Abstract
The risk of venous thromboembolism (VTE) is increased in cancer patients. To improve prediction of VTE in cancer patients, we performed a prospective and observational cohort study of patients with newly diagnosed cancer or progression of disease after remission. A previously developed risk scoring model for prediction of VTE that included clinical (tumor entity and body mass index) and laboratory (hemoglobin level and thrombocyte and leukocyte count) parameters was expanded by incorporating 2 biomarkers, soluble P-selectin, and D-Dimer. Of 819 patients 61 (7.4%) experienced VTE during a median follow-up of 656 days. The cumulative VTE probability in the original risk model after 6 months was 17.7% in patients with the highest risk score (≥ 3, n = 93), 9.6% in those with score 2 (n = 221), 3.8% in those with score 1 (n = 229), and 1.5% in those with score 0 (n = 276). In the expanded risk model, the cumulative VTE probability after 6 months in patients with the highest score (≥ 5, n = 30) was 35.0% and 10.3% in those with an intermediate score (score 3, n = 130) as opposed to only 1.0% in patients with score 0 (n = 200); the hazard ratio of patients with the highest compared with those with the lowest score was 25.9 (8.0-84.6). Clinical and standard laboratory parameters with addition of biomarkers enable prediction of VTE and allow identification of cancer patients at high or low risk of VTE.
Introduction
The association between cancer and venous thromboembolism (VTE) is well-established. Up to 20% of cancer patients develop VTE, which is recognized as one of the leading causes of death in these patients.1 However, the cancer population is heterogeneous in terms of thrombosis risk. Rates of VTE widely differ in subgroups of cancer patients and depend on the presence of various patient-, tumor-, and treatment-related risk factors.2-4
For instance, age, obesity, medical comorbidities, and immobilization add to the risk of VTE in the general population as well as in cancer patients.3-8 The primary site of cancer and the presence of metastatic disease are among the most important risk factors for cancer-associated thrombosis, with highest VTE rates observed in patients with brain, pancreatic and gastric cancer.2,5,7,9-11 Also patients with haematologic malignancies, particularly those with lymphoma and multiple myeloma, have relatively high rates of VTE.2,3,5 Furthermore, cancer-related treatments including chemotherapy and antiangiogenic agents, hormonal therapy, surgery, and erythropoiesis-stimulating agents predispose to VTE.3,4,7,9,12-14
In addition to the epidemiologic and treatment-related risk factors, in recent studies laboratory parameters have been reported to be associated with an increased risk of cancer-associated thrombosis. A high platelet count12,15 or a high leukocyte count16 have been shown to significantly increase the VTE risk. In our prospective cohort study, the Vienna Cancer and Thrombosis Study (CATS), our group was able to identify novel predictive biomarkers for cancer-associated VTE. Elevated levels (≥ 53.1 ng/mL) of the cell adhesion molecule soluble P-selectin (sP-selectin) were associated with a 2.6-fold increased risk of future VTE.17 Biomarkers reflecting activation of blood coagulation and fibrinolysis, such as high levels of D-Dimer and the prothrombin fragment 1 + 2 (F1 + 2), were also independently predictive of the occurrence of VTE in cancer patients.18,19
Despite the high rates of VTE in the cancer population and its significant impact on morbidity and mortality, primary thrombophrophylaxis in cancer patients is challenging, as the risk of VTE is not equal in all cancer patients, and as anticoagulation in patients with cancer is associated with increased bleeding complications compared with patients without cancer.20-23 Therefore, stratification of cancer patients according to their VTE risk is of the utmost clinical importance, since patients at high risk of developing VTE may benefit from primary thromboprophylaxis, whereas routine anticoagulation may even be unfavorable in patients of low risk of VTE on account of the associated high bleeding risk.
A novel and promising approach to stratify cancer patients according to their risk of VTE is the use of risk scoring models. Recently, a risk scoring model incorporating 5 clinical and laboratory parameters, such as the site of cancer, platelet count, hemoglobin and/or use of erythropoiesis-stimulating agents, leukocyte count, and body mass index (BMI) was developed by Khorana et al to predict chemotherapy-associated thrombosis in ambulatory cancer patients.16 However, this risk scoring system has not yet been independently validated in other studies. We have applied this risk model in the framework of our prospective observational cohort study for prediction of cancer-associated VTE. Furthermore, we have expanded the risk model by adding 2 new laboratory parameters (sP-selectin and D-Dimer) that had been previously identified to predict cancer-associated VTE to find out whether stratification of patients into high- and low-risk groups can thus be achieved more accurately.
Methods
Study population and design
The study population comprises patients enrolled between October 2003 and December 2008 in CATS, an ongoing prospective observational cohort study performed at the Medical University of Vienna with approval of the institutional ethics committee and in accordance with the Declaration of Helsinki. The detailed methodology of CATS, along with the exact inclusion and exclusion criteria for the study, have been described in detail in previous reports.17,18 In brief, the study includes cancer patients with newly diagnosed cancer or progression of disease after complete or partial remission who have not recently received chemotherapy (within the last 3 months), radiotherapy, and surgery (within the last 2 weeks). Patients with the following cancer sites, confirmed by histology, have been recruited into CATS: brain, breast, lung, stomach, colorectal, pancreas, kidney, prostate, and hematologic malignancies (myeloma and lymphoma). Patients give their informed consent and are followed prospectively for a 2-year observation period, until the occurrence of VTE or death, loss of follow-up, or withdrawal of consent. At the time of study entry venous blood samples are drawn to routinely perform a complete blood count and for further laboratory analyses.
Outcome measure
The main outcome measure of the study is objectively confirmed symptomatic or fatal VTE within 2 years after study inclusion.
Diagnosis of VTEs
There was no routine screening for VTE. Only when a patient developed symptoms of VTE, objective imaging methods were performed to confirm or exclude the diagnosis. Duplex sonography or venography were applied for diagnosis of deep vein thrombosis (DVT) and computerized tomography or ventilation/perfusion lung scan for diagnosis of pulmonary embolism (PE). In patients who died during follow-up, death certificates and, if available, autopsy findings were reviewed to establish a diagnosis of fatal PE.
Once-yearly VTE events were presented to an independent adjudication committee consisting of experts in the fields of angiology, radiology, and nuclear medicine who were informed of patients' medical history but were completely unaware of laboratory results. The members of the adjudication committee confirmed the diagnosis and examined and proved the clinical significance of these events. Accidentally detected thrombotic events (eg, PE detected in a routine computerized tomography) were considered events, when the adjudication committee decided that these events were of clinical significance.
Definition of risk scores
A risk scoring model was previously developed by Khorana et al based on clinical and laboratory parameters.16 According to this risk model, we assigned 2 points for a “very-high-risk” site of cancer (stomach, pancreas, or brain) and 1 point for a “high-risk” site of cancer (lung, kidney, lymphoma, or myeloma). To calculate the risk score, 1 point each was added for a platelet count of 350 × 109/L or more, hemoglobin less than 10 g/dL and/or use of erythropoiesis-stimulating agents, leukocyte count more than 11 × 109/L, and BMI of 35 kg/m2 or more. As in our study a relatively high number of patients with brain tumors (high-grade glioma) is also included (a malignancy known to be strongly associated with a very-high VTE risk), we allocated brain tumors to the “very-high-risk” sites of cancer. Our study also includes patients with myeloma and kidney carcinoma, which are known to have a relatively high risk of VTE; these cancer sites were allocated to the “high-risk” group. All other cancer sites were assigned to have 0 points, in the previous study as well as in our study.
The expanded model additionally includes sP-selectin and D-Dimer, with 1 point assigned to elevated sP-selectin (≥ 53.1 ng/mL) and 1 point to elevated D-Dimer (≥ 1.44 μg/mL). The cutoff points for elevated sP-selectin and elevated D-Dimer were chosen according to our clinical experience and previous findings.17,18 Now, we have also validated the predictive value of sP-selectin and D-Dimer for occurrence of VTE in cancer patients in a new and independent cohort of 305 cancer patients (detailed results are summarized in the supplemental materials, available on the Blood Web site; see the Supplemental Materials link at the top of the online article).
All clinical and laboratory parameters and complete follow-up information were available in 819 patients for calculation of the 2 (original and expanded) risk scoring models.
Statistical analysis
Continuous variables were described by median and the first and third quartile; categorical variables were described by absolute numbers and percentages, respectively. In Kaplan-Meier and some Cox regression analyses, for both risk scores the 3 groups with the highest scores were summarized into one high-risk group, because of the small numbers of patients in each of these groups. The median follow-up time was calculated by Kaplan-Meier analysis, but with the status indicator reversed. Kaplan-Meier analyses were applied to compare thrombosis-free survival among groups defined by risk scores and log-rank tests were used to test, whether differences among groups were statistically significant.
Hazard ratios for VTE were calculated by univariate and multivariable Cox regression analyses. We tested for a linear trend in the association of the risk scores with VTE and as this was significant (P < .001), we included the risk scores as continuous variables in the Cox regression models. The multivariable Cox regression analysis included additionally to the risk score variables for age at study inclusion, sex, chemotherapy, surgery, and radiotherapy. We assumed that surgery, chemotherapy, and radiotherapy would entail a modified risk for VTE not only at the exact timepoint of the procedure, but also for a certain time period immediately after the procedure. Therefore, 3 time-dependent dichotomous variables were included in the statistical model indicating times of possible influence on the VTE risk by surgery (from the day of surgery plus 6 consecutive weeks), chemotherapy (from the first day of a treatment cycle until the last day plus 4 weeks), or radiotherapy (from the first day of treatment until the last day plus 4 weeks). The Cox regression models were tested for all pairwise interactions and interactions with log(time) by candidate variables. As no significant interaction was found (P < .01), no interaction was added. For all Cox models the percentage explained variation was computed.24
Sensitivity, specificity, positive and negative predictive values for VTE at 6 months were calculated. A P value less than .05 was regarded as statistically significant. All calculations were conducted with SAS 9.2.
Results
Characteristics of the study population
The baseline characteristics of the investigated cohort of cancer patients (n = 819, 44.3% female), values of laboratory parameters included in the risk scoring models and information on the site of cancer and cancer treatments are given in Table 1. None of the study participants used an erythropoiesis-stimulating agent at study inclusion. Overall, 61 patients (7.4% of the total study population) developed VTE over a median follow-up of 656 (25th-75th percentile: 277-731) days. The cumulative probability of VTE was 6.0% (95% confidence interval [CI]: 4.5%-7.9%) after 6 months and 7.7% (6.0%-9.9%) after 1 year. PE was fatal in 4 (6.6% of VTE events) patients. In 8 patients PE was detected incidentally on computed tomography scan; they were, however, considered clinically significant by the adjudication committee and were therefore classified as an event. Detailed characteristics of cancer patients with VTE, site of VTE, classification of cancer and site of cancer are given in Table 2.
Risk and rates of VTE in relation to risk scores according to Khorana et al16
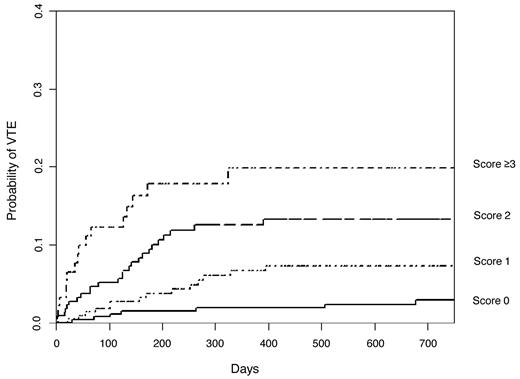
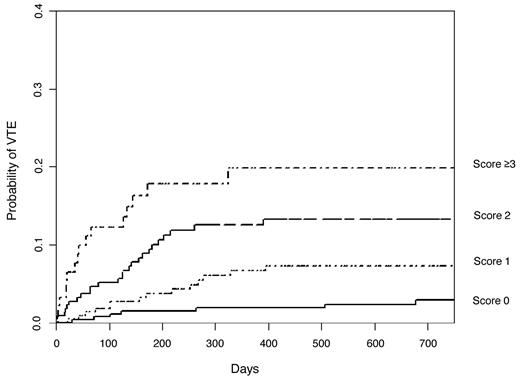
In Kaplan-Meier analysis, the cumulative probability of VTE after 6 months was 17.7% (95% CI: 11.0%-27.8%) in patients with the highest risk score (score ≥ 3, number of patients in this risk category = 93), 9.6% (6.2%-14.7%) in those with score 2 (n = 221), 3.8% (1.9%-7.4%) in those with score 1 (n = 229), and only 1.5% (0.6%-3.9%) in patients with score 0 (n = 276; logrank test, P < .001; Figure 1). The linear trend for association of risk scores with VTE was statistically significant (P < .001). In univariate Cox regression analysis, the hazard ratio (HR) of VTE was 2.1 (95% CI: 1.6-2.6) per 1 point increase in the risk score and remained unchanged after adjustment for age, sex, chemotherapy, surgery, and radiotherapy (2.1 [1.6-2.8]). Compared with patients with risk score 0, the HRs of patients with scores 1, 2 and ≥ 3 for developing VTE were 2.7 (1.1-6.6), 5.5 (2.4-12.6), and 9.5 (3.9-23.1), respectively.
Kaplan-Meier estimates of the risk of VTE in patients with risk scores 0, 1, 2, and ≥ 3 according to the risk scoring model developed by Khorana et al.16 The cumulative probability of VTE showed statistically significant association with the risk scores (log-rank test, P < .001).
Kaplan-Meier estimates of the risk of VTE in patients with risk scores 0, 1, 2, and ≥ 3 according to the risk scoring model developed by Khorana et al.16 The cumulative probability of VTE showed statistically significant association with the risk scores (log-rank test, P < .001).
At 6 months and at the cutoff point for high risk (score ≥ 3), we calculated the sensitivity (probability of high risk in those patients experiencing VTE), specificity (probability of low risk in those not experiencing VTE), positive predictive value (PPV, probability of VTE in those patients identified to be at high risk), and negative predictive value (NPV, probability of no VTE in those patients identified to be at low risk) for this model. The sensitivity was 31.9%, the specificity 91.9%, the PPV 22.1%, and the NPV 94.9%.
Risk and rates of VTE in the expanded risk scoring model
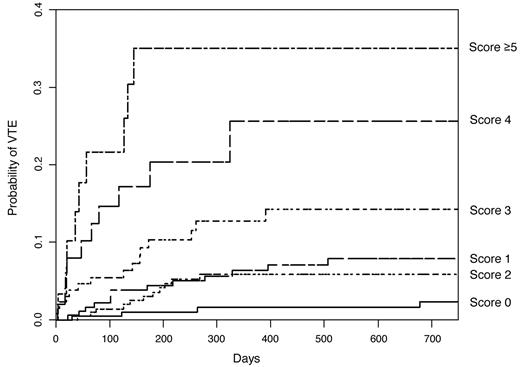
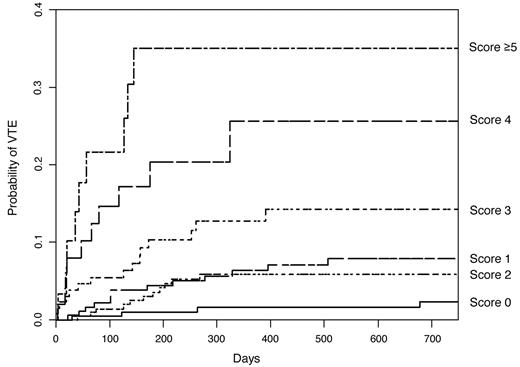
In the expanded risk scoring model including sP-selectin and D-Dimer the stratification turned out to be considerably improved. The VTE rates were significantly higher in risk groups with a high score than in those with a low score. The cumulative probability of developing VTE after 6 months was 35.0% (19.7%-57.0%) in the subgroup of patients with score ≥ 5 (n = 30), 20.3% (11.0%-35.7%) in patients with score 4 (n = 51), 10.3% (5.9%-17.5%) in those with score 3 (n = 130), 3.5% (1.8%-7.3%) in those with score 2 (n = 218), 4.4% (2.2%-8.6%) in those with score 1 (n = 190), and only 1.0% (0.3%-4.0%) in the subgroup with score 0 (n = 200; log-rank test, P < .001; Figure 2). The expanded risk model also showed statistically significant association with VTE (P for linear trend < .001). In univariate and multivariate Cox regression analysis, a 1 point increase in the risk score was associated with 1.8-fold (1.5-2.2) and 1.9-fold (1.6-2.2) increase in the HR for VTE, respectively. Compared with patients with the lowest-risk score (score 0), the HR of those with the highest-risk score (score ≥ 5) for VTE was 25.9 (8.0-84.6). The HRs of patients with scores 1, 2, 3, and 4 compared with score 0 were 3.7 (1.2-11.5), 2.9 (0.9-9.1), 7.0 (2.3-21.4), and 15.6 (4.9-50.0), respectively.
Kaplan-Meier estimates of the risk of VTE in the expanded risk scoring model including sP-selectin and D-Dimer. The cumulative probability of developing VTE was significantly higher in patients with a high score than in those with a low score (log-rank test, P < .001).
Kaplan-Meier estimates of the risk of VTE in the expanded risk scoring model including sP-selectin and D-Dimer. The cumulative probability of developing VTE was significantly higher in patients with a high score than in those with a low score (log-rank test, P < .001).
For the expanded model, the sensitivity at the cutoff point for highest risk (score ≥ 5) and at 6 months was 19.1%, specificity 98.2%, PPV 42.9%, and NPV 94.4%. Table 3 shows the sensitivity, specificity, PPV, and NPV at the cutoff point of different risk scores.
Discussion
In this observational cohort study we have confirmed that cancer patients at high or low risk of VTE can be identified prospectively, when risk assessment models are applied. The risk scoring system previously developed by Khorana et al,16 which incorporated site of cancer, platelet count, hemoglobin and/or use of erythropoiesis-stimulating agents, leukocyte count, and BMI, also turned out to be useful in our patient cohort. With our expanded risk model, which included sP-selectin and D-Dimer, 2 biomarkers identified in our study to predict cancer-associated thrombosis, we could show that risk prediction can be considerably improved. In patients with the highest compared with patients with the lowest risk, the probability for VTE was 26-fold higher.
Because we have based the risk model on previous findings, we validated the risk scoring model by Khorana et al who used 5 clinical and laboratory parameters routinely available in every patient initiating chemotherapy.16 The sensitivity and specificity of the original risk scoring system for VTE in the previous and the current study was comparable, which underlines the reproducibility of the risk model. Although the results concerning the ability to identify cancer patients at high or low risk of VTE are consistent between both studies, some differences have to be pointed out. In the current study VTE events were subsequently evaluated by an independent adjudication committee, whereas VTE diagnosis in the previous study had been done by the treating physicians. In contrast to the previous study, which had aimed to identify risk factors for chemotherapy-associated thrombosis, the VTE rates in our study were higher (2.1% vs 7.4%). This is most probably due to the different follow-up times of the 2 studies (2.5 months in the previous study and median 21.4 months in our study) and the higher proportion of high-risk cancer sites, such as brain, gastric, and pancreatic tumors in our study. Whereas Khorana et al included only patients who underwent chemotherapy, our study includes a more heterogeneous cohort of cancer patients undergoing also surgery or radiotherapy or even untreated patients. In our multivariate model, we have corrected for these time-dependent risk parameters, and still, the scoring models have turned out to be a good predictor for future VTE in cancer patients.
We have demonstrated that cancer patients at a very high risk of VTE can be defined more precisely, and the probability of VTE can be predicted more accurately, when additional parameters are added to Khorana's risk model. Several recent studies have reported that stratification of cancer patients according to their VTE risk can be accomplished by measuring biomarkers.6,17-19,25 The 2 markers sP-selectin and D-Dimer have shown to improve the risk prediction of VTE considerably.
The advantage of the “Khorana-Score” is that all parameters of this risk model are routinely determined in cancer patients at diagnosis or the beginning of antineoplastic therapy and are readily available, whereas for the expanded risk assessment model additional laboratory tests have to be performed. D-Dimer is a well-studied biomarker in the diagnosis and management of VTE and a risk factor for VTE recurrence with potential implications for deciding on the duration of oral anticoagulation for secondary VTE prophylxis in noncancer patients.26-29 sP-selectin is a cell adhesion molecule that promotes thrombus formation and exhibits procoagulant properties per se.26,30,31 Recent data suggest that sP-selectin is associated with primary and recurrent thrombosis in noncancer patients.32-34 sP-selectin can be easily and accurately measured by ELISA, which has been demonstrated previously by our group.17,32 We have also validated the predictive power of elevated sP-selectin and elevated D-Dimer for occurrence of VTE in cancer patients in a new and independent cohort of 305 cancer patients (see supplemental material for detailed results). D-Dimer and sP-selectin are both continuous parameters and the assignment of a point of “1” at the predefined cutoff level in our study is based on our previous data and clinical experience. The definitions of cutoff levels for continuous parameters and the appropriate assignment of points in the risk scoring models may be refined by further statistically analysis. Whether other biomarkers may also contribute to a more precise and accurate prediction when additionally added to Khorana's risk model was not tested in our current study, but could be assumed.
The sensitivity and specificity of our model incorporating additional variables are comparable with those of D-Dimer testing for the assessment of a suspected acute VTE.27 At the cutoff point of score 1 the sensitivity of our model of 96% was high enough to identify cancer patients at a low risk of VTE, who may be excluded from thromboprophylaxis and at a higher cutoff point (score ≥ 5) the specificity of the model of 98% was satisfying to find those patients with an increased VTE risk, who may benefit from thromboprophylaxis. The NPV of the risk model at each cutoff point was between 93% and 99%. However, as expected the PPV was as low as the PPV reported for D-Dimer. Although the stratification of cancer patients at risk of VTE could be achieved more accurately in the expanded model, the inclusion of additional biomarkers may lead to additional costs. Whether it is worthwhile to draw on finer risk categories when deciding on the need for primary thromboprophylaxis, and if this contributes to a better cost-benefit ratio, still needs to be evaluated in interventional and randomized controlled trials.
According to this risk assessment model, the VTE risk in the high-risk group of cancer patients was much higher compared with other well-defined patient groups, such as hospitalized, medically ill patients after general surgery, and even much higher than in patients with orthopedic surgery.35-39 It has to be considered that we did not screen for VTE, but that our rates of VTE exclusively comprised symptomatic events. Thromboprophylaxis has been shown to be effective in these high risk situations.39 However, routine prophylactic anticoagulation is currently not established in ambulatory cancer patients, except for patients treated with thalidomide or lenalidomide.40 Risk assessment models that accurately and prospectively categorize cancer patients with respect to their VTE risk may help clinicians to tailor anticoagulant therapy and lead to improved use of thromboprophylaxis, thus maximizing the clinical benefit and cost-effectiveness of primary prophylaxis and additionally minimizing the risk of bleeding complications, which is considerably higher in cancer patients.41 The efficacy and safety of routine thromboprophylaxis in high-risk groups of cancer patients identified by these models need to be assessed in randomized controlled trials.
In conclusion, reproducible and simple scoring systems in cancer patients are useful to individually stratify patients according to their VTE risk and to optimize thromboprophylaxis. Interventional trials based on risk assessment models are needed to demonstrate effectiveness and safety of thromboprophylaxis in high-risk patients.
An Inside Blood analysis of this article appears at the front of this issue.
The online version of this article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank all persons who have supported us in patient recruitment for CATS: Prof Dr Thomas Brodowicz, Prof Dr Wolfgang Füreder, Prof Dr Alexander Gaiger, Prof Dr Heinz Gisslinger, Prof Dr Michael Hejna, Prof Dr Ulrich Jäger, Prof Dr Paul Knöbl, Prof Dr Michael Krainer, Prof Dr Gabriela Kornek, Prof Dr Christine Marosi, Prof Dr Leopold Öhler, Prof Dr Robert Pirker, Prof Dr Markus Raderer, Prof Dr Werner Scheithauer, Prof Dr Manuela Schmidinger, Dr Cathrin Skrabs, Prof Dr Günther Steger, Prof Dr Peter Valent, Prof Dr Herbert Watzke, Prof Dr Christoph Wiltschke, Prof Dr Sabine Zöchbauer-Müller, Dr Marco Hassler, Prof Dr Irene Kührer, Dr Axel Eisenhut, Prof Dr Michael Gnant, Prof Dr Bela Teleky, Prof Dr Richard Pötter, Dr Gregor Goldner, Prof Dr Ute Dieckmann, Prof Dr Gerda Hohenberg, Prof Dr Petra Munda, Prof Dr Ernst Kubista, Prof Dr Martin Schwarz, Magdalena Pabinger, and many more colleagues (all from the Medical University of Vienna).
We thank Richard Rataj, Heidi Dude, Judith Raglhofer (Clinical Institute of Medical and Chemical Laboratory Diagnostics, Medical University of Vienna), and Silvia Koder (Clinical Division of Hematology and Haemostaseology, Department of Medicine I, Medical University of Vienna) for management of blood samples and technical assistance.
We thank the members of the adjudication committee: Prof Dr Renate Koppensteiner, Dr Markus Haumer, and Prof Dr Andrea Willfort-Ehringer (Department of Angiology, Medical University of Vienna); Prof Dr Sylvia Metz-Schimmerl (Department of Diagnostic Radiology, Medical University of Vienna); and Prof Dr Robert Dudczak (Department of Nuclear Medicine, Medical University of Vienna)
We thank Tanja Altreiter, MA (Clinical Division of Hematology and Haemostaseology, Department of Medicine I, Medical University of Vienna) for proofreading this manuscript.
This study was supported by a grant from the Jubiläumsfonds of the Austrian National Bank (project numbers 10935 and 12739) and an unrestricted grant from Pfizer Austria.
Authorship
Contribution: C.A. acquired data, analyzed and interpreted data, drafted the manuscript, critically revised the manuscript for important intellectual content, obtained funding, and provided administrative, technical, or material support; D.D. analyzed and interpreted data, drafted the manuscript, critically revised the manuscript for important intellectual content, and performed statistical analysis; C.M. acquired data and critically revised the manuscript for important intellectual content; A.-L.C. acquired data and provided administrative, technical, or material support; R.V. designed and conceived the study, analyzed and interpreted data, and obtained funding; R.S. acquired data and provided administrative, technical, or material support; P.Q. critically revised the manuscript for important intellectual content and provided administrative, technical, or material support; C.Z. designed and conceived the study, analyzed and interpreted data, and critically revised the manuscript for important intellectual content; I.P. designed and conceived the study, analyzed and interpreted data, drafted the manuscript, critically revised the manuscript for important intellectual content, obtained funding, and supervised the study; and all authors reviewed and edited the entire manuscript and approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Ingrid Pabinger, Clinical Division of Haematology and Haemostaseology, Department of Medicine I, Medical University of Vienna, Waehringer Guertel 18-20, A-1090 Vienna, Austria; e-mail: ingrid.pabinger@meduniwien.ac.at.