Abstract
Abstract 218
Graft-versus-leukemia (GVL) effects are closely associated with graft-versus-host disease (GVHD) after allogeneic hematopoietic cell transplantation (HCT). In a reexamination of GVL effects, we evaluated acute and chronic GVHD defined by NIH consensus criteria and immunosuppressive treatment (IST) as risk factors for recurrent malignancy after HCT.
We analyzed a cohort of 2656 consecutive patients with acute myeloid leukemia (AML), acute lymphoblastic leukemia (ALL), chronic myeloid leukemia (CML), myelodysplastic syndrome (MDS) or myeloproliferative neoplasms (MPN) who received allogeneic HCT after high-intensity conditioning between 1992 and 2005. The onset of NIH chronic GVHD was ascertained by retrospective chart review using follow-up information obtained by our Long Term Follow Up clinic. Rates and hazards of recurrent malignancy and mortality were analyzed according to GVHD and IST as time-varying covariates. To illustrate the effect of time-varying covariates, we calculated the rate of recurrent malignancy per patient-year according to prior GVHD within sequential 90-day intervals after HCT. Cox proportional hazard models were adjusted for potential factors affecting outcomes.
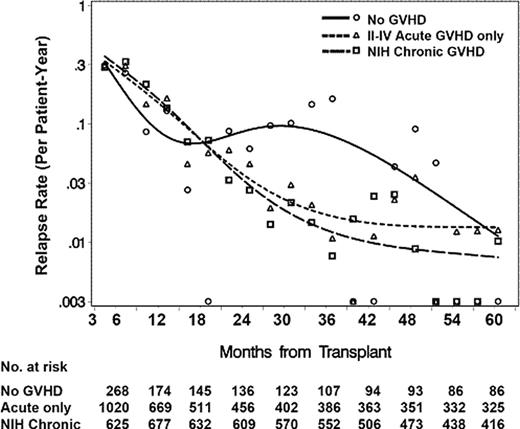
The median patient age at HCT was 39 years (range, 0 to 71 years). Donors were HLA-identical relatives (n=1088), HLA-matched unrelated volunteers (n=912), HLA-mismatched relatives (n=243), and HLA-mismatched unrelated volunteers (n=413). GVHD prophylaxis was mostly cyclosporine and methotrexate (n=1885, 71%). Relapse rates per patient-year declined from 3 months until at least 36 months after HCT for patients with prior acute GVHD or NIH chronic GVHD (Figure). Patients without prior GVHD showed a much less pronounced decline between 12 and 30 months after HCT. Adjusted Cox analysis showed that acute GVHD and NIH chronic GVHD were associated with statistically similar reductions in risk of late recurrent malignancy beyond 18 months after HCT, with no incremental effect of chronic GVHD in patients with prior acute GVHD (Table 1). GVL effects were demonstrable in patients with CML or AML but not in those with ALL or MDS/MPN. Discontinuation of IST was associated with a decreased risk of recurrent malignancy among patients without prior GVHD but not among those with prior GVHD (Table 2). Grades III–IV acute GVHD and NIH chronic GVHD with prior acute GVHD were associated with a statistically significant increase in risk of early mortality between 3 and 18 months, but grade II acute GVHD and NIH chronic GVHD without prior acute GVHD were not.
Risk of recurrent malignancy according to GVHD state
| State . | Early recurrent malignancy (3-18 mos) . | Late recurrent malignancy (>18 mos) . | |||||
|---|---|---|---|---|---|---|---|
| Acute GVHD . | NIH chronic GVHD . | HR1 . | 95% CI . | P . | HR1 . | 95% CI . | P . |
| None | Absent | 1.00 | – | – | 1.00 | – | – |
| Grade II | Absent | 0.90 | 0.66–1.24 | .53 | 0.45 | 0.28–0.72 | .001 |
| Grades III–IV | Absent | 0.76 | 0.50–1.15 | .19 | 0.28 | 0.12–0.64 | .003 |
| None | Present | 0.99 | 0.59–1.66 | .96 | 0.29 | 0.13-0.63 | .002 |
| Grades II–IV | Present | 0.93 | 0.66–1.32 | .70 | 0.30 | 0.18–0.48 | <.0001 |
| State . | Early recurrent malignancy (3-18 mos) . | Late recurrent malignancy (>18 mos) . | |||||
|---|---|---|---|---|---|---|---|
| Acute GVHD . | NIH chronic GVHD . | HR1 . | 95% CI . | P . | HR1 . | 95% CI . | P . |
| None | Absent | 1.00 | – | – | 1.00 | – | – |
| Grade II | Absent | 0.90 | 0.66–1.24 | .53 | 0.45 | 0.28–0.72 | .001 |
| Grades III–IV | Absent | 0.76 | 0.50–1.15 | .19 | 0.28 | 0.12–0.64 | .003 |
| None | Present | 0.99 | 0.59–1.66 | .96 | 0.29 | 0.13-0.63 | .002 |
| Grades II–IV | Present | 0.93 | 0.66–1.32 | .70 | 0.30 | 0.18–0.48 | <.0001 |
Adjusted for disease, risk category, and total body irradiation.
Risk of recurrent malignancy according to GVHD state and immunosuppressive treatment (IST) state
| State . | Early recurrent malignancy (3-18 mos) . | Late recurrent malignancy (>18 mos) . | |||||
|---|---|---|---|---|---|---|---|
| Any GVHD . | IST . | HR1 . | 95% CI . | P . | HR1 . | 95% CI . | P . |
| Absent | Continuing | 1.00 | – | – | – | – | – |
| Absent | Discontinued | 0.35 | 0.18–0.68 | .002 | 1.00 | – | – |
| Present | Continuing2 | 0.64 | 0.45–0.91 | .01 | 0.35 | 0.21–0.57 | <.0001 |
| Present | Discontinued2 | 0.47 | 0.29–0.75 | .002 | 0.34 | 0.21–0.54 | <.0001 |
| State . | Early recurrent malignancy (3-18 mos) . | Late recurrent malignancy (>18 mos) . | |||||
|---|---|---|---|---|---|---|---|
| Any GVHD . | IST . | HR1 . | 95% CI . | P . | HR1 . | 95% CI . | P . |
| Absent | Continuing | 1.00 | – | – | – | – | – |
| Absent | Discontinued | 0.35 | 0.18–0.68 | .002 | 1.00 | – | – |
| Present | Continuing2 | 0.64 | 0.45–0.91 | .01 | 0.35 | 0.21–0.57 | <.0001 |
| Present | Discontinued2 | 0.47 | 0.29–0.75 | .002 | 0.34 | 0.21–0.54 | <.0001 |
Adjusted for disease, risk category, and total body irradiation.
Direct comparison between these 2 states showed no statistically difference in both the early and late phase.
Rates of recurrent malignancy according to GVHD state and time interval from transplantation
Rates of recurrent malignancy according to GVHD state and time interval from transplantation
Both acute and NIH chronic GVHD are associated with potent GVL effects, but NIH chronic GVHD does not confer any incremental benefit after acute GVHD. Withdrawal of IST was associated with a reduction in risk of recurrent malignancy in patients without prior GVHD. Analyses of GVL effects should account for time from HCT, the history of GVHD, type of malignancy and IST. Immune manipulations such as prophylactic donor lymphocyte infusion or early withdrawal of IST may represent reasonable approaches to decrease the risk of recurrent malignancy in patients without prior GVHD, if the risk of GVHD could be minimized.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.