Abstract
Abstract 3726
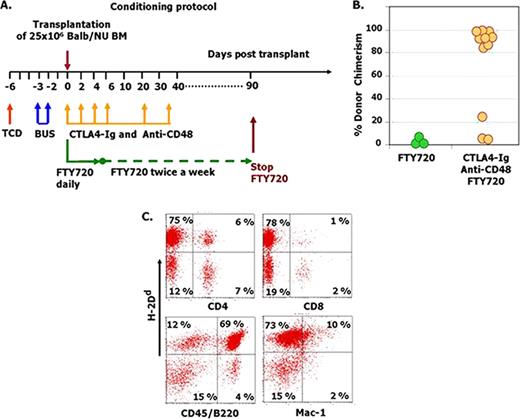
Induction of specific durable immune tolerance towards transplanted donor cells and tissues, without chronic administration of toxic immunosuppressive drugs, represents a most desirable goal in transplantation medicine. Two major approaches addressing this challenge have shown promise in rodent studies. The first is the use of co-stimulatory blockade to inhibit T cells with anti-donor specificity, and the second uses bone marrow (BM) transplantation to achieve a tolerizing chimeric state in which donor antigens are continuously presented in the host thymus. The exceptional clinical potential of the latter approach has been recently demonstrated in a pilot study of combined renal and bone-marrow transplantation from a single donor. However, the presence of alloreactive T cells in the BM graft imposes a significant risk for GVHD which is unacceptable in patients with non-malignant conditions. While T cell depleted BMT could prevent GVHD, the high rejection rate in the absence of aggressive conditioning treatment, represents a significant obstacle. More than a decade ago a co-stimulatory blockade based on anti CD40L was successfully used to induce chimerism following T depleted BMT. However, anti CD40L was later found to be thrombotic in humans, leading to a search for a safer protocol. In previous studies attempting embryonic pancreas xeno-transplantation (Tchorsh-Yutsis et al. Diabetes 2009), we were able to achieve optimal maintenance of the embryonic graft upon transient treatment with CTLA4-Ig and anti CD48, in conjunction with continuous immune suppression with FTY720. However, durable tolerance was not achieved and rejection ensued upon cessation of immune suppression. Therefore, in the present study we sought to investigate the potential of transient treatment with CTLA4-Ig, anti CD48 and FTY720, the equivalents of which are available for clinical use, combined with transplantation of ‘mega dose' T cell depleted BMT. If successful, such a protocol could achieve the desired durable tolerizing chimeric state. Considering the importance of providing empty niches for successful BM engraftment, we initially determined the minimal myeloablation with busulphan which can induce durable chimerism following infusion of congenic B6-SJL(Ly-5.1) TDBM (25×106) into B6 (Ly-5.2) mice. Testing doses ranging from 10mg/Kg to 100mg/Kg busulphan showed that donor type chimerism above 50% was attained at doses >50mg/Kg (40±26%, 66±7% and 75±2% chimerism at 50, 60 and 100 mg/Kg). Consequently, the sublethal dose of 60mg/Kg was selected for further use in all attempts to induce allogeneic chimerism, in conjunction with transient debulking of host lymphocytes by a single infusion of anti CD4 and anti CD8 depleting antibodies. The well tolerated combined sublethal conditioning presented a formidable barrier for engraftment of allogeneic ‘megadose' T cell depleted BM, and no chimerism was achieved. However, addition of transient post transplant treatment with CTLA4-Ig, anti CD48 and FTY720 (Fig 1A), led in two independent experiments to marked donor type chimerism with a median follow up of 116 days (range: 70 to 163 days) beyond cessation of immune suppression (Fig.1B). Thus, while no chimerism could be detected in mice treated post transplant with FTY720 alone (0/7), transient post transplant immune suppression with CTLA4-Ig, anti CD48 and FTY720 resulted in more than 80% donor type chimerism in 8 of 11 mice. As can be seen in Fig.1C, significant chimerism was attained in both the myeloid and lymphoid lineages. Since agents such as Belatacept (CTLA4-Ig) and Alefacept (blocking the interaction of CD48) are available for clinical use, our results suggest a potentially feasible co-stimulatory blockade approach for the induction of durable hematopoietic chimerism under non myeloablative conditioning, as a platform for cell therapy and organ transplantation.
Non myeloablative conditioning and co-stimulatory blockade for chimerism induction. (A) C3H/Hen recipient mice were conditioned with busulfan (2×30mg/Kg) and T cell debulking (TCD) with 300mg anti CD4 and anti CD8. Post transplant treatment included 200mg CTLA4 Ig, 250mg anti CD48, and 0.1mg FTY720 administered at the indicated time points. (B-C): Long term multilineage chimerism (A) Chimerism level 163 days after cessation of immune suppression. (B) Typical multilineage chimerism in the spleen of a chimeric mouse shown in B.
Non myeloablative conditioning and co-stimulatory blockade for chimerism induction. (A) C3H/Hen recipient mice were conditioned with busulfan (2×30mg/Kg) and T cell debulking (TCD) with 300mg anti CD4 and anti CD8. Post transplant treatment included 200mg CTLA4 Ig, 250mg anti CD48, and 0.1mg FTY720 administered at the indicated time points. (B-C): Long term multilineage chimerism (A) Chimerism level 163 days after cessation of immune suppression. (B) Typical multilineage chimerism in the spleen of a chimeric mouse shown in B.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.