To the editor:
Mechanisms for anemia in patients with nephrotic syndrome (NS) are complex and incompletely understood. Copper is an essential mineral in red blood cell metabolism. It is absorbed in the intestine, bound to its carrier protein, transported to the liver, and stored. Up to 95% of serum copper is bound to ceruloplasmin. Mouse models have shown that severe copper deficiency results in profound neutropenia1 and anemia.2 In humans, copper deficiency, which has been reported mostly in patients with chronic intestinal dysfunction, leads to anemia, neutropenia,3 and dysmyelopoietic features.4 Copper deficiency is thought to worsen anemia in patients with kidney failure.5 However, copper deficiency anemia has not yet been described in the congenital NS infant.
The patient was born at 40 weeks' gestational age. At 6 months of age, a nephrotic syndrome developed. Clinically, the patient suffered from asthenia, anorexia, and edema. Biologically, proteinuria was at 33 g/L, and serum albumin level was as low as 6 g/L before high-dose intravenous albumin infusion. Renal biopsy showed a slightly thickened mesangium, with tubular atrophy and dilated tubuli. Genetic analysis revealed a heterozygote mutation in the NPHS2 gene (c.714G>T in exon 5, leading to p.Arg238Ser) coding for podocin. No mutations were detected in the NPHS1 gene.
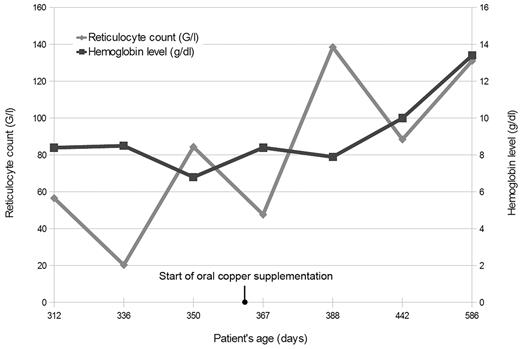
At 7 months of age, severe aregenerative anemia (hemoglobin level as low as 5.0 g/dL) was detected; neutrophils (1.6 × 109/L) and lymphocytes (2.5 × 109/L) were low. An infectious work-up (including HIV, hepatitis A/B/C, CMV, and EBV) came back negative. Hemoglobin electrophoresis was normal. Hemolysis was ruled out because haptoglobin was not low, and both LDH and unconjugated bilirubin were normal. Antinuclear antibody, SSA, and SSB tests were negative for lupus. Early bone marrow biopsy only showed few hypochromic erythroblasts; no vacuolated erythroids were detected. Total copper serum level was low (0.32 mg/L, normal range 1.08 to 1.44 mg/L), along with ceruloplasmin level (0.2 g/L, normal range 0.22 to 0.61 g/L). Transferrin level was slightly below normal values (1.4 g/L, normal range 2 to 3.5 g/L). Anemia was refractory to erythropoietin (NeoRecormon 6000 UI per week), iron, and vitamin B12 supplementation, which has been described.6 Blood transfusions had a very transient efficiency. Oral supplementation of copper gluconate was started (10.2 mg per day, progressively increased to as high as 31 mg per day) while monitoring hemoglobin level and reticulocyte count (Figure 1). Ceruloplasmin and total copper serum level remained low throughout supplementation because of persistent urinary loss of ceruloplasmin. However, increase of free copper was correlated with an increase in white cell count, hemoglobin level, and reticulocyte count.
In conclusion, urinary losses because of massive proteinuria may cause copper depletion, involved in the pathogenesis of neutropenia and anemia. Interestingly, whereas normal doses of oral copper gluconate were sufficient to increase white blood cell count, high doses were necessary to lead to an increase in hemoglobin level. Therefore, it should be considered to help correct refractory aregenerative anemia in NS patients.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Olivier Niel, Pediatric Resuscitation, L'Archet 2 Hospital, 151 Route de Saint-Antoine de Ginestière, 06200 Nice, France; e-mail: o.r.p.niel@free.fr.