Abstract
Abstract 371
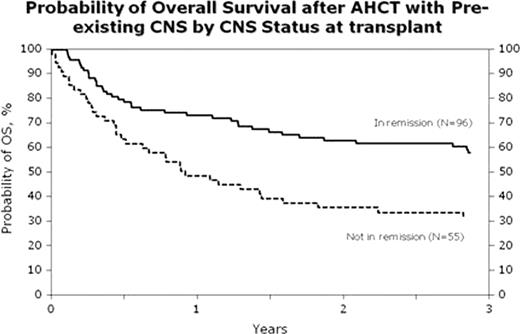
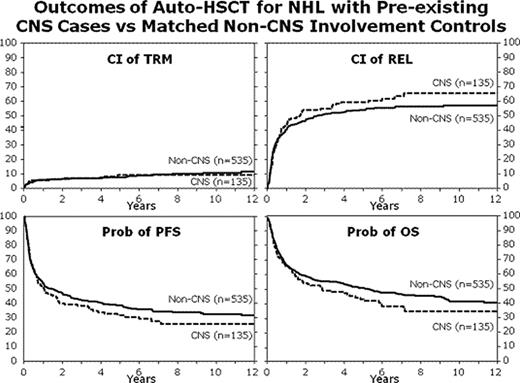
Various small, retrospective single institutional and registry analyses have suggested that pre-existing central nervous system (CNS) involvement was not a contraindication for autologous hematopoietic stem cell transplantation (aHSCT) for patients with non-Hodgkin's lymphoma (NHL). The outcomes of 151 adult patients with NHL with pre-existing CNS involvement (CNS+), identified as CNS involvement identified at any time in the course of their disease, undergoing aHSCT were analyzed and compared to 4688 patients who underwent the procedure but with no pre-existing CNS involvement (CNS−) during the years 1990–2005. There were significant baseline differences between the groups with CNS+ patients more likely to be younger, have lower performance status, higher age adjusted international prognostic index scores, more advanced disease stage at diagnosis, more aggressive histology, increased # of extranodal disease sites, and to have a shorter interval between diagnosis and aHSCT. There were no discernible differences in sex, immunophenotype, B symptoms at diagnosis, bone marrow involvement, # prior lines of therapy, conditioning regimens or disease status at aHSCT. Median follow-up of survivors was equivalent (CNS+: 77 months vs CNS− 73 months). Comparing the CNS+ with the CNS− groups, the univariate probabilities of DFS were 30 vs 35%, OS were 42 vs 49%, respectively. Cumulative incidence for relapse was 61 vs 57% and for NRM was 9 vs 8%, respectively. No statistically significant differences were identified between the two groups although there was a trend to higher relapse and lower OS for the CNS+ transplant group. Further analysis was performed on the CNS+ cohort, stratifying by disease status at time of aHSCT. Marked increase in relapse rates (72 vs 49%) with associated lower DFS (19 vs 46%) and OS (31 vs 58%) were found in patients with active CNS disease (Figure 1). With recognition that there were differences in disease presentation and risk features, a propensity analysis was performed on the original CNS− cohort to allow a case match control study, matched for number of high risk features but differing based upon CNS involvement. 135 CNS+ patients selected for B cell phenotype and common NHL subtypes were compared to 535 CNS− patients. On multi-variate analysis, no statistically significant differences in relapse rates, NRM, DFS and OS (Figure 2) were found comparing these groups in the case control study. Validation of the CNS− case match study population showed no differences in OS of the matched CNS− group with the non-matched CNS- population. In summary, NHL patients with CNS involvement in the course of their disease, despite often presenting with more adverse features, can achieve excellent long-term outcomes with aHSCT. However, optimal outcomes are only achieved when CNS disease control is present at the onset of the aHSCT.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.