Abstract
Abstract 222
There is growing evidence that geographic proximity to health care affects utilization and outcomes. Access to centers offering allogeneic hematopoietic stem cell transplantation (HSCT) may be challenging for patients living in geographically distant areas, which could potentially result in worse outcomes. Previous studies were limited by small sample sizes and limited geographic analyses. We therefore examined whether geographic proximity to transplant center affected transplantation outcome in a large cohort of patients who underwent allogeneic HSCT at Dana-Farber/Brigham and Women's Cancer Center (DF/BWCC).
We analyzed all adult patients who underwent allogeneic HSCT at DF/BWCC between 1996 and 2009 and who resided within 6 hours driving time of the institution. Driving time from primary residence to DF/BWCC based on zipcode was determined using geographic information systems (ArcGIS 9, ESRI, Redlands CA, USA).
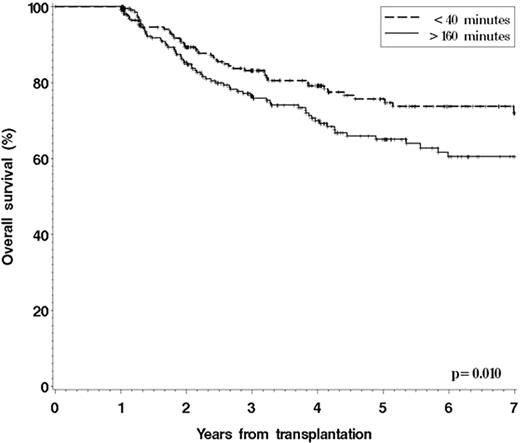
Of 2414 patients who underwent allogeneic HSCT at DF/BWCC during the study period, 2008 met our inclusion criteria. The median age (range) was 47 (17-73) years; 55% underwent HSCT for acute leukemia/myelodysplasia, 24% for lymphoma and 13% for chronic myelogenous leukemia. Sixty two percent received myeloablative conditioning; 45% were transplanted from a matched related donor; 63% received peripheral blood stem cells. The median driving time (range) to DF/BWCC was 72 (2-358) minutes. Although overall survival (OS) was not statistically different between patients when divided by driving time in quartiles (p=0.21), the survival curves appeared to diverge after 1 year. In a landmark analysis of 940 patients alive and free of disease at 1 year, 5-yr OS was 76% and 65% for patients in the bottom (<40 minutes) and top (>160 minutes) quartiles of driving time to DF/BWCC, respectively (p=0.010) (Figure 1). In a multivariable model of patients alive and disease free at one year (including covariates for age, gender, race, median household income, zipcode of residence, performance status at HSCT, disease, stage at HSCT, conditioning intensity, donor type, graft source, gender match, CMV serostatus, GVHD prophylaxis and year of HSCT), patients in the top quartile had a higher risk of death than those in the bottom quartile (hazard ratio (HR) 1.71; p=0.006). Similarly, the HR for relapse or death was 1.49; p=0.021. Based on competing risks multivariable regression analyses, this difference was mostly due to an increase in non-relapse mortality.
Kaplan-Meier OS for patients alive and disease free at one year after allogeneic HSCT according to driving time from primary residence to DF/BWCC
Kaplan-Meier OS for patients alive and disease free at one year after allogeneic HSCT according to driving time from primary residence to DF/BWCC
In patients alive and disease-free one year after allogeneic HSCT, increased driving time from primary residence to transplantation center was associated with a significant decrease in post-HSCT survival. This suggests that continued close follow-up and supportive care at the transplantation center may be important in optimizing the outcome of transplantation, even beyond 1 year. This could have simple but far-reaching implications for the post-transplant management of patients who do not live within close range of their transplant center.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.