per donor) or are from 3 to 5 (C) donors; error bars, mean ± SEM of 3 to 5 experiments (C) or ± SD of triplicates (F). < 15 indicates below the lower limit of detection of IL-17 (15 pg/mL).
IL-7, IL-15, and TGF-β up-regulate IL-1RI expression on naive CD4+ T cells, leading to enhanced IL-17 production in response to IL-1β and TCR triggering. (A) Flow cytometric analysis of IL-1RI expression on CD4+ T cells in human umbilical cord blood. (B) Flow cytometric analysis of IL-1RI expression on peripheral IL-1RI− naive CD4+ T cells that were incubated for 6 days with the common γ chain cytokine cocktail (IL-2, IL-7, IL-15, IL-21) or IL-17 promoting cytokine cocktail (IL-1β, IL-6, IL-21, IL-23) in the presence or absence of TGF-β as well as with anti-CD3 and anti-CD28 antibody-coated beads. (C) Flow cytometric analysis of the induction of IL-1RI expression on IL-1RI− naive CD4+ T cells that were incubated for 6 days with different combinations of cytokines in the common γ chain cytokine cocktail and TGF-β. The presence and absence of each cytokine are indicated by + and −, respectively. NS indicates not significant; *P < .05, respectively, by paired t test in comparison of cells treated with the common γC cytokine cocktail. (D) Flow cytometric analysis of IL-1RI expression on IL-1RI− naive CD4+ T cells that were treated for 6 days with an inhibitor for AKT (SH-5), JAK1/STAT5 (AG-490), PI3K (LY294002), or MEK1/2 (PD980599) in the presence of IL-7, IL-15, and TGF-β. (E) Flow cytometry of CD45RA and CCR7 expression on IL-1RI− naive CD4+ T cells that were incubated with IL-7, IL-15, and TGF-β as in panel C. (F) ELISA of IL-17 production from sorted IL-1RI− memory CD4+ T cells that were incubated for 6 days with IL-7, IL-15, and TGF-β followed by washing off the cytokines and an additional 7-day stimulation with anti-CD3 and anti-CD28 antibody-coated beads with or without IL-1β in the presence or absence of IL-1R antagonist (IL-1Ra). (G) Flow cytometric analysis of CD31 and IL-1RI expression on naive CD4+ T cells. (H) Flow cytometric analysis of IL-1RI and CD31 expression on IL-1RI− naive CD4+ T cells treated for 6 days with or without IL-7, IL-15, and TGF-β. Data represent 6 (A), 2 (B,D,H) and 4 (E-G) separate experiments (1 experiment per donor) or are from 3 to 5 (C) donors; error bars, mean ± SEM of 3 to 5 experiments (C) or ± SD of triplicates (F). < 15 indicates below the lower limit of detection of IL-17 (15 pg/mL).
To determine the biologic significance of cytokine-mediated up-regulation of IL-1RI in vitro, we treated IL-1RI− naive CD4+ T cells with cytokines (IL-7, IL-15, TGF-β) followed by washing off the cytokines and stimulating the cells with IL-1β, anti-CD3, and anti-CD28 antibodies. Indeed, such cells had increased production of IL-17 and this phenomenon was blocked by adding IL-1Ra (Figure 7F) and enhanced by adding IL-23 but not TGF-β (supplemental Figure 11). However, IL-17 production was hardly detected in the same cytokine-treated cells when these cells were stimulated with TCR triggering alone (Figure 7F). In addition, no IL-17 was detected in the same cells in response to IL-1β alone (data not shown). These findings indicate that the cytokine pretreatment enhanced IL-17 production via up-regulating IL-1RI with the subsequent response to IL-1β. Of interest, a recent study reported that human naive CD4+ T cells treated with IL-7 up-regulated the expression of CD31 (platelet endothelial cell adhesion molecule-1), a marker also previously linked to cells recently emigrated from the thymus.31 Thus, we measured CD31 expression on IL-1RI+ and IL-1RI− naive CD4+ T cells to further explore the effect of IL-7 on IL-1RI expression. Indeed, IL-1RI+ naive CD4+ T cells were largely CD31+ cells (Figure 7G). In addition, IL-1RI− naive CD4+ T cells that up-regulated the expression of IL-1RI upon IL-7, IL-15, and TGF-β treatment were mostly CD31+ cells (Figure 7H). Taken together, our findings suggest that IL-1RI+ naive CD4+ T cells are developed through exposure to cytokines including IL-7, IL-15, and TGF-β.
Discussion
Here we have demonstrated the presence of 2 distinct CD4+ T-cell populations with and without IL-1RI expression that have different capacities for producing IL-17 in naive and memory T cells of human peripheral blood. Compared with IL-1RI− memory CD4+ T cells, IL-1RI+ memory CD4+ T cells had higher levels of IL-17 production as well as increased gene expression of IL17F, IL26, IL23R, RORC, RORA, and IRF4 in response to TCR triggering. A combination of TCR triggering and IL-1β, which is known to promote IL-17 expression in CD4+ T cells,6-8,11 augmented IL-17 production from IL-1RI+ memory CD4+ T cells, indicating the biologic significance of the receptor expression. Indeed, IL-1RI+ memory CD4+ T cells that were freshly isolated from peripheral blood had increased gene expression of IL17, RORC, and IRF4 even before TCR triggering, suggesting that the effect of IL-1β is programmed in these memory CD4+ T cells. Of interest, IL-1β also promoted IL-17 production from TCR-stimulated IL-1RI− memory CD4+ T cells. Such a phenomenon was likely secondary to TCR-mediated up-regulation of IL-1RI on IL-1RI− memory CD4+ T cells. Although TCR triggering alone hardly induced production of IL-17 from both IL-1RI+ and IL-1RI− naive CD4+ T cells, adding IL-1β to TCR triggering resulted in substantial production of IL-17 from the former cells but not from the latter cells. It is likely that up-regulation of IL-1RI on naive CD4+ T cells occurs in the periphery because CD4+ T cells from human umbilical cord blood were uniformly negative for IL-1RI. Such up-regulation appears to be mediated at least in part by cytokines including IL-7, IL-15, and TGF-β because these cytokines up-regulated IL-1RI expression on naive CD4+ T cells and IL-17 production from the cytokine-treated cells was induced by IL-1β, which was blocked by IL-1Ra.
Although it is well known that some cytokine receptors are differentially expressed on T cells,26 leading to distinct responses to their cytokines, it was previously unknown whether human CD4+ T cells had homogeneous expression of IL-1 receptors and responded uniformly to IL-1β. The results of our study now show the existence of 2 distinct CD4+ T-cell populations with and without IL-1RI expression. This observation is novel because no studies reported a similar finding using human primary T cells although T cells have been known to express IL-1 receptors for more than 20 years.20 In fact, differential expression of IL-1 receptors on mouse primary T cells or T-cell clones was previously reported, with predominant expression of IL-1 receptors on memory CD4+ T cells and Th2 clones.32,33 However, in our study, both IL-1RI+ and IL-1RI− memory CD4+ T cells produced similar levels of Th2 cytokines (supplemental Figure 12). It is still largely unknown how the IL-1RI and TCR signaling pathways synergize in differentiating Th17 cells. The up-regulation of Th17-associated transcriptional factors RORC, RORA, and IRF4 in IL-1RI+ naive CD4+ T cells in response to IL-1β and TCR triggering as well as in freshly isolated human IL-1RI+ memory CD4+ T cells suggests the possible involvement of such transcription factors in promoting Th17 differentiation by IL-1β and TCR triggering.
Surprisingly, we found IL-1RI+ and IL-1RI− CD4+ T cells in both naive and memory human CD4+ T-cell populations. Although it is arguable that IL-1RI+ naive CD4+ T cells may not be truly naive, they produced almost no or minimal amounts of effector cytokines such as IL-17 and IFN-γ but much higher levels of IL-2 compared with IL-1RI+ memory CD4+ T cells (supplemental Figure 13), which is consistent with the known cellular characteristics of naive and memory T cells. In addition, this finding is supported by similar expression levels of cell differentiation markers including CD28 and CD27 on IL-1RI+ and IL-1RI− naive CD4+ T cells. Of interest, levels of IL-2 produced from IL-1RI− naive CD4+ T cells were approximately twice as high as levels of the same cytokine produced from IL-1RI+ naive CD4+ T cells (mean ± SEM, 13 206.62 ± 1468.08 pg/mL vs 6473.67 ± 1915.59 pg/mL, n = 3 separate donors) although the latter value was still 30-fold higher than the mean of IL-2 levels in IL-1RI+ memory CD4+ T cells (supplemental Figure 13). Based on the results of our studies, including the absence of IL-1RI+ CD4+ T cells in umbilical cord blood, we propose that IL-1RI+ naive CD4+ T cells are generated via exposure to cytokines including IL-7, IL-15, and TGF-β and that such conditioning leads to the up-regulation of IL-1RI on naive CD4+ T cells promoting their differentiation into Th17 cells upon TCR triggering and IL-1β stimulation. Furthermore, our data provide a possible explanation for how TGF-β promotes Th17 differentiation in human naive CD4+ T cells, which could be in part through up-regulating IL-1RI and enhancing the effect of IL-1β. Our findings also provide a scientific rationale for investigating the potential effect of increased levels of IL-7 and IL-15 on Th17 responses in lymphopenic conditions.
Our results indicate that the effect of IL-1β on promoting IL-17 production from CD4+ T cells is dynamically regulated via IL-1 receptors including IL-1RI and IL-1RII. Indeed, we showed that cytokines such as IL-7, IL-15, and TGF-β as well as TCR triggering up-regulated functional IL-1RI expression, which set up CD4+ T cells to produce increased levels of IL-17 in response to subsequent IL-1β stimulation and TCR triggering. This finding is supported by a recent studying reporting IL1RI gene up-regulation in human CD4+ T cells by TCR triggering.34 The effect of IL-1β on IL-17 production from memory CD4+ T cells could be self-regulated by decoy IL-1RII. This receptor binds to IL-1 without transmitting activation signals and we were able to enhance IL-17 production from IL-1RI+ memory CD4+ T cells that expressed IL-1RII by blocking it with neutralizing antibodies.
We speculate that IL-1RI+ memory CD4+ T cells are cells that have seen IL-1β via IL-1RI and been subsequently programmed with IL-1β effect, based on our observations that IL-1RI+ memory CD4+ T cells expressed increased levels of IL17, RORC, and IRF4 genes and IL-23R even before stimulation as well as that IL-17 is rapidly produced by them upon stimulation. Having such a capacity, IL-1RI+ memory CD4+ T cells could be an important type of CD4+ T cell that promptly and efficiently mobilizes innate immune responses against microbial invasions via recruiting neutrophils35 and promoting the synthesis of antimicrobial molecules such as defensins.1 Of interest, the IL-17–producing capacity of IL-1RI+ memory CD4+ T cells, which are already committed to produce IL-17, can be further boosted by IL-1β as seen in our study. This suggests that IL-1RI+ memory CD4+ T cells may serve as a link connecting not only adaptive and innate immunity but also different types of innate immune cells. For instance, microbial infection can stimulate macrophages and DCs to produce IL-1β, which in turn enhances the production of IL-17 from IL-1RI+ memory CD4+ T cells leading to an increase in neutrophil recruitment and expression of antimicrobial molecules. Similar to IL-1RI+ memory CD4+ T cells, IL-1β from macrophages and DCs can enhance IL-17 production from IL-1RI+ naive CD4+ T cells. However, the magnitudes of and time required for IL-17 production from these cells would be much smaller and longer compared to IL-1RI+ memory CD4+ T cells. We recognize that the boosting effect by innate immune cells in promoting IL-17 production from IL-1RI+ memory CD4+ T cells could be also mediated through other cytokines such as IL-23 and IL-6 that enhance Th17 cell response.8,10,13,36 To our knowledge, our study is the first one reporting the existence of 2 distinct CD4+ T cells with and without IL-1RI expression that have different capacities in producing IL-17 in human naive and memory CD4+ T cells. IL-1RI+ CD4+ T cells that are likely developed through TCR triggering as well as exposure to cytokines including IL-7, IL-15, and TGF-β may have a distinct role in human immune responses.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Dr Alexia Belperron for critical review of this paper and Ms Amy Shelton for assisting in the recruitment of human subjects.
This work was supported in part by grants from the National Institutes of Health (AG028069, AG030834, AR049444, AI075157; I.K.). I.K. is a participant of the World Class University Program of the Republic of Korea.
National Institutes of Health
Authorship
Contribution: W.W.-.L., S.W.K., J.C., K.S., and S.-H.L. conducted the experiments; and W.-W.L., E.E.E., R.A.F., and I.K. were involved in designing the research and writing the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Insoo Kang, Department of Internal Medicine, Section of Rheumatology, S525C TAC, 300 Cedar St, New Haven, CT 06520; e-mail: insoo.kang@yale.edu.