Abstract
The bone and immune systems are closely related through cellular and molecular interactions. Because bone-resorbing osteoclasts (OCs) are derived from the monocyte/macrophage lineage, similar to dendritic cells (DCs), we hypothesized that OCs could serve as antigen-presenting cells (APCs) to activate T cells. In this study, OCs were generated from human monocytes with stimulation by receptor activator of nuclear factor κB ligand (RANKL) and macrophage colony-stimulating factor (M-CSF). Results showed that, similar to DCs, OCs express major histocompatibility complex (MHC) classes I and II, and CD80, CD86, and CD40; and uptake soluble antigens. OCs secrete interleukin-10 (IL-10), transforming growth factor-β (TGF-β), IL-6, and tumor necrosis factor-α (TNF-α), but not IL-12p70. OCs present allogeneic antigens and activate both CD4+ and CD8+ alloreactive T cells in an MHC-restricted fashion. OCs also present soluble protein tetanus toxoid to activate autologous CD4+ T cells. These findings indicate that OCs can function as APCs and activate both CD4+ and CD8+ T cells. Thus, our study provides new insight into the effect of OCs on the immune system and may help develop novel strategies for treating diseases such as rheumatoid arthritis and multiple myeloma, which affect both the bone and immune systems.
Introduction
Bone is a dynamic tissue that is constantly being remodeled by bone-resorbing osteoclasts (OCs) and bone-forming osteoblasts.1 Accumulating evidence has indicated that the skeletal and immune systems are closely related through cellular and molecular interactions.2 In the bone marrow (BM), immune cells are derived from the hematopoietic stem cells that interact with bone cells.3 Several regulatory molecules are shared by the immune and skeletal systems, which include cytokines, receptors, signaling molecules, and transcription factors.2,3 For example, receptor activator of nuclear factor κB ligand (RANKL; also known as TNFSF11), which is an essential cytokine for osteoclastogenesis and OC activation, is expressed not only by osteoblasts, but also by activated T cells.4-6 RANKL binding to RANK on OCs induces the trimerization of RANK and tumor necrosis factor (TNF) receptor–associated factor 6, which leads to the activation of nuclear factor κB and mitogen-activated protein kinases, including JUN N-terminal kinase and p38.2 The interaction between the skeletal and immune systems can also be seen in the autoimmune disease rheumatoid arthritis (RA), which is characterized by abnormal and/or prolonged activation of T cells and bone resorption caused by OCs.2 In a commentary article published in Nature, Arron and Choi suggested the term osteoimmunology to describe the interface between bone biology and immunology.7 Now the regulation of OC formation and activity by the immune system has been investigated intensively. RANKL expressed on activated T cells was shown to directly act on OC precursor cells and induce osteoclastogenesis in vitro.8 T cell–derived cytokines such as interferon-γ (IFN-γ), interleukin-4 (IL-4), and IL-10 could inhibit osteoclastogenesis, whereas IL-17, IL-6, and TNF-α could activate osteoclastogenesis.2 However, the effect of OCs on the immune system is still unclear.
OCs, the effector cells for bone resorption, differentiate from hematopoietic monocytic precursors under stimulation of the cytokines RANKL and macrophage colony-stimulating factor (M-CSF).9-11 OC differentiation is associated with activation of genes encoding tartrate-resistant acid phosphatase (TRAP), calcitonin receptor, cathepsin K, β3-integrin, and adenosine triphosphate–dependent proton pump subunits.12 Mature OCs polarize and adhere to bone matrix, induce actin ring formation, acidify bone surface, release osteolytic enzymes, and resorb bone.13 As OCs are differentiated from the same precursor as macrophages and dendritic cells (DCs), which are professional antigen presenting cells (APCs), the potential of OCs to function as APCs was investigated in this study.
APCs are required for priming and initiating antigen-specific T-cell immune responses.14 Professional APCs include DCs, B cells, and macrophages, and nonprofessional APCs include endothelial cells, fibroblasts, epithelial cells, and tumors such as multiple myeloma (MM) cells.15,16 Two generally distinct pathways are used by major histocompatibility complex (MHC) class I and class II molecules for the presentation of peptide antigens to CD8+ and CD4+ T cells, respectively.15 In addition to MHC molecules and antigenic peptides, the costimulatory molecules and cytokines expressed by APCs play pivotal roles in inducing T-cell immunity or tolerance.17,18
In this study, we examined our hypothesis that OCs could serve as APCs to activate T cells. First, we examined the expression of MHC and costimulatory molecules on OCs and the cytokine profile of OCs upon stimulation of lipopolysaccharide (LPS), inflammatory cytokines, or soluble CD40L (sCD40L). Next, we tested the capability of OCs to present alloantigens and activate alloreactive CD4+ and CD8+ T cells, and the ability of OCs to present soluble protein antigen to autologous CD4+ T cells. Our study clearly demonstrated that OCs can serve as APCs to activate both CD4+ and CD8+ T cells, and provides new insight into the immune function of OCs.
Methods
This study was approved by the Institutional Review Board Committee of The University of Texas M. D. Anderson Cancer Center.
Generation and functional assay of osteoclasts
Peripheral blood mononuclear cells (PBMCs) were obtained from buffy coats of healthy volunteers (Gulf Coast Regional Blood Center) by Ficoll-Paque (GE Healthcare) density gradient centrifugation. Isolated PBMCs were allowed to adhere in culture plates for 2 hours in RPMI-1640 (Mediatech Cellgro). Cells were washed 3 times with fresh medium to remove the nonadherent cells. The adherent cells were cultured in OC medium, which was composed of α-minimum essential medium (Gibco) supplemented with 10% fetal bovine serum (Hyclone), antibiotics (Gibco), human RANKL (50 ng/mL; R&D Systems), and human M-CSF (25 ng/mL; R&D Systems) for 14 days. OC medium was changed every 3 days. After 14 days of culture, large numbers of multinucleated OCs were generated. TRAP staining of OCs was performed with Leukocyte Acid Phosphatase kit for TRAP (Sigma-Aldrich) according to the manufacturer's instructions.
The bone resorption assay was performed with dentine discs (Immunodiagnostic Systems). In brief, OCs were induced from monocytes with OC medium in 96-well plate for 14 days with dentine discs in the wells. After washing, dentine discs were fixed with 4% glutaraldehyde (Sigma-Aldrich) in 0.2M sodium cacodylate (Sigma-Aldrich) solution, and stained with 1% toluidine blue (Sigma-Aldrich) in 0.5% sodium tetraborate solution (Sigma-Aldrich). Resorption lacunae, which are blue, were identified with light microscopy (Zeiss).
Generation of dendritic cells and macrophages
Monocyte-derived DCs were generated from PBMCs using a standard protocol.19 In brief, PBMCs were allowed to adhere in culture flasks for 2 hours. The adherent cells were cultured in RPMI-1640 supplemented with 10% fetal bovine serum, antibiotics, granulocyte-macrophage colony-stimulating factor (10 ng/mL; R&D Systems), and IL-4 (10 ng/mL; R&D Systems), with further addition of the cytokines every other day. After 5 days of culture, immature DCs were harvested for use. In some studies, DCs were induced to maturation by addition of LPS (Sigma-Aldrich), IFN-γ (R&D Systems), TNF-α (R&D Systems), and IL-1β (R&D Systems), or sCD40L (R&D Systems).
Macrophages were also generated from PBMCs by suspending in RPMI-1640 and allowing to adhere in culture plates for 2 hours. The adherent cells were cultured in RPMI-1640 supplemented with 10% fetal bovine serum, antibiotics, and M-CSF (10 ng/mL) for 5 days with further addition of cytokines every other day.
Immunophenotyping
OCs cultured in plates were collected by incubation on ice with cold phosphate-buffered saline (PBS) for 10 minutes, followed by digestion with Non-Enzymatic Cell Dissociation Solution (Sigma-Aldrich) for 10 minutes at 37°C. Detached OCs were harvested and resuspended in 3mM ethylenediaminetetraacetic acid/1% bovine serum albumin/PBS buffer. Phycoerythrin (PE)–conjugated or fluorescein isothiocyanate–conjugated monoclonal antibodies (BD Biosciences) against human HLA-ABC, HLA-DR, CD40, CD80, CD86, and CD11c and PE-conjugated monoclonal antibody (eBioscience) against Toll-like receptor 4 (TLR4) were added to cells and incubated for 30 minutes at 4°C. After washing, cells were fixed and analyzed by a flow cytometer (FACSCalibur; BD Biosciences).
ELISA
OCs and DCs were stimulated with LPS (1 μg/mL; Sigma-Aldrich), IFN-γ (50 ng/mL; R&D Systems), TNF-α (10 ng/mL; R&D Systems), and IL-1β (10 ng/mL; R&D Systems), or sCD40L (2 μg/mL; R&D Systems) for 48 hours. Supernatants were collected for measurement of production of IL-12p70, IL-10, transforming growth factor-β1 (TGF-β1), IL-6, IL-1β, and TNF-α using enzyme-linked immunosorbent assay (ELISA) kits (R&D Systems) according to the manufacturer's instructions.
Isolation of monocytes and T cells
CD14+ monocytes and CD3+, CD4+, and CD8+ T cells were isolated from PBMCs with CD14, CD3, CD4, or CD8 magnetic microbeads (Miltenyi Biotec) according to the manufacturer's instructions.
Allogeneic mixed lymphocyte reaction assay
To test for T-cell stimulatory effect of the cells, mixed lymphocyte reaction (MLR) assay was performed. OCs, DCs, macrophages, and 30 Gy–irradiated PBMCs were used as stimulators to 2 × 105 allogeneic PBMCs or purified CD4+ or CD8+ T cells in 96-well flat-bottomed microtiter plates (Corning). Cells were cultured at 37°C in 5% CO2 for 4 to 6 days. Proliferation was determined with the addition of 1 μCi (0.037 MBq)/well of 3H-thymidine (GE Healthcare) 18 hours before harvest. Radioactivity was measured using a β-liquid scintillation analyzer. The results are expressed as the mean number of counts per minute (cpm) of triplicate values.
In some experiments, cultured T cells were labeled with 5(6)-carboxyfluorescein diacetate succinimidyl ester (CFSE; 5μM; Invitrogen) for 10 minutes at 37°C. After washing, labeled T cells were seeded into 96-well flat-bottomed plates and incubated with stimulatory cells for 6 days. Flow cytometry analysis was used to detect the dilution of CFSE.
Analysis of T-cell cytokine production
Purified CD3+ T cells were stimulated with allogeneic OCs or DCs. After 6-day culture, CD4+ T cells were sorted with flow cytometry and restimulated with plate-bound anti-CD3 (OKT3; 5 μg/mL) and anti-CD28 (1 μg/mL) at a concentration of 2 × 106/mL for 24 hours. Supernatants were collected for measuring IFN-γ, IL-10, IL-4, and TGF-β1 concentrations by ELISA kits (R&D Systems).
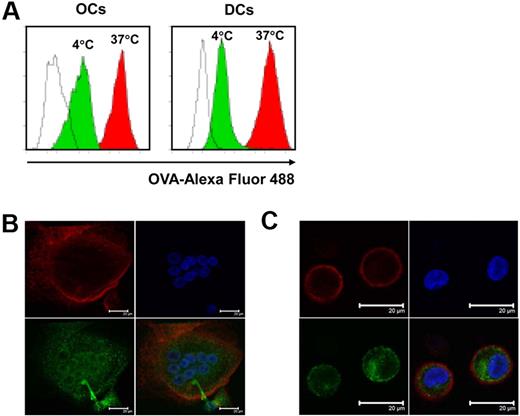
Antigen uptake assay
OCs and immature DCs were incubated with 1 mg/mL ovalbumin (OVA)–Alexa Fluor 488 at 37°C or 4°C for 30 minutes. After incubation, cells were washed with PBS 3 times. OCs were detached with Non-Enzymatic Cell Dissociation Solution (Sigma-Aldrich) before fixation with 4% paraformaldehyde. DCs were fixed directly after washing. The uptake of OVA–Alexa Fluor 488 was analyzed by flow cytometry.
To visualize the antigen uptake with confocal microscope, OCs cultured on the culture slides (BD Bioscience) were incubated with 1 mg/mL OVA–Alexa Fluor 488 at 37°C for 30 minutes. After washing, OCs were stained with PE-conjugated anti-CD11c antibody (BD Bioscience) at 4°C for 20 minutes. Cells were fixed with 4% paraformaldehyde and mounted with DAPI (4′,6 diamidino-2-phenylindole)/Prolong Gold mounting medium (Invitrogen). DCs were treated in the same manner and were cytospun onto glass slides before mounting. Imaging was performed on fixed cells using a Leica SP2 RS laser scanning confocal microscope with an oil immersion objective (633/1.4 numerical aperture).
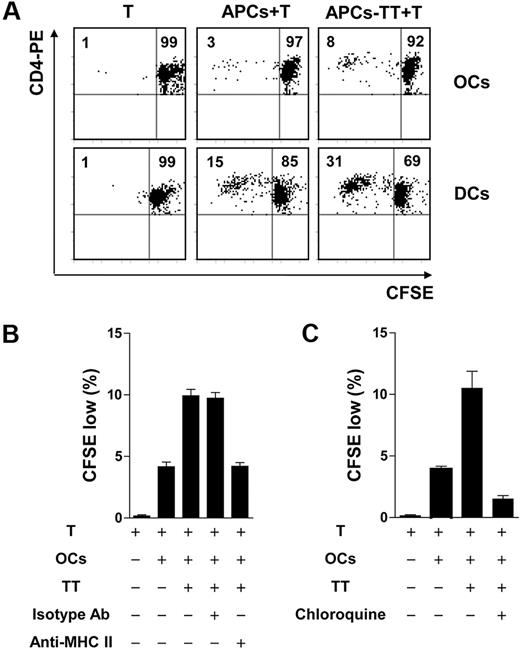
Antigen-presentation assay
To test whether OCs could uptake exogenous soluble antigens and present them to CD4+ T cells, tetanus toxoid (TT)–immunized healthy donors were recruited as we described before.16,20 OCs and immature DCs were pulsed with TT (5 μg/mL) overnight, and DCs were induced to mature with LPS. After washing to remove unbound antigens, cytokines, or LPS, cells were cocultured with autologous purified CD4+ T cells at a T-cell/APC ratio of 20:1. T-cell proliferation was determined on day 6 by CFSE dilution assay as we described previously.19,21
MHC restriction
To study MHC molecules involved in allogeneic MLR and autologous antigen presentation, mouse monoclonal antibodies against HLA-DR (immunoglobulin G2b [IgG2b]; Immunotech), HLA-ABC (IgG2b; W6/32), and a mouse isotypic control IgG2b (Immunotech) were used. The antibodies were added to cell cultures at a final concentration of 10 μg/mL. Results are expressed as the percentage of inhibition compared with cultures without the addition of the antibodies.
Chloroquine treatment
A lysosomotropic agent (chloroquine; Sigma-Aldrich) was used to inhibit antigen processing and presentation. The effect of the drug was evaluated by adding it to cultures containing TT-pulsed OCs and purified autologous T cells, to a final concentration of 50mM.
Results
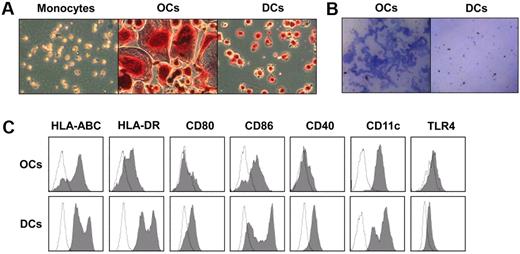
Characterization of OCs
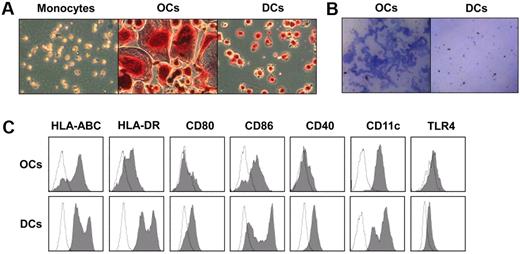
OCs were differentiated in vitro from monocytes of healthy donors in cell culture with the addition of M-CSF and RANKL.22,23 To detect the activity of TRAP in OCs, cultured cells were washed and stained with TRAP kit.24 Because DCs were used as controls in this study and both OCs and DCs were induced from monocytes, we also examined the TRAP activity in monocytes and DCs. Monocytes and immature DCs were cytospun onto glass slides for TRAP staining. As shown in Figure 1A, OCs and immature DCs strongly expressed TRAP, which appeared as purplish to dark red granules in the cytoplasm, whereas only weak TRAP activity could be detected in monocytes. As OCs were formed through the merge of precursors, OCs were much larger than monocytes and DCs, and multiple cell nuclei could be seen in OCs.
Characterization of OCs. Osteoclasts (OCs) were generated from monocytes with macrophage colony-stimulating factor (M-CSF) and receptor activator of nuclear factor κB ligand (RANKL) for 14 days. Dendritic cells (DCs) were derived from monocytes with the addition of granulocyte-macrophage colony-stimulating factor and IL-4 for 5 days. (A) Tartrate-resistant acid phosphatase (TRAP) staining to detect the TRAP activity in monocytes, OCs, and DCs. TRAP activity appears as purplish to dark red granules in the cytoplasm of the cells. (B) Bone resorption assay of OCs and DCs. OCs and DCs were generated from monocytes in 96-well plates with dentine discs in the wells. Dentine discs were stained with toluidine blue, and the blue area indicates the resorption of the dentine. (C) Phenotype of OCs and immature DCs. OCs and DCs were harvested and stained with antibodies and analyzed by flow cytometry. Shown are representative results of 3 independent experiments.
Characterization of OCs. Osteoclasts (OCs) were generated from monocytes with macrophage colony-stimulating factor (M-CSF) and receptor activator of nuclear factor κB ligand (RANKL) for 14 days. Dendritic cells (DCs) were derived from monocytes with the addition of granulocyte-macrophage colony-stimulating factor and IL-4 for 5 days. (A) Tartrate-resistant acid phosphatase (TRAP) staining to detect the TRAP activity in monocytes, OCs, and DCs. TRAP activity appears as purplish to dark red granules in the cytoplasm of the cells. (B) Bone resorption assay of OCs and DCs. OCs and DCs were generated from monocytes in 96-well plates with dentine discs in the wells. Dentine discs were stained with toluidine blue, and the blue area indicates the resorption of the dentine. (C) Phenotype of OCs and immature DCs. OCs and DCs were harvested and stained with antibodies and analyzed by flow cytometry. Shown are representative results of 3 independent experiments.
To examine whether these OCs were capable of bone resorption, OCs were cultured on dentine discs. DCs were used as control. As shown in Figure 1B, the resorbed area of the dentine was stained in blue. OCs were able to resorb dentine, whereas DCs did not. These results show that OCs derived from monocyte were large, TRAP-positive, and multinucleated cells with bone resorption activity.
Phenotype of OCs
To test our hypothesis that OCs could function as APCs to present antigens, we first examined whether OCs express surface molecules important for antigen presentation. To activate T cells, APCs need to express MHC molecules and costimulatory molecules on the cell surface.14,15 MHC class I and class II molecules loaded with antigenic peptides provide the antigen-specific signal to T-cell receptor, whereas molecules such as CD80, CD86, and CD40 mediate the necessary costimulatory signals to T cells. Hence, we detected the expression of these molecules on the surface of OCs by flow cytometric assay. Immature DCs were used as control. As shown in Figure 1C, OCs expressed these molecules, although the percentages of positive cells was lower than that of DCs. Our results showed that both DCs and OCs express CD11c. As TLRs were often expressed on APCs,25 we detected the expression of TLR4 on OCs and DCs (Figure 1C).
Mature DCs have a strong ability to activate T cells through up-regulated expression of MHC molecules and costimulatory molecules.26 DC maturation can be induced by a wide spectrum of factors, including TLR agonists, inflammatory cytokines, and CD40L. To investigate whether these stimulators have a similar effect on OCs, we cultured OCs with LPS (1 μg/mL), IFN-γ (50 ng/mL), TNF-α (10 ng/mL), and IL-1β (10 ng/mL), or sCD40L (2 μg/mL) for 2 days. After the culture, cells were harvested for flow cytometric analysis. Results in Figure 2A show that, whereas TNF-α and IL-1β or sCD40L had little effect, LPS and IFN-γ up-regulated the expression of MHC and costimulatory molecules on OCs. As shown in Figure 2A, all of these stimulators could up-regulate the expression of MHC and costimulatory molecules on DCs. Quantitative expression of these molecules was summarized in Figure 2B. These results clearly show that OCs express MHC and costimulatory molecules that are important for antigen presentation, and the expression of these molecules could be up-regulated by LPS and IFN-γ stimulation.
Phenotypic properties of OCs and DCs.(A) OCs and DCs were cultured with lipopolysaccharide (LPS), interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), and interleukin-1β (IL-1β), or sCD40L for 48 hours. Cells were harvested and stained with antibodies for flow cytometric assay. (B) Summarized data (mean ± SEM) for mean fluorescence intensity (MFI) of cells from 3 different donors are shown.
Phenotypic properties of OCs and DCs.(A) OCs and DCs were cultured with lipopolysaccharide (LPS), interferon-γ (IFN-γ), tumor necrosis factor-α (TNF-α), and interleukin-1β (IL-1β), or sCD40L for 48 hours. Cells were harvested and stained with antibodies for flow cytometric assay. (B) Summarized data (mean ± SEM) for mean fluorescence intensity (MFI) of cells from 3 different donors are shown.
Cytokine profile of OCs
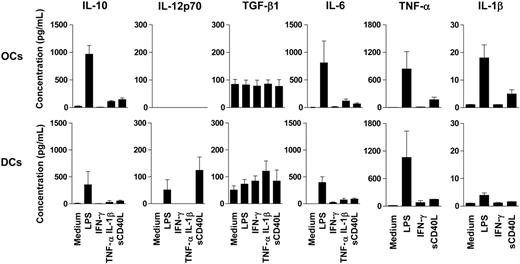
As cytokines secreted by APCs are important for T-cell activation and polarization, we examined cytokine expression by OCs in comparison with DCs with ELISA. OCs and DCs were stimulated with LPS, IFN-γ, TNF-α, and IL-1β, or sCD40L for 48 hours, and supernatants were collected to detect the secretion of cytokines. Results in Figure 3 show that, similar to DCs, OCs secreted IL-10, TGF-β1, TNF-α, IL-6, and IL-1β. However, DCs but not OCs secreted IL-12p70 upon stimulation with LPS or sCD40L, and OCs secreted more IL-10, IL-6, and IL-1β than DCs when stimulated by LPS.
Cytokine profiles of OCs and DCs. Monocyte-derived OCs and DCs were cultured with LPS, IFN-γ, TNF-α, and IL-1β, or sCD40L for 48 hours, supernatants were harvested, and cytokine concentration was measured by ELISA. Shown are summarized data (mean ± SEM) of cytokines from cells from 3 different donors.
Cytokine profiles of OCs and DCs. Monocyte-derived OCs and DCs were cultured with LPS, IFN-γ, TNF-α, and IL-1β, or sCD40L for 48 hours, supernatants were harvested, and cytokine concentration was measured by ELISA. Shown are summarized data (mean ± SEM) of cytokines from cells from 3 different donors.
Stimulatory capacity of OCs
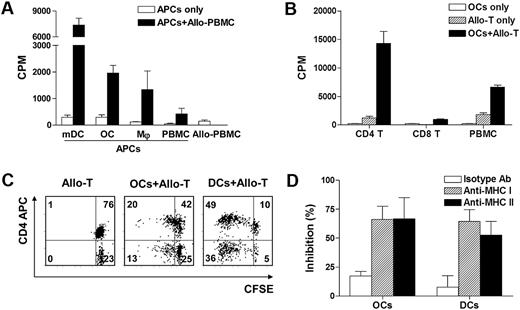
To test our hypothesis that OCs could function as APCs, we performed experiments to examine the ability of OCs to present alloantigens to and activate alloreactive T cells in MLR. Mature DCs, macrophages, and PBMCs from the same donors were used as controls. As OCs and macrophages were adherent cells, they were generated from the same numbers of CD14 magnetic bead–purified monocytes in 96-well flat-bottom plates and cocultured with allogeneic PBMCs as effector T cells. DCs and PBMCs were seeded in wells together with allogeneic PBMCs. Cell proliferation was measured by 3H-thymidine incorporation assay. As shown in Figure 4A, although mature DCs induced the highest allospecific response, OCs were as, if not more, efficient as macrophages at activating alloreactive T cells. These results clearly show that OCs possess the ability of APCs to activate alloreactive T cells.
Capacity of OCs to stimulate alloreactive T cells. (A) Allogeneic peripheral blood mononuclear cells (PBMCs; 2 × 105) were cocultured with 104 LPS-matured DCs (mDCs), OCs, macrophages (Mφ), or PBMCs from the same donors (n = 3), and T-cell proliferation was determined on day 4 with 3H-thymidine assay. (B) OC capacity to activate both CD4+ and CD8+ alloreactive T cells in mixed lymphocyte reaction (MLR) assay. Allogeneic PBMCs or purified CD4+ or CD8+ T cells (2 × 105) were cocultured with 104 OCs, and T-cell proliferation was determined on day 5. Summarized data (mean ± SEM) of cell proliferation (cpm) of cells from 3 different donors are shown. (C) OC capacity to activate both CD4+ and CD8+ alloreactive T cells measured by CFSE dilution assay. CFSE-labeled CD3+ T cells were cocultured with allogeneic OCs and DCs for 5 days. Representative results from 1 of 3 performed experiments are shown. (D) Major histocompatibility complex (MHC) restriction in MLR assay. Antibodies for HLA-ABC or HLA-DR (10 μg/mL) were added to the culture of MLR assay. Isotype IgG was used as control. Shown are percentages of inhibition (mean ± SD) from 3 independent experiments using cells from 3 different blood donors.
Capacity of OCs to stimulate alloreactive T cells. (A) Allogeneic peripheral blood mononuclear cells (PBMCs; 2 × 105) were cocultured with 104 LPS-matured DCs (mDCs), OCs, macrophages (Mφ), or PBMCs from the same donors (n = 3), and T-cell proliferation was determined on day 4 with 3H-thymidine assay. (B) OC capacity to activate both CD4+ and CD8+ alloreactive T cells in mixed lymphocyte reaction (MLR) assay. Allogeneic PBMCs or purified CD4+ or CD8+ T cells (2 × 105) were cocultured with 104 OCs, and T-cell proliferation was determined on day 5. Summarized data (mean ± SEM) of cell proliferation (cpm) of cells from 3 different donors are shown. (C) OC capacity to activate both CD4+ and CD8+ alloreactive T cells measured by CFSE dilution assay. CFSE-labeled CD3+ T cells were cocultured with allogeneic OCs and DCs for 5 days. Representative results from 1 of 3 performed experiments are shown. (D) Major histocompatibility complex (MHC) restriction in MLR assay. Antibodies for HLA-ABC or HLA-DR (10 μg/mL) were added to the culture of MLR assay. Isotype IgG was used as control. Shown are percentages of inhibition (mean ± SD) from 3 independent experiments using cells from 3 different blood donors.
Next we examined whether OCs could activate CD4+ and CD8+ alloreactive T cells, respectively. Effector T cells such as allogeneic PBMCs, purified CD4+ T cells, and CD8+ T cells were cocultured with OCs, and T-cell proliferation was determined by 3H-thymidine incorporation assay. As shown in Figure 4B, OCs induced strong alloreactive T-cell responses in CD4+ and CD3+ (PBMC) populations, whereas CD8+ T-cell activation was also observed but weaker. In addition, purified CD3+ T cells were labeled with CFSE and cocultured with allogeneic OCs, and T-cell proliferation was determined by CFSE dilution assay. As shown in Figure 4C, OCs induced the proliferation of both CD4+ T cells and CD8+ T cells. These results suggest that OCs can both present MHC class I– and class II–restricted alloantigens to and activate CD4+ and CD8+ T cells.
To confirm the results, mouse monoclonal antibodies against human HLA-ABC or HLA-DR were used to inhibit allogeneic MLR. Purified CD3+ T cells were labeled with CFSE and cocultured with allogeneic OCs for 6 days in the presence or absence of 10 μg/mL monoclonal antibodies or isotype control. As shown in Figure 4D, both HLA-ABC and HLA-DR antibodies could inhibit the proliferation of T cells.
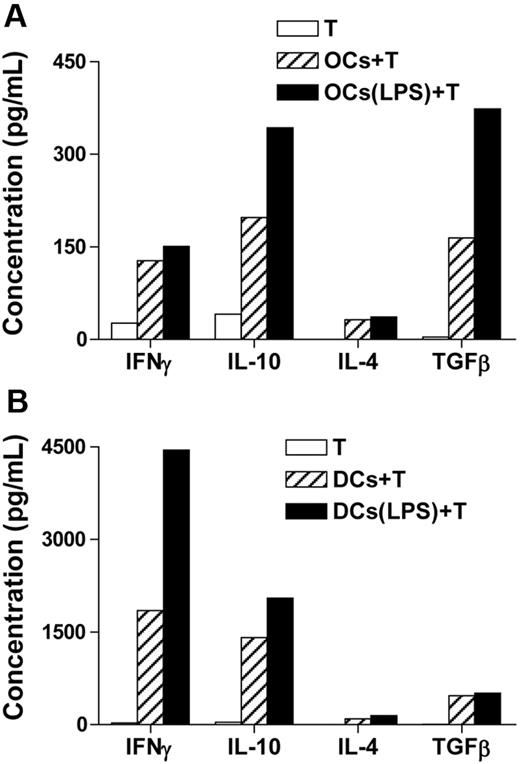
To characterize T-cell cytokine profiles in response to allogeneic OCs or DCs, we sorted out OC-stimulated CD4+ T cells and restimulated them with anti-CD3 and anti-CD28 for 24 hours. Cytokines secreted into supernatants were measured with ELISA. As shown in Figure 5A, CD4+ T cells stimulated by OCs secreted more IL-10 than IFN-γ. LPS-stimulated OCs up-regulated the production of IL-10 and TGF-β1 by the T cells. In contrast, T cells stimulated by DCs secreted more IFN-γ than IL-10, and LPS-matured DCs further up-regulated the secretion of IFN-γ by the T cells (Figure 5B).
Cytokine production of allospecific CD4+ T cells. Purified CD3+ T cells were stimulated with allogeneic OCs or LPS-stimulated OCs for 6 days. DCs were used as control. After the culture, CD4+ T cells were sorted out and restimulated with anti-CD3 and anti-CD28 antibodies for 24 hours. Supernatants were collected and the concentrations of IFN-γ, IL-10, IL-4, and TGF-β1 were measured by ELISA. (A) Production of cytokines by CD4+ T cells stimulated by OCs. (B) Production of cytokines by CD4+ T cells stimulated by DCs. Representative results from 2 independent experiments are shown.
Cytokine production of allospecific CD4+ T cells. Purified CD3+ T cells were stimulated with allogeneic OCs or LPS-stimulated OCs for 6 days. DCs were used as control. After the culture, CD4+ T cells were sorted out and restimulated with anti-CD3 and anti-CD28 antibodies for 24 hours. Supernatants were collected and the concentrations of IFN-γ, IL-10, IL-4, and TGF-β1 were measured by ELISA. (A) Production of cytokines by CD4+ T cells stimulated by OCs. (B) Production of cytokines by CD4+ T cells stimulated by DCs. Representative results from 2 independent experiments are shown.
Antigen uptake assay
Our previous study showed that OCs could uptake MM cells.24 To examine whether OCs could uptake soluble antigen, OVA–Alexa Fluor 488 was incubated with OCs at 37°C for 30 minutes. Incubation of the cells with OVA–Alexa Fluor 488 at 4°C was used as control for surface binding. After incubation and washing, cells were harvested for flow cytometric analysis. As shown in Figure 6A, OCs and immature DCs incubated with OVA–Alexa Fluor 488 at 37°C contained more Alexa Fluor 488 than cells incubated at 4°C, indicating that both DCs and OCs could uptake OVA–Alexa Fluor 488. We also detected the antigen uptake by confocal microscopy. Cells were stained with PE-conjugated anti-CD11c antibody (red), which binds to the surface of OCs and DCs. Nuclei were stained with DAPI (blue). As shown in Figure 6B, OVA–Alexa Fluor 488 (green) could be seen in the cytoplasm of OCs, similar to immature DCs (Figure 6C).
Uptake of soluble antigens by OCs. OCs and immature DCs were incubated with OVA–Alexa Fluor 488 at a concentration of 1 mg/mL at 37°C or 4°C for 30 minutes. After washing and fixation, cells were analyzed by flow cytometry and confocal microscope. (A) Flow cytometric analysis of the uptake of OVA–Alexa Fluor 488 by OCs and DCs. Unfilled curves show cells incubated without OVA–Alexa Fluor 488, green curves show cells incubated with OVA–Alexa Fluor 488 at 4°C, and red curves show cells incubated with OVA–Alexa Fluor 488 at 37°C. Images of (B) OCs or (C) DCs by confocal microscopy. Red shows staining with anti-CD11c antibody, green shows staining with OVA–Alexa Fluor 488, and blue shows nuclei stained with DAPI. Scale bar represents 20 μm. Representative results from 1 of 3 experiments performed are shown.
Uptake of soluble antigens by OCs. OCs and immature DCs were incubated with OVA–Alexa Fluor 488 at a concentration of 1 mg/mL at 37°C or 4°C for 30 minutes. After washing and fixation, cells were analyzed by flow cytometry and confocal microscope. (A) Flow cytometric analysis of the uptake of OVA–Alexa Fluor 488 by OCs and DCs. Unfilled curves show cells incubated without OVA–Alexa Fluor 488, green curves show cells incubated with OVA–Alexa Fluor 488 at 4°C, and red curves show cells incubated with OVA–Alexa Fluor 488 at 37°C. Images of (B) OCs or (C) DCs by confocal microscopy. Red shows staining with anti-CD11c antibody, green shows staining with OVA–Alexa Fluor 488, and blue shows nuclei stained with DAPI. Scale bar represents 20 μm. Representative results from 1 of 3 experiments performed are shown.
Presentation of soluble antigen to autologous T cells
Next, we tested whether OCs could present exogenous soluble antigens to CD4+ T cells. TT-immunized healthy donors were recruited as we have described before.16,20 OCs and immature DCs generated from monocytes of the same donors were pulsed with TT (5 μg/mL) overnight. DCs were induced to mature with addition of LPS to cultures. After removal of unbound antigens, cytokines, or LPS, these cells were cocultured with autologous purified CD4+T cells at a T-cell/APC ratio of 20:1. T-cell proliferation was determined on day 6 by CFSE dilution assay. As shown in Figure 7A, OCs could present TT and induced the proliferation of CD4+T cells, although less efficiently compared with TT-pulsed mature DCs. These results indicate that OCs can uptake exogenous soluble antigens and present them to autologous CD4+ T cells.
Capacity of OCs to present soluble antigen TT to CD4+ T cells and induce T-cell proliferation. (A) Proliferation of tetanus toxoid (TT)–specific T cells induced by TT-pulsed OCs and DCs. CFSE-labeled CD4+ T cells were cultured with autologous OCs or DCs pulsed with TT for 6 days. Flow cytometric analysis was performed to detect the proliferation of CD4+ T cells. Representative results from 1 of 3 experiments performed are shown. (B) MHC restriction in TT-specific CD4+ T-cell response. Antibody (10 μg/mL) for HLA-DR or isotypic control was added to the culture of T cells and TT-pulsed OCs. Data show the proliferation rate of CD4+ T cells detected by CFSE dilution assay. (C) Effect of chloroquine on antigen processing and presentation by OCs. Chloroquine was added at a final concentration of 50 mM to the cell cultures, and T-cell proliferation was detected by CFSE dilution assay. Cultures in panels B and C were run in triplicate and results are expressed as mean ± SD. Representative results from 2 independent experiments are shown.
Capacity of OCs to present soluble antigen TT to CD4+ T cells and induce T-cell proliferation. (A) Proliferation of tetanus toxoid (TT)–specific T cells induced by TT-pulsed OCs and DCs. CFSE-labeled CD4+ T cells were cultured with autologous OCs or DCs pulsed with TT for 6 days. Flow cytometric analysis was performed to detect the proliferation of CD4+ T cells. Representative results from 1 of 3 experiments performed are shown. (B) MHC restriction in TT-specific CD4+ T-cell response. Antibody (10 μg/mL) for HLA-DR or isotypic control was added to the culture of T cells and TT-pulsed OCs. Data show the proliferation rate of CD4+ T cells detected by CFSE dilution assay. (C) Effect of chloroquine on antigen processing and presentation by OCs. Chloroquine was added at a final concentration of 50 mM to the cell cultures, and T-cell proliferation was detected by CFSE dilution assay. Cultures in panels B and C were run in triplicate and results are expressed as mean ± SD. Representative results from 2 independent experiments are shown.
To investigate the MHC restriction of the antigen presentation, monoclonal antibody against HLA-DR was used to inhibit TT-induced T-cell stimulation. The antibody or isotype control (10 μg/mL) was added to the culture of autologous CD4+ T cells and TT-pulsed OCs. As shown in Figure 7B, TT-induced CD4+ T-cell stimulation was inhibited by HLA-DR blocking antibody. No inhibitory effect was seen with isotypic control.
Effect of chloroquine
To confirm that lysosomes were involved in TT presentation on MHC class II molecules of OCs, an inhibitor for lysosomal acidification, chloroquine, was used to treat OCs during TT pulsing and processing. As shown in Figure 7C, TT-induced T-cell stimulation was completely abolished by the presence of chloroquine in the culture.
Discussion
In this study, we described the capacity of OCs to act as APCs. OCs, which were TRAP-positive, multiple nucleated cells with bone resorption ability, were generated from human monocytes with the addition of RANKL and M-CSF. We found that OCs expressed MHC molecules (HLA-ABC and HLA-DR) and signaling or costimulatory molecules (CD80, CD86, and CD40) and that the expression of these molecules could be up-regulated by LPS and IFN-γ. Cytokine assay showed that OCs secreted IL-10, TNF-α, IL-6, TGF-β, and IL-1β, but not IL-12p70. In addition, we found that OCs could induce allogeneic T cells to proliferate and present TT to autologous T cells. These results indicate that, indeed, OCs can act as functional APCs in vitro.
APCs play a pivotal role in cellular immunity by processing and presenting antigens to specific T cells.14 Within the immune synapse formed between APCs and T cells, 3 signals are required for antigen-specific T-cell activation.18 The first signal is provided by antigen peptide–MHC I and peptide–MHC II complexes on the surface of APCs through T-cell receptor to activate CD8+ and CD4+ T cells, respectively. The second signal for T-cell activation involves costimulatory/coinhibitory molecules from B7 family and TNF family.27 CD80 (B7-1) and CD86 (B7-2) provide the best characterized costimulatory signal for T-cell activation through binding to CD28. The third signal for T-cell response is mediated by cytokines. APCs secrete cytokines IL-12, IL-10, TGF-β, IL-6, and IL-23, which direct the differentiation of activated lymphocytes into different effector T-cell subsets.
Our study provides evidence that OCs could act as APCs. Results showed that OCs expressed MHC I and II molecules and costimulatory molecules CD80, CD86, and CD40, and cytokines IL-10, TGF-β, IL-6, and TNF-α, indicating that OCs fulfill the phenotypic and cytokine requirements as APCs. In addition, OCs also functioned as APCs in vitro. OCs were able to induce allogeneic T-cell stimulation, compared with DCs, macrophages, and PBMCs from the same donors. OCs presented the recall antigen TT to autologous T cells and induced T-cell stimulation, which was abolished by the treatment of OCs with the lysosomotropic agent chloroquine.
DCs are the most powerful APCs to prime and activate T cells.28-30 Compared with DCs, the expression levels of HLA-ABC, HLA-DR, and costimulatory molecules on OCs were lower and response to stimuli was different. Both LPS and IFN-γ, but not TNF-α, IL-1β, or CD40L, could up-regulate the expression of these molecules on OCs. OCs secreted higher amounts of IL-10 than DCs upon stimulation with LPS, but OCs did not secrete IL-12p70, suggesting that OCs and DCs may promote different types of T-cell differentiation. In addition, the ability of OCs to activate allogeneic T cells and TT-specific CD4+ T cells was also weaker than that of DCs. The difference between OCs and DCs in phenotype, cytokine expression, and ability to activate CD4+ and CD8+ T cells may indicate that OCs may function differently than DCs in the promotion of T-cell immunity or tolerance. Currently, we are working on the capacity of OCs to regulate the immune responses.
OCs are formed from the fusion of mononuclear precursor cells in the BM.12 BM is not only an important site for hematopoiesis, but is also an important organ for T-cell responses. Feuerer et al have provided convincing evidence to show that BM can be a priming site for T-cell responses to blood-borne antigens that are mediated by resident CD11c+ DCs.31 The responses were not tolerogenic and resulted in generation of cytotoxic T lymphocytes, protective antitumor immunity, and immunologic memory. In addition, BM is also a preferred site for homeostatic proliferation of memory CD8+ T cells.32 In this study, we identified the APC property of human OCs to activate T cells in vitro. Next we will investigate the in vivo effect of OCs on T-cell activation and T-cell function in the BM microenvironment with a mouse model. As reported in a recent study, OCs derived from murine BM cells could cross-present antigen to CD8+ T cells.33
It is well known that T cell–derived cytokines can regulate the generation of OCs.2 For example, IFN-γ inhibits RANKL-induced OC differentiation by accelerating the degradation of tumor necrosis factor receptor–associated factor-6 through activation of the ubiquitin/proteasome system.6,7 The inhibitory effect of IL-10 on RANKL-stimulated osteoclastogenesis is associated with decreases in nuclear factor of activated T cells c1 expression and reduced translocation of this transcription factor into the nucleus as well as suppressed c-Fox and c-Jun expression.34,35 In this study, we found that OCs stimulated T cells to secrete more IL-10 than IFN-γ, which may provide new insight in the effect of OCs on T cells and T cell–mediated immune response.
In conclusion, our study provides direct evidence that OCs could act as APCs and stimulate both CD4+ and CD8+ T cells in vitro. OCs and DCs are different in the expression levels of MHC and costimulatory molecules, cytokine profiles, and the ability to activate T cells. In human diseases with bone loss complication, such as RA,36 and MM,19 T-cell immune responses are responsible for the autoimmunity-mediated tissue damage and for the protective antitumor effect. As increased OC formation and activity occur in RA37 and MM,38 our study on the effect of OCs on T cells will be helpful not only in understanding the mechanism of these diseases, but also in developing new strategies to treat diseases involving both the bone and immune systems.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Ms Alison Woo for providing editorial assistance, and Dr Tomasz Zal and Ms Anna Zal for the technical support with confocal microscopy.
This work was supported by institutional start-up funds from the University of Texas M. D. Anderson Cancer Center, the Center for Targeted Therapy of The University of Texas M. D. Anderson Cancer Center, grants from the National Cancer Institute (R01 CA96569, R01 CA103978, and R01 CA138402), the Leukemia & Lymphoma Society, the Multiple Myeloma Research Foundation, and the Commonwealth Foundation for Cancer Research.
National Institutes of Health
Authorship
Contribution: H.L. performed the majority of experiments and statistical analyses and wrote the paper; S.H. and J.Q. performed some experiments; J.Y. and Y.Z. provided critical suggestions to this study; and Q.Y. contributed to the conceptual idea and experimental design of the paper and to the writing and editing of the paper.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Qing Yi, Department of Lymphoma and Myeloma, The University of Texas M. D. Anderson Cancer Center, 1515 Holcombe Blvd, Unit 0903, Houston, TX 77030; e-mail: qyi@mdanderson.org.