Abstract
The clinical value of imaging is well established for the follow-up of many lymphoid malignancies but not for chronic lymphocytic leukemia (CLL). A meta-analysis was performed with the dataset of 3 German CLL Study Group phase 3 trials (CLL4, CLL5, and CLL8) that included 1372 patients receiving first-line therapy for CLL. Response as well as progression during follow-up was reassessed according to the National Cancer Institute Working Group1996 criteria. A total of 481 events were counted as progressive disease during treatment or follow-up. Of these, 372 progressions (77%) were detected by clinical symptoms or blood counts. Computed tomography (CT) scans or ultrasound were relevant in 44 and 29 cases (9% and 6%), respectively. The decision for relapse treatment was determined by CT scan or ultrasound results in only 2 of 176 patients (1%). CT scan results had an impact on the prognosis of patients in complete remission only after the administration of conventional chemotherapy but not after chemoimmunotherapy. In conclusion, physical examination and blood count remain the methods of choice for staging and clinical follow-up of patients with CLL as recommended by the International Workshop on Chronic Lymphocytic Leukemia 2008 guidelines. These trials are registered at http://www.isrctn.org as ISRCTN 75653261 and ISRCTN 36294212 and at http://www.clinicaltrials.gov as NCT00281918.
Introduction
For most lymphoid malignancies, the use of computed tomography (CT) scanning is clearly recommended by the most recent version of response criteria.1 CT scans are mandatory for initial staging as well as for the evaluation of response and detection of relapse during follow-up.2-5 For chronic lymphocytic leukemia (CLL) the role of CT scan has not been clearly defined according to the National Cancer Institute Working Group (NCI-WG) criteria6 : CT scans were recommended “when clinically indicated.” The definition of complete remission (CR) according to these criteria included the “absence of lymphadenopathy by physical examination and appropriate radiographic techniques.” Therefore, and in contrast to other lymphoma entities, the role of CT scans has become a constant matter of debate for the planning of clinical trials and routine practice of patients with CLL.
The authors of 3 studies7-9 showed that the lymph node diameter as determined clinically or by CT scans has some prognostic impact in predicting the time to relapse and/or time to retreatment. Moreover, the use of CT scans seemed to lower the rate of complete remissions and the overall response10,11 but had little impact on predicting progression-free survival.
In the recently published International Workshop on Chronic Lymphocytic Leukemia (IWCLL) criteria, researchers have attempted to limit the routine use of CT scans in CLL by recommending a total of 2 CT scans (before and after treatment) for patients included in clinical trials.12 However, this recommendation has not been substantiated by experimental data or clinical trials. To clarify the clinical role of CT scans for the follow-up and staging of CLL patients, we performed a meta-analysis by using the data of 3 phase 3 studies (CLL4, CLL5, and CLL8 protocol of the German CLL Study Group) to evaluate the clinical relevance of imaging for the follow-up of CLL patients.
Methods
Study population
This meta-analysis was based on the results of 1398 patients receiving first-line therapy for CLL within a phase 3 trial of the German CLL Study Group (CLL4, CLL5, or CLL8 protocols)11,13,14 between 1999 and 2006. Twenty-six patients were excluded because of violation of the inclusion or exclusion criteria. A total of 1372 patients included in all clinical trials had a confirmed diagnosis of CLL, were previously untreated, and in an advanced stage (Binet stage C or Binet stage B or A with active disease). A total of 362 patients younger than 65 years of age were included in the CLL4 trial, 193 patients older than 64 years in the CLL5 trial, and 817 patients without any age limit but with normal renal function and a low comorbidity burden defined by a cumulative illness rating score15 of up to 6 were included in the CLL8 trial. Within the CLL4 trial patients were randomized between first-line therapy with fludarabine versus fludarabine plus cyclophosphamide (FC), within the CLL5 trial between fludarabine and chlorambucil treatment, and within the CLL8 trial between FC and FC plus rituximab (FCR) therapy. With the exception of chlorambucil treatment, which was administered for 12 months or until the maximum response was achieved, all other treatment regimen consisted of 6 cycles. A total of 100 patients received chlorambucil, 275 patients fludarabine, 589 FC, and 408 patients FCR.
All study protocols were approved by the institutional review board of the University of Munich and University of Cologne, respectively. All patients had signed an informed-consent form before study entry in accordance with the Declaration of Helsinki. These trials are registered at http://www.isrctn.org as ISRCTN 75653261 and ISRCTN 36294212 and at http://www.clinicaltrials.gov as NCT00281918.
Response assessment
After 3 and 6 courses of fludarabine, FC or FCR therapy as well as after 3, 6, 9, and 12 months of chlorambucil treatment the treatment response was assessed according to the NCI-WG criteria.6 During follow-up response duration was assessed every 3 months during the first 2 to 3 years and then every year for the CLL4 and CLL5 trial and every 6 months for the CLL8 trial, respectively, according to the NCI-WG criteria.6 CT scans or other radiologic examinations were not performed by routine but were recommended at pretherapeutic staging, interim and final staging, and during the follow-up phase, if clinically indicated according to NCI-WG 1996 recommendations.6 CT scans were performed and evaluated by the local radiologist of the participating center. A member of the central medical review reevaluated the response assessment after therapy and during follow-up according to strict algorithm determined by the NCI-WG criteria.6
Statistical analysis
Statistical analysis was performed on intent-to-treat basis including all eligible patients. Time to event was estimated by use of the Kaplan-Meier method and treatment comparison was tested with the log-rank test. Overall survival was calculated from randomization to death and progression-free survival from randomization to the time of disease progression according to NCI or death. Patient groups were compared by the chi-square test and the Fisher exact test, respectively, if the expected count less than 5 was larger than 20%. All statistical tests were 2-sided. Statistical significance was defined at a P value less than 5%. The analysis was performed with SPSS V16.0. The analysis presented here was determined from the data collected by June 2008.
Results
Patients' characteristics
The median overall follow-up time for all patients alive included in this meta-analysis was 31 months (54 months for the CLL4 trial, 40 months for the CLL5 trial, and 26 months for the CLL8 trial). During follow-up period, CT scans were performed in 569 patients (52% of all patients in follow-up), ultrasound examinations in 936 patients (85%), and chest radiographs in 606 patients (55%). At least one imaging technique (CT scan, ultrasound, or radiograph) was conducted in 1089 patients (78%). In 309 patients (22%) no imaging examination was performed during the whole study period. Patients with at least one imaging examination were compared with those without imaging assessment with regard on the distribution of clinical parameters as well treatment outcome (Table 1). An imbalance between these 2 groups was detected: the group of patients who underwent imaging examinations was younger and contained more physically fit and more Binet stage B patients, in whom progressive disease was not clinically apparent.
Use of imaging diagnostics during the studies
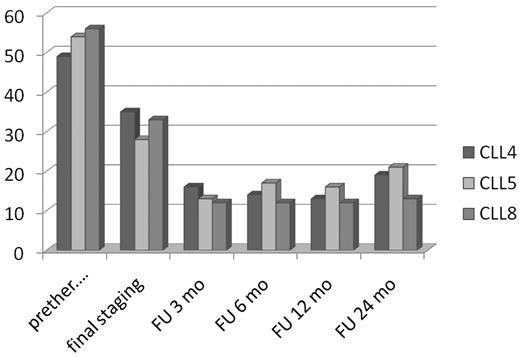
During the whole study period, a total of 10 915 imaging techniques were performed, including 2324 CT scans. The median time between 2 CT scans was 4.0 months. With respect to the follow-up period, 2111 imaging techniques and 569 CT scans were conducted. Figure 1 shows the distribution of CT scans performed per patient within the 3 clinical trials. Despite significant differences for all 3 phase III trials in age groups, physical fitness and years of examination there were no major imbalances in the distribution of CT scans.
Percent of patients with CT scans performed at different time points for each of the clinical trials included in this meta-analysis.
Percent of patients with CT scans performed at different time points for each of the clinical trials included in this meta-analysis.
CT scans and detection of progressive disease during follow-up
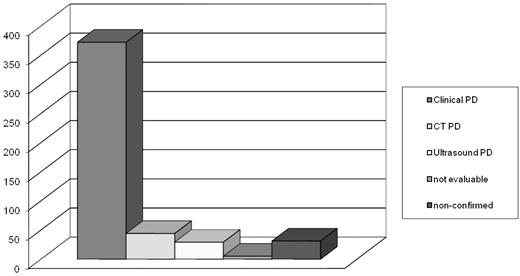
We evaluated the number of patients for whom the radiologic examination was crucial to determine disease progression (PD) according to the NCI-WG criteria. A total of 481 cases were considered as PD during treatment or follow-up. In 372 patients (77%) progression was clinically detected by physical examination and/or blood count though 195 patients (52%) had a CT scan at the same time point as well (Figure 2). In 15% of the 481 cases the detection method of progression was determined by imaging technique (9% CT scans, 6% ultrasound). Five patients with documented progressive disease could not be reevaluated because of a missing reference examination at pretherapeutic evaluation. In 31 patients (6%) the assessment of progressive disease by the treating physician could not be confirmed by a strict, independent application of the NCI-WG criteria. These patients were therefore assessed as stable disease.
Detection of progressive disease by method of examination. In 77% of the patients, PD was detected clinically by physical examination and/or blood count, in 9% by CT scan, in 6% by ultrasound, and in 1% the detection method was not evaluable because the reference result was missing. In 6% of the patients PD, as documented by the treating physician, could not be confirmed by the strict algorithm according to the NCI-WG criteria and were therefore assessed as stable disease.
Detection of progressive disease by method of examination. In 77% of the patients, PD was detected clinically by physical examination and/or blood count, in 9% by CT scan, in 6% by ultrasound, and in 1% the detection method was not evaluable because the reference result was missing. In 6% of the patients PD, as documented by the treating physician, could not be confirmed by the strict algorithm according to the NCI-WG criteria and were therefore assessed as stable disease.
CT scans and relapse treatment
The number of patients for whom CT scans or ultrasound examinations led to the initiation of a relapse treatment attributable to a bulky lymph node (defined as a diameter of > 5 cm) was assessed. Of 176 patients receiving relapse treatment attributable to progression, only 2 patients (1%) received retreatment on the basis of the result of CT scan or ultrasound. In these 2 patients a new bulky lymphadenopathy was detected by radiologic examination, whereas results of the physical examination and blood count were normal. In the remaining 174 patients clinical symptoms and/or results of the blood count were the underlying cause for initiating relapse treatment.
Prognostic value of bulky disease
Next, we evaluated the prognostic value of bulky disease, detected by radiologic examination at pretherapeutic staging. During pretherapeutic staging a CT scan was performed in 721 of 1372 patients (53%). An ultrasound was performed in 996 patients (73%). Overall a pretherapeutic imaging technique was applied in 1245 patients (91%).
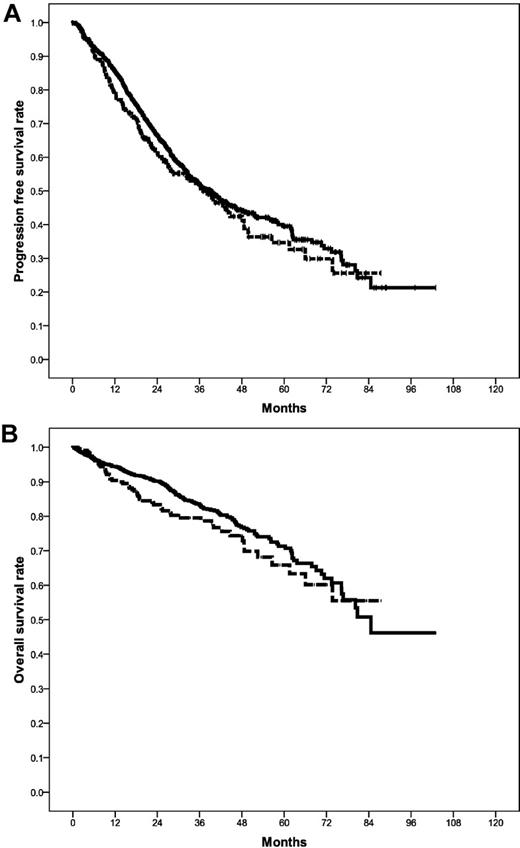
Bulky disease, defined as lymph node diameter > 5 cm, was found in 233 patients (17%) before treatment initiation. Response rates and survival times were correlated with the initial detection of bulky lymph nodes by CT scan or ultrasound. No significant difference in overall response rates between patients with and without bulky lymph nodes were detected (86% vs 89%, P = .2). The number of CRs was greater in patients without bulky lymph node (22% vs 29%, P = .02). However, progression-free survival (Figure 3A) and overall survival (Figure 3B) showed no significant difference between both cohorts (36 vs 39 months, P = .2 and 85 months vs median overall survival not reached, P = .08, respectively).
Prognostic impact of bulky lymphademopathy. Progression-free (A) and overall survival (B) for patients with versus without bulky lymphadenopathy detected by pretherapeutic imaging methods (CT scan or ultrasound). No significant difference in progression free (P = .2) and overall survival (P = .08) was assessed.
Prognostic impact of bulky lymphademopathy. Progression-free (A) and overall survival (B) for patients with versus without bulky lymphadenopathy detected by pretherapeutic imaging methods (CT scan or ultrasound). No significant difference in progression free (P = .2) and overall survival (P = .08) was assessed.
Impact of CT scans on the prognosis of complete remissions
To assess the impact of CT scans on the prognosis of CR rates we analyzed the progression-free survival in 2 patients groups with differently defined complete remissions. Patients in the one group (n = 248) fulfilled all criteria according to the NCI WG criteria6 and IWCLL criteria,12 which are mandatory for all patients, including normal physical examination, normal peripheral blood count, and bone marrow biopsy. The other group (n = 96) was defined by additionally performed CT scans (of the abdomen and/or thorax), confirming the complete remission. When pooling the data of all patients—independent of the clinical trial—we found that progression-free survival at the 75% percentile was 36 months in the group of patients with CR by clinical examination and bone marrow biopsy versus 49 months in the group of patients with additionally negative CT scans (P = .04; Figure 4A). The difference in progression-free survival was most evident in the CLL 4 trial comparing fludarabine alone versus FC (44 months vs not reached at 75% percentile, P = .015; data not shown). Interestingly, within the CLL8 trial comparing FC versus FCR no difference between the 2 CR groups was detected (35 months vs 41 months at 75% percentile, P = .44; Figure 4B).
Prognostic impact of complete remission confirmed by CT scan. Progression-free survival for all 3 studies (A) and for the CLL8 trial (B) (FC vs FCR) for patients with CRs additionally confirmed by CT scans versus CRs confirmed by clinical examination and bone marrow biopsy only. In all studies median progression-free survival was significantly longer in patients with additionally performed CT scans in comparison with those without (P = .04). The CLL8 trial evaluating the role of chemoimmunotherapy (B) showed no difference between both CR definitions (P = .44)
Prognostic impact of complete remission confirmed by CT scan. Progression-free survival for all 3 studies (A) and for the CLL8 trial (B) (FC vs FCR) for patients with CRs additionally confirmed by CT scans versus CRs confirmed by clinical examination and bone marrow biopsy only. In all studies median progression-free survival was significantly longer in patients with additionally performed CT scans in comparison with those without (P = .04). The CLL8 trial evaluating the role of chemoimmunotherapy (B) showed no difference between both CR definitions (P = .44)
Discussion
The results of this meta-analysis indicate that the use of imaging techniques and CT scans in particular in the follow-up period after first line treatment of patients with CLL has limited clinical benefit. The majority of events defined as disease progression was detected by physical examination and/or blood count. Moreover and more importantly, the results of the imaging methods rarely influenced the decision to initiate relapse treatment after first-line therapy. These data confirm the recent recommendation by the IWCLL guidelines12 that physical examination and blood count remain the methods of choice for clinical follow-up of patients with CLL in routine practice and within clinical trials.
This meta-analysis from 3 randomized phase 3 trials includes a large data set based on 1372 patients. Because the use of imaging methods for staging and follow-up was not mandatory within these trials, a bias between the 2 patient groups (patients with or without imaging diagnostics) was observed: As shown in Table 1, patients in whom imaging diagnostics were used were younger and physically fitter. Therefore, the results of our analysis seem to reflect rather the situation of these younger and fitter patients with CLL. The use of imaging diagnostics is reduced in the group of elderly and/or comorbid patients attributable to potential toxicity (eg, of CT contrast liquids in patients with impaired renal function) and lack of clinical consequences in this patient group where treatment decisions are made under palliative aspects and tend to be more symptom-based. The data presented here confirm the strategy to be more restrained with use of imaging diagnostics in elderly and comorbid patients because they rarely influence therapeutic decisions and may present an additional burden for this group of patients.
The results of this meta-analysis might be of general importance for the clinical practice in that they prevent unnecessary patient exposure to irradiation for the patient and reduce health care costs. Moreover, certain imaging techniques, such as CT scans, are not widely available in some regions of the world and may require some effort for patients to visit to the next radiology center.
In specific clinical situations, the use of CT scans or ultrasound of the abdomen might add important information during the follow-up of patients with CLL, especially when treatment decisions rely on that information. First, if an alemtuzumab-based regimen is considered for the treatment of relapsed disease, an imaging technique should be performed to assess the abdominal or mediastinal lymph node mass. Patients with lymph nodes of more than 5 cm in diameter are known to respond poorer to alemtuzumab monotherapy9,16 and should therefore be considered to receive a different treatment regimen in case of bulky disease. Second, radiologic examinations might be useful before starting the conditioning regimen for allogeneic stem cell transplantation. The tumor burden before allogeneic stem cell transplantation has been shown to be a major prognostic factor for the outcome of allogeneic stem cell transplantation.17
Although the up-dated IWCLL guidelines recommend chest radiograph for the staging of CLL,12 no disease progression was detected by this method. In contrast to the indications for CT scan and ultrasound examination of the abdomen, chest radiographs have a very limited role for the follow-up of CLL patients.
As for the prognostic value of imaging techniques for CLL, 2 recently published trials showed the association of thoracic or abdominal lymph node masses detected by CT scan with significantly shorter progression free and treatment free survival in both, advanced and early stage of the disease.7,8 However, both studies failed to show a statistically significant survival benefit for patients with normal abdominal CT or low lymphadenopathy burden. The data of the meta-analysis presented here show no statistically significant difference for progression-free and overall survival between patients with or without bulky lymphadenopathy detected by initially performed CT scan. With the availability of novel biologic markers, such as genetics (fluorescence in situ hybridization), immunoglobulin variable heavy-chain mutational status, ZAP 70, CD 38, and the serum markers beta2-microglobulin and serum thymidine kinase, a detailed evaluation of the individual prognosis is now possible.18-22 In particular, the evaluation of genetic aberrations by the use of fluorescence in situ hybridization is able to predict the response to various chemo(immuno)therapy regimens.17,23-26 Our data provide strong evidence that imaging techniques play a minor, if any, role for the prognostic evaluation of patients with CLL who undergo treatment.
Finally, the relationship of CT scan results with the quality of CR rates and progression-free survival was assessed. The authors of a previous publication10 have shown that the addition of CT scans changed the CR rate but had no significant impact on progression-free survival rate. In contrast to our study this analysis included a smaller subset of patients (n = 82). The results presented here show a significant difference in progression-free survival between patients with CR confirmed by CT scan versus unconfirmed, if data from all 3 clinical trials were included. Interestingly, the difference disappeared, if progression-free survival for both CR definitions was evaluated only for the CLL8 trial comparing FC versus FCR. However, in the era of chemoimmunotherapy, where a substantial number of complete remissions is achieved, the use of 4-color flow cytometry for detecting minimal residual disease might be the method of choice to assess “true” complete remissions in CLL and be superior to imaging technologies.27 Taken together, the results provided by this meta-analysis suggest that imaging techniques such as CT scans, ultrasound, or chest radiographs provide only limited benefit for the evaluation of complete remission and follow-up of patients with CLL.
The online version of this article contains a data supplement.
Results from an interim analysis were presented, in part, at the 50th annual meeting of the American Society of Hematology, San Francisco, CA, December 6-9, 2008, as well as at the 13th International CLL Workshop, Barcelona, ESP, October 16-18, 2009.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
We thank Ute Elberskirch and Anne Westermann of the study office and Katrin Klein for data management.
This evaluation was supported by the German Cancer Aid (Deutsche Krebshilfe), grant number 106142 and the Competence Network Lymphoma (Bundesministerium für Bildung und Forschung), Cologne. The initial clinical trials were supported by Medac Schering Onkologie, Munich, and Hoffmann-La Roche Pharma AG, Basel.
Authorship
Contribution: B.F.E., K.F., A.-M.F., and T.E. supervised and monitored the trials; B.F.E., C.M.W., M.B., S.S., G.H., M.R., and M.H. were responsible for patient accrual, monitoring, and management of the clinical data at their referring center; J.B. and R.B. analyzed the trial; B.F.E., T.E., C.M.W., V.G., and M.H. contributed to the analysis; B.F.E. and M.H. wrote the report; M.H. acted as the sponsor and principal investigator and started the initiative for this analysis; and all authors critically contributed to the final preparation of the article.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Barbara Eichhorst, MD, Department I of Internal Medicine, Centre of Integrated Oncology Köln Bonn, University of Cologne, Kerpener Strasse 62, D-50924 Köln, Germany; e-mail: barbara.eichhorst@uk-koeln.de.