Abstract
Gaucher disease, caused by a deficiency of the lysosomal enzyme glucocerebrosidase, leads to prominent glucosylceramide accumulation in lysosomes of tissue macrophages (Gaucher cells). Here we show glucosylsphingosine, the deacylated form of glucosylceramide, to be markedly increased in plasma of symptomatic nonneuronopathic (type 1) Gaucher patients (n = 64, median = 230.7nM, range 15.6-1035.2nM; normal (n = 28): median 1.3nM, range 0.8-2.7nM). The method developed for mass spectrometric quantification of plasma glucosylsphingosine is sensitive and robust. Plasma glucosylsphingosine levels correlate with established plasma markers of Gaucher cells, chitotriosidase (ρ = 0.66) and CCL18 (ρ = 0.40). Treatment of Gaucher disease patients by supplementing macrophages with mannose-receptor targeted recombinant glucocerebrosidase results in glucosylsphingosine reduction, similar to protein markers of Gaucher cells. Since macrophages prominently accumulate the lysoglycosphingolipid on glucocerebrosidase inactivation, Gaucher cells seem a major source of the elevated plasma glucosylsphingosine. Our findings show that plasma glucosylsphingosine can qualify as a biomarker for type 1 Gaucher disease, but that further investigations are warranted regarding its relationship with clinical manifestations of Gaucher disease.
Introduction
Gaucher disease, a relatively common recessively inherited lysosomal storage disorder, is caused by a deficiency in the enzyme glucocerebrosidase, encoded by the GBA gene.1 Deficient enzymatic activity of glucocerebrosidase results in the lysosomal accumulation of its substrate glucosylceramide, most prominently in macrophages. Three variants of Gaucher disease are generally distinguished based on the absence (type 1) or presence of central nervous system involvement1 (types 2 and 3). In the much more common type 1 variant of Gaucher disease, glycosphingolipid-laden macrophages, referred to as Gaucher cells, accumulate in the visceral tissues liver, spleen, and bone marrow, inducing a pleiotropic array of symptoms, including hepatosplenomegaly and pancytopenia. In addition, type 1 Gaucher patients often develop bone complications: bone pain and crises, avascular necrosis, and pathologic fractures.1 Two different types of therapeutic intervention are available for type 1 patients. One relies on chronic intravenous administration of recombinant glucocerebrosidase, denoted enzyme replacement therapy (ERT).2 Two recombinant enzyme preparations are now registered for ERT in type 1 Gaucher disease: imiglucerase (Cerezyme; Genzyme Corp) and velaglucerase alfa (Vpriv; Shire HGT).3 A third enzyme, a plant-cell-expressed recombinant glucocerebrosidase, is under clinical development (Taliglucerase; Protalix/Pfizer).3 The other therapeutic intervention is based on oral administration of the iminosugar N-butyldeoxinojirimycin (Miglustat; Zavesca, Actelion).4 This compound is thought to effectively lower synthesis of the accumulating metabolite, glucosylceramide, by inhibiting its synthesizing enzyme, glucosylceramide synthase.5 The clinical responses to ERT are fast and impressive, such as significant corrections in hepatosplenomegaly, improvement of hematologic parameters and reduction of bone marrow infiltration as seen by magnetic resonance imaging.6 The response to miglustat treatment is less prominent, and its use is authorized for mildly to moderately affected patients who are unsuitable for ERT (EMA) or in whom ERT is not a therapeutic option (FDA).7 Future use of such small compounds for treating patients with a neuronopathic course of Gaucher disease is appealing given their potential to penetrate the brain (in contrast to recombinant enzyme).8 The availability of costly therapies has stimulated searches for plasma biomarkers that can assist in clinical management of individual patients. Several circulating protein markers for Gaucher cells have meanwhile been identified (for a review see Aerts et al9 ). It has been demonstrated that the enzyme chitotriosidase10 and the chemokine CCL1811 are produced by Gaucher cells and secreted into the circulation. Both proteins are candidate biomarkers since their plasma concentrations are markedly increased in symptomatic type 1 Gaucher patients and vary with disease progression as well as correction by therapeutic interventions.9 It has been known for a long time that type 1 Gaucher patients show increased levels of plasma and erythrocyte glucosylceramide.12 In addition, secondary increases in gangliosides and other glycolipids have been reported for plasma of type 1 Gaucher patients.13-15 Relatively little attention has been paid to these abnormalities as candidate biomarkers, since the cellular origin of the excessive circulating glycolipids is unclear. Also documented for several decades is the observation that a deacylated form of glucosylceramide, glucosylsphingosine, accumulates in tissues of Gaucher patients. Seminal investigations by Kanfer and colleagues and Svennerholm and coworkers revealed massively elevated glucosylsphingosine concentrations in brain of type 2 and 3 Gaucher patients, and to a lesser extent in type 1 Gaucher patients.16,17 More recently, Sidransky and colleagues reexamined glucosylsphingosine levels in relation to various variants of Gaucher disease.18 Over the years it has been repeatedly proposed that elevated glucosylsphingosine may underlie some clinical symptoms.19,20 For example, recent investigations with cultured osteoblasts of a type 1 Gaucher disease–like mouse model led to the hypothesis that glucosylsphingosine may actively contribute to low bone mineral density by interfering with normal osteoblast function,20 possibly by altered intracellular calcium homeostasis.21 In addition, a role for glucosylsphingosine in neurologic symptoms of Gaucher patients has been frequently proposed.18-20,22-24 Importantly, increased concentrations of other lysoglycosphingolipids have been documented for other lysosomal sphingolipidoses as well, such as galactosylsphingosine (psychosine) in Krabbe disease,24 and globotriaosylsphingosine (lysoGb3) in Fabry disease,25 each presumed to play an active role in disease related pathology.
Given the potential biologic significance of glucosylsphingosine and the successful development of a sensitive quantitative detection method, we investigated its plasma concentration in a cohort of type 1 Gaucher disease patients. Following our observation of a prominent increase in plasma glucosylsphingosine in patients, we examined its relationship with GBA genotypes and its correlation with clinical manifestations and established plasma markers of Gaucher cells. Corrections in plasma glucosylsphingosine levels after therapeutic interventions were also studied. Finally, the possible cellular source of glucosylsphingosine elevation was investigated. Here, we describe our findings which support plasma glucosylsphingosine as a candidate biomarker for type 1 Gaucher disease.
Methods
Materials and standards
LC-MS/MS grade MeOH, water, formic acid, and HPLC grade CHCl3 were purchased from Biosolve (Valkenswaard). Ammonium formate and glucosylsphingosine (D-glucosyl-β1-1′-D-erythro-sphingosine) were obtained from Sigma-Aldrich and Avanti Polar Lipids, respectively.
Patients and plasma samples
Diagnosis of Gaucher disease in patients was confirmed by genotyping and demonstration of deficient glucocerebrosidase activity in leucocytes or fibroblasts. EDTA plasma samples were collected before therapy from 50 Dutch patients (23 males, 27 females) suffering from Gaucher disease type 1, known by referral to the Academic Medical Center. Most patients were compound heterozygotes for the N370S and one other GBA mutation, with the exception of 5 patients homozygous for N370S. We also studied 14 homozygotes for the N370S mutation seen at the Yale Gaucher Clinic,2 patients suffering from saposin C deficiency seen at the Department of Pediatrics at the Children's Memorial Health Institute in Warsaw, 3 Gaucher disease type 3 patients, and 34 obligate carriers of Gaucher disease. Plasma samples were stored frozen at −20°C. Age-matched plasma samples from 14 male and 14 female healthy volunteers were obtained and treated likewise. Plasma was collected from patients receiving ERT (Ceredase, Cerezyme; Genzyme), and substrate deprivation therapy (Zavesca; Oxford Glycosciences). Eighteen patients had been splenectomized before therapy. Liver volume was measured as described previously.6 Clinical severity assessment at baseline was performed using a severity scoring index (SSI).6 Skeletal disease was defined as having a history of bone crises, avascular necrosis, or pathologic fractures, before therapy. Bone marrow fat fraction was assessed by Dixon quantitative shift imaging (QCSI) of the lumbar spine.6 Consent for use of stored plasma samples to study new biomarkers was obtained from all patients in accordance with the Declaration of Helsinki, and all experiments were approved by the Academic Medical Center of Amsterdam.
Sample preparation and LC-ESI-MS/MS quantification of glucosylsphingosine
Glucosylsphingosine was extracted using the method of Bligh and Dyer with an overall recovery of 89%. Briefly, 500 μL CHCl3/MeOH was added to 10 μL of plasma, in a 2:3 ratio (vol:vol), and samples were centrifuged for 3 minutes at 16 000g to remove protein precipitate. Subsequently, 100 μL CHCl3 and 260 μL MQ-H2O was added for phase separation. After vortexing and centrifugation for 3 minutes at 16 000g, the lower organic phase was collected, and upper phase reextracted with 300 μL CHCl3. Pooled lower phases were desiccated in a heat block set at (37°C) using mild N2 flow. Dried samples were redissolved in 100 μL MeOH, of which 10 μL was analyzed by LC-ESI-MS/MS using a BEH C18 Column and spiked glucosylsphingosine (Waters Corp). The exact procedure is described in detail in supplemental Methods (see the Supplemental Materials link at the top of the article).
Monocyte isolation and macrophage differentiation
Monocytes were isolated as described previously.26 For differentiation, monocytes were cultured for 4 days in RPMI 1640 (BioWhittaker) supplemented with 10% human serum (BioWhittaker). Phenotypical maturation was confirmed by light microscopy. After maturation, the medium was exchanged for X-VIVO 15 medium (Lonza) containing cyclophellitol epoxide BODIPY (MDW941; final concentration 500nM) for specific inhibition of glucosylceramide hydrolysis.27 At indicated time points, cells were washed 3 times and harvested for glucosylsphingosine and glycosphingolipid analysis. Glucosylceramide levels were quantified by HPLC according to Groener et al.14 Total protein concentrations were determined using the Bradford method with BSA as a standard.
Determination of Gaucher biomarkers
Statistical analyses
Results are presented as median and range. Mann-Whitney U testing was used for the following comparisons: Glucosylsphingosine levels of control subjects vs Gaucher patients and Gaucher patients with or without skeletal disease. All correlations were tested by the rank correlation test (Spearman coefficient, ρ). Results were considered to be statistically significant when 2-tailed P values were < .05.
Results
Quantification of plasma glucosylsphingosine by tandem mass spectrometry
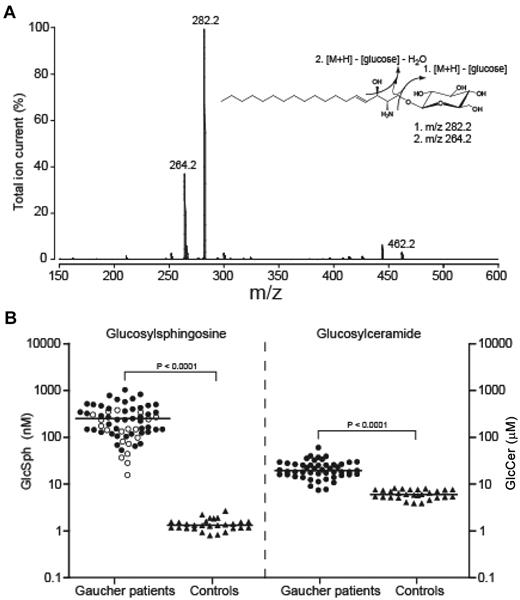
To investigate plasma glucosylsphingosine levels in type 1 Gaucher patients, an LC-tandem mass spectrometric assay was developed. First, optimal mass spectrometric settings were determined on direct infusion of glucosylsphingosine standard in positive ion mode. An abundant peak at m/z 464.2 was detected, consistent with a protonated form of glucosylsphingosine (M+H)+ (data not shown). Collision-induced fragmentation of glucosylsphingosine gave 2 stable product ions with m/z 264.2 and 282.2, corresponding to the loss of glucose with or without an H2O molecule, respectively (Figure 1A). Electrospray and collision settings were optimized for precursor-product fragmentation (m/z 464.2 > 282.2) and detection (see “Sample preparation and LC-ESI-MS/MS quantification of glucosylsphingosine”).
Quantification of glucosylsphingosine in plasma of type 1 Gaucher type patients. (A) Fragmentation spectrum of glucosylsphingosine. Predominant product ions (m/z 282.2 and 264.2) generated by collision induced fragmentation of glucosylsphingosine (m/z 464.2) are indicated. (B) Diagnostic value of glucosylsphingosine in type 1 Gaucher disease. Glucosylsphingosine and glucosylceramide levels in plasma of type 1 Gaucher patients (n = 64 and n = 49, respectively) and controls (n = 28). Patients homozygous for the mutation N370S are indicated with open circles (n = 19). Lines represent the median value in each group.
Quantification of glucosylsphingosine in plasma of type 1 Gaucher type patients. (A) Fragmentation spectrum of glucosylsphingosine. Predominant product ions (m/z 282.2 and 264.2) generated by collision induced fragmentation of glucosylsphingosine (m/z 464.2) are indicated. (B) Diagnostic value of glucosylsphingosine in type 1 Gaucher disease. Glucosylsphingosine and glucosylceramide levels in plasma of type 1 Gaucher patients (n = 64 and n = 49, respectively) and controls (n = 28). Patients homozygous for the mutation N370S are indicated with open circles (n = 19). Lines represent the median value in each group.
Next, efficacy of the Bligh and Dyer procedure for extraction of glucosylsphingosine from plasma samples was examined using serial dilutions of pure glucosylsphingosine standard (range 0-2μM) added to human plasma. Calibration lines were linear over the range of 0-2μM, covering all glucosylsphingosine concentrations present in plasma samples of controls and Gaucher patients (data not shown). The overall recovery was 89% (n = 10). To determine the intra- and inter-assay variation, a fixed amount of 10 pmol glucosylsphingosine was added to 10 μL human plasma. The intra-assay variation (3%, n = 6) was determined by analyzing a pooled sample in one batch, whereas the inter-assay variation (6.8%, n = 6) was determined by analyzing individually prepared samples in different runs over different days. The limit of quantification for plasma-derived glucosylsphingosine was only 0.3nM.
Plasma glucosylsphingosine in healthy subjects and Gaucher patients
Glucosylsphingosine and glucosylceramide levels were determined in plasma samples obtained from 28 control subjects and 64 Dutch type 1 Gaucher patients (including 14 additional patients seen at the Yale Gaucher Clinic) before, or not receiving, therapy (Figure 1B). In plasma of all type 1 Gaucher patients, glucosylsphingosine was increased on average > 200-fold (median 230.7nM, range 15.6-1035.2nM). Only trace amounts of glucosylsphingosine were present in plasma of control subjects (median 1.3nM, range 0.8-2.7nM). In comparison, glucosylceramide was also found to be significantly increased in Gaucher plasma, but only by a factor of 3 (Gaucher, median 17.9μM, range 7.0-54.2μM; Controls, median 5.7μM; range 3.7μM-7.6μM). In contrast to glucosylceramide levels, no overlap was observed between ranges of glucosylsphingosine levels for Gaucher samples and controls.
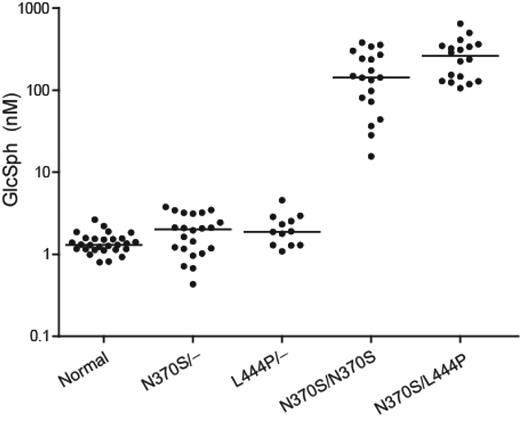
Plasma glucosylsphingosine and glucocerebrosidase genotype
Next, we determined plasma glucosylsphingosine concentrations in obligate Gaucher disease carriers, patients homozygous for the mild glucocerebrosidase N370S amino acid substitution and compound heterozygotes with N370S and L444P substitutions. Figure 2 shows that glucosylsphingosine plasma levels of obligate Gaucher carriers are not significantly elevated. In plasma of 19 examined N370S GBA homozygous individuals, the increase in plasma glucosylsphingosine was lower on average than in plasma of N370S/L444P glucocerebrosidase patients (P = .05). Within the group of N370S GBA homozygous patients, a clear relation between disease severity and glucosylsphingosine levels was observed (data not shown).
Plasma glucosylsphingosine levels in relation to GBA genotype. Glycolipid concentration was determined in plasma samples collected before initiation of therapy. Controls (n = 28), N370S heterozygotes (n = 22), L444P heterozygotes (n = 12), N370S homozygotes (n = 19), and N370S/L444P compound heterozygotes (n = 18).
Plasma glucosylsphingosine levels in relation to GBA genotype. Glycolipid concentration was determined in plasma samples collected before initiation of therapy. Controls (n = 28), N370S heterozygotes (n = 22), L444P heterozygotes (n = 12), N370S homozygotes (n = 19), and N370S/L444P compound heterozygotes (n = 18).
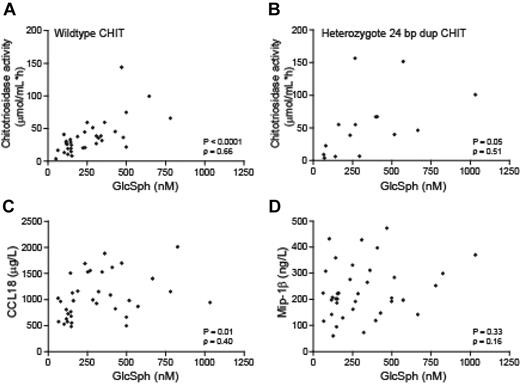
Correlation of plasma glucosylsphingosine with established plasma markers of Gaucher cells, chitotriosidase, and CCL18
The excessive chitotriosidase and CCL18 concentrations in plasma of symptomatic Gaucher patients both stem from Gaucher cells.30 We investigated the correlation between plasma glucosylsphingosine and these 2 established Gaucher cell markers. For measurement of chitotriosidase, an improved substrate was used for which both G102-chitotriosidase and the polymorphic S102-chitotriosidase show similar specific activity.31 In addition, chitotriosidase genotypes were determined with respect to the 24 bp duplication resulting in absence of protein production.32 In patients with wild-type chitotriosidase genotype a significant correlation was found between plasma glucosylsphingosine and chitotriosidase (ρ = 0.66; P < .0001; Figure 3A). Significance was less robust in Gaucher patients with the 24 bp duplication in one allele of the chitotriosidase gene (ρ = 0.51; P = .05; Figure 3B). Plasma glucosylsphingosine also correlated with CCL18 levels, albeit to a lesser extent (ρ = 0.40; P = .01; Figure 3C).
Relation between plasma glucosylsphingosine levels and established Gaucher biomarkers. Correlation between plasma glucosylsphingosine and chitotriosidase activity in type 1 Gaucher patients with wild-type CHIT genotype (n = 34; A) and carriers of the 24 bp duplication in the CHIT gene (n = 15; B). Correlation of plasma glucosylsphingosine level of type 1 Gaucher patients and cytokine CCL18 (n = 36; C) and macrophage inflammatory protein MIP-1β (n = 37; D).
Relation between plasma glucosylsphingosine levels and established Gaucher biomarkers. Correlation between plasma glucosylsphingosine and chitotriosidase activity in type 1 Gaucher patients with wild-type CHIT genotype (n = 34; A) and carriers of the 24 bp duplication in the CHIT gene (n = 15; B). Correlation of plasma glucosylsphingosine level of type 1 Gaucher patients and cytokine CCL18 (n = 36; C) and macrophage inflammatory protein MIP-1β (n = 37; D).
No correlation between plasma glucosylsphingosine and MIP-1β
Previously, van Breemen and colleagues reported markedly elevated levels of the chemokines MIP-1α and MIP-1β in plasma of symptomatic Gaucher patients.29 This finding has recently been confirmed in an independent investigation.33 The MIP proteins were found to be produced by surrounding inflammatory spleen macrophages and not by mature Gaucher cells.29 This different cellular source is also reflected in the observation that corrections in plasma MIP-1α and MIP-1β afterERT are not proportional to those of the Gaucher cell markers chitotriosidase and CCL18.34 We observed no correlation of plasma glucosylsphingosine with MIP-1β levels (Figure 3D).
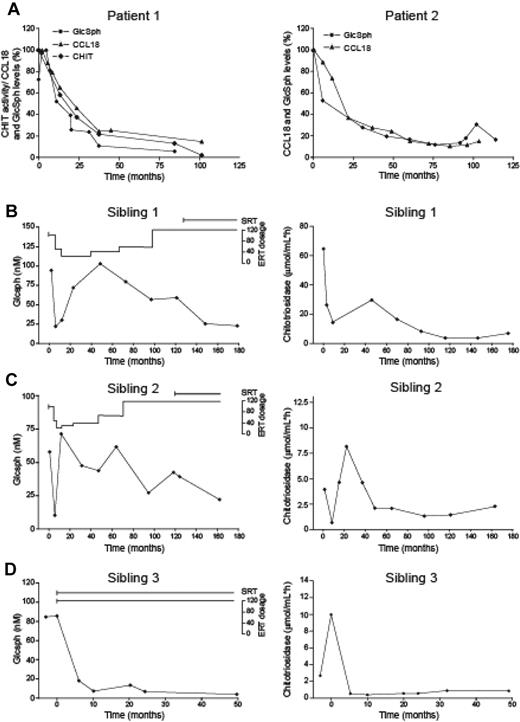
Effect of therapy on plasma glucosylsphingosine levels
Enzyme therapy with mannose-terminated recombinant enzyme results in supplementation of mannose-receptor containing macrophages with lysosomal glucocerebrosidase activity. The treatment results in rapid and pronounced reduction of Gaucher cells in various tissues and bone marrow.1,2,6 Changes in plasma glucosylsphingosine for 2 patients (responding well to ERT) are presented in Figure 4A. Plasma chitotriosidase and CCL18 were comparably reduced.
Response to therapy. (A) Characteristic reduction in plasma glucosylsphingosine, chitotriosidase and CCL18 in 2 type 1 Gaucher patients after enzyme therapy. Reductions are expressed as percentage of amount at start of treatment. Patient with wild-type chitotriosidase genotype (left panel); patient homozygous for a 24 bp duplication in the chitotriosidase gene, lacking chitotriosidase activity (right panel). (B-D) Changes in plasma glucosylsphingosine (left panels) and chitotriosidase (right panels) levels in 3 siblings suffering from type 3 Gaucher disease after enzyme replacement therapy (ERT; variable dosage) in combination with miglustat treatment (SRT). Patients received different combinations of enzyme replacement therapy and treatment with miglustat (3 × 100 mg/kg/d), starting at a very young age. The individual treatment regimens are indicated as ERT and SRT.
Response to therapy. (A) Characteristic reduction in plasma glucosylsphingosine, chitotriosidase and CCL18 in 2 type 1 Gaucher patients after enzyme therapy. Reductions are expressed as percentage of amount at start of treatment. Patient with wild-type chitotriosidase genotype (left panel); patient homozygous for a 24 bp duplication in the chitotriosidase gene, lacking chitotriosidase activity (right panel). (B-D) Changes in plasma glucosylsphingosine (left panels) and chitotriosidase (right panels) levels in 3 siblings suffering from type 3 Gaucher disease after enzyme replacement therapy (ERT; variable dosage) in combination with miglustat treatment (SRT). Patients received different combinations of enzyme replacement therapy and treatment with miglustat (3 × 100 mg/kg/d), starting at a very young age. The individual treatment regimens are indicated as ERT and SRT.
In addition, we analyzed plasma glucosylsphingosine levels in 3 siblings, 2 sisters, and 1 brother homozygous for the L444P glucocerebrosidase mutation and suffering from type 3 Gaucher disease. The oldest patient was diagnosed at 1.5 years of age and the younger siblings at birth. All received (different) combinations of enzyme and substrate reduction therapy, starting at a very young age. Clinical courses and treatment regimens have been described in detail by Cox-Brinkman et al.35 The analysis of plasma specimens (Figures 4B-D left columns) revealed that very early in life plasma glucosylsphingosine levels were already high when therapy was initiated. Negative effects of enzyme dose reduction on plasma glucosylsphingosine levels were detectable. The initiation of cotreatment with miglustat seemed to result in additional positive effects on plasma glucosylsphingosine concentrations in the first 2 children, although the data are limited. All these findings are similar to those observed for plasma chitotriosidase levels (Figures 4B-D right columns).
Marked reductions in glucosylsphingosine levels were observed in the majority of the type 1 Gaucher patients studied receiving enzyme replacement therapy (supplemental Figure 1A). However, we noted in the case of 5 Gaucher patients a poor response in plasma glucosylsphingosine, not coinciding with the reductions in chitotriosidase and CCL18 (supplemental Figure 1B). At present an explanation for this discrepancy is lacking. Compared with the average response to ERT, the impact of substrate reduction therapy with miglustat alone was less prominent in the 2 patients investigated: only a modest decline in elevated glucosylsphingosine (< 15%) was noted, even after a treatment period > 5 years (supplemental Figure 1C).
Correlation between plasma glucosylsphingosine and sphingolipids
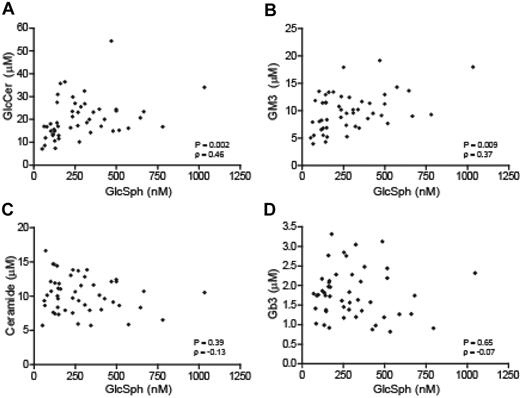
Glucosylceramide, the primary storage lipid in Gaucher disease, is also slightly elevated in the circulation, as it is present in lipoproteins.14,15 To investigate whether elevations in plasma glucosylceramide and glucosylsphingosine levels in Gaucher patients are related, we compared the concentrations of these lipids. The analysis revealed a significant correlation (P = .002; Figure 5A). Similarly, the ganglioside GM3, shown to be secondarily increased in plasma of Gaucher patients,15 also correlated with glucosylsphingosine when levels of these 2 lipids in plasma from individual Gaucher patients were compared (Figure 5B). No correlation of glucosylsphingosine was observed with ceramide, the hydrolytic product of glucosylceramide, or with the globoside Gb3 (Figure 5C-D).
Relation between plasma glucosylsphingosine levels and other sphingolipids. (A) Glucosylceramide; (B) Ganglioside GM3; (C) Ceramide; and (D) Globoside Gb3. (n = 49).
Relation between plasma glucosylsphingosine levels and other sphingolipids. (A) Glucosylceramide; (B) Ganglioside GM3; (C) Ceramide; and (D) Globoside Gb3. (n = 49).
Origin of elevated plasma glucosylsphingosine
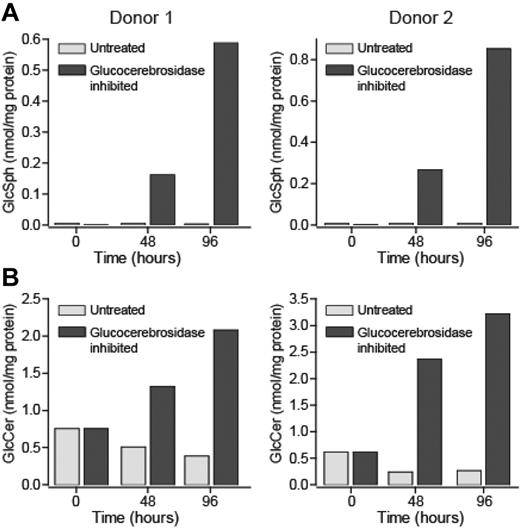
Our finding that the primary storage material in Gaucher cells, glucosylceramide, as well as plasma markers of Gaucher cells correlate strongly with plasma glucosylsphingosine levels, prompted us to investigate whether macrophages could be the source of the elevated plasma glucosylsphingosine in type 1 Gaucher patients. First, we studied whether macrophages can generate glucosylsphingosine. To this end, isolated monocytes from 2 healthy donors were differentiated into macrophages. Subsequently, part of the macrophage culture was incubated with a very specific suicide inhibitor27 of glucocerebrosidase, resulting in its complete inactivation. Glucosylceramide and glucosylsphingosine levels were analyzed in macrophages with and without active glucocerebrosidase at different time points (0-96 hours). Figure 6A shows that cultured macrophages with normal glucocerebrosidase activity (t = 0) contain only a trace of glucosylsphingosine. In contrast, glucosylceramide is quite abundant in the cells (Figure 6B). After inactivation of glucocerebrosidase, the cultured macrophages from both donors rapidly accumulate glucosylsphingosine, already within 24 hours (data not shown), which progressed markedly in the next 72 hours (Figure 6A). In comparison, inactivation of glucocerebrosidase resulted in a far more modest increase in glucosylceramide (Figure 6B). In spleens from 4 type 1 Gaucher patients the concentrations of glucosylceramide (28.1, 38.1, 35.8 and 17.0 mmol/kg wet weight) and glucosylsphingosine (11.8, 7.8, 15.6 and 17.8 μmol/kg) were concomitantly increased compared with the concentrations of glucosylceramide (0.03 and 0.02 mmol/kg) and glucosylsphingosine (0.03 and 0.14 μmol/kg) in the spleens from 2 normal subjects. These data support the idea that Gaucher cells are the source of glucosylsphingosine.
Accumulation of glucosylceramide and glucosylsphingosine in cultured macrophages afterinactivation of glucocerebrosidase. Macrophages were differentiated from peripheral blood monocytes obtained from 2 different donors. After 7 days of culture, glucocerebrosidase was irreversibly inactivated for 4 days with an excess of the suicide inhibitor MDW941. Cells were harvested at indicated time points, and glucosylsphingosine (A) and glucosylceramide content (B) determined.
Accumulation of glucosylceramide and glucosylsphingosine in cultured macrophages afterinactivation of glucocerebrosidase. Macrophages were differentiated from peripheral blood monocytes obtained from 2 different donors. After 7 days of culture, glucocerebrosidase was irreversibly inactivated for 4 days with an excess of the suicide inhibitor MDW941. Cells were harvested at indicated time points, and glucosylsphingosine (A) and glucosylceramide content (B) determined.
Correlation of plasma glucosylsphingosine with disease parameters
Plasma glucosylsphingosine concentrations in untreated type 1 Gaucher patients were compared with overall disease severity of individuals as assessed with the generally used SSI.6 No significant correlation was found (ρ = 0.23; P = .13, Figure 7A). No significant difference in plasma glucosylsphingosine levels was found in samples obtained from patients without (n = 18) and with a spleen (n = 32; data not shown). A significant correlation was noted between plasma glucosylsphingosine and liver volume (ρ = 0.57; P < .0001; Figure 7B). We also compared levels of glucosylsphingosine in Gaucher patients with and without skeletal complications. No significant differences were found between both groups (Figure 7C). One of the proposed inducers of skeletal disease in Gaucher patients is the presence of Gaucher cells in the bone marrow, leading to the displacement of adipocytes.36 Previously we reported that in our cohort of Gaucher patients, the lumbar marrow fat fraction, as measured by quantitative chemical shift imaging (QCSI), is significantly lower in Gaucher patients compared with control individuals: patients (mean 20%, range 8%-40%), controls (mean 37%, range 27-0.55%).36 When analyzing the entire group of patients, a significant correlation was observed between plasma glucosylsphingosine levels and bone marrow fat fraction (ρ = −0.43; P = .01; Figure 7D). It has recently been hypothesized that glucosylsphingosine negatively influences osteoblasts so that abnormally high levels might contribute to the osteopenic nature of bone of Gaucher patients.20 We therefore compared the levels of glucosylsphingosine with those of 2 specific bone formation markers, ie osteocalcin and bone-specific alkaline phosphatase (P1NP), in plasma of Gaucher patients. A negative relation was observed between plasma glucosylsphingosine and osteocalcin (ρ = −0.22; P = .30). A similar negative trend, though again not reaching significance, was observed between plasma glucosylsphingosine and P1NP (ρ = −0.21; P = .33; Figure 7E-F). Patients with higher levels of osteocalcin and P1NP in or close to the normal range tended to show relatively low plasma glucosylsphingosine levels. A comparison between bone mineral density in Gaucher patients before treatment and their corresponding plasma glucosylsphingosine levels was not feasible because of a lack of sufficient pre-treatment data.
Relation between plasma glucosylsphingosine and disease manifestations or bone marrow markers. (A) Plasma glucosylsphingosine and disease severity score (SSI; n = 46). (B) Plasma glucosylsphingosine and liver volume (n = 45). (C) Plasma glucosylsphingosine and skeletal disease (n = 48). (D) Plasma glucosylsphingosine and bone marrow fat fraction (n = 34). (E) Plasma glucosylsphingosine and osteocalcin (n = 24). (F) Plasma glucosylsphingosine and P1NP (n = 24).
Relation between plasma glucosylsphingosine and disease manifestations or bone marrow markers. (A) Plasma glucosylsphingosine and disease severity score (SSI; n = 46). (B) Plasma glucosylsphingosine and liver volume (n = 45). (C) Plasma glucosylsphingosine and skeletal disease (n = 48). (D) Plasma glucosylsphingosine and bone marrow fat fraction (n = 34). (E) Plasma glucosylsphingosine and osteocalcin (n = 24). (F) Plasma glucosylsphingosine and P1NP (n = 24).
Discussion
Here we report on the marked increase in concentration of plasma glucosylsphingosine in symptomatic Gaucher disease patients. This abnormality may have gone unnoticed because of the previously cumbersome procedures for quantification of glucosylsphingosine. Existing detection methods are based either on thin-layer chromatography with subsequent staining, or on high-performance liquid chromatography, often in combination with derivatization with fluorescent agents to increase detection sensitivity. Here we introduce a rapid mass spectrometric detection method allowing accurate quantification of glucosylsphingosine at nanomolar concentrations in plasma. Our method can be further improved by the use of stable isotope-labeled glucosylsphingosine as internal standard. Large-scale synthesis of 5,6,7,8,9 13C5-glucosylsphingosine is presently undertaken for this purpose.
The elevation of glucosylsphingosine in Gaucher patients has been observed previously. The pioneering investigations by Raghavan and colleagues16 and those by Svennerholm and coworkers17 already led to the notion that glucosylsphingosine is elevated in tissues (particularly brain), of type 2 and 3 Gaucher patients and to a lesser extent in tissues from type 1 Gaucher patients. To the best of our knowledge the average 200-fold elevated plasma glucosylsphingosine in type 1 Gaucher patients has not been reported previously.
The abnormality in circulating glucosylsphingosine in type 1 Gaucher patients is of interest for several reasons which each warrant discussion. In the first place, elevated plasma glucosylsphingosine might offer a convenient additional biomarker to monitor disease progression and correction aftertherapeutic intervention. Possibly, it may also assist clinicians in decision making on initiation of therapy and optimizing individual dosing regimens. To test the potential of plasma glucosylsphingosine as biomarker, we studied several relationships. First, we observed that the plasma glucosylsphingosine level is related to glucocerebrosidase deficiency. Plasma glucosylsphingosine levels are not significantly increased in heterozygotes. Patients with less severe disease generally show more modest increases in plasma glucosylsphingosine. This is also reflected by the finding that homozygotes for N370S, generally presenting a more benign course of disease,37 show in general lower increases of glucosylsphingosine than compound heterozygotes for the N370S and L444P glucocerebrosidase mutations. In addition, within the group of N370S glucocerebrosidase homozygous patients a clear relation between disease severity and glucosylsphingosine levels was observed. The relatively common N370S glucocerebrosidase mutation encodes an enzyme with almost normal routing to lysosomes and considerable residual activity38 whereas the L444P glucocerebrosidase mutation encodes an enzyme that largely folds incorrectly and is prematurely degraded by proteasomes.39 Second, we observed clear correlations between plasma glucosylsphingosine levels and established plasma markers of Gaucher cells. These lipid-laden macrophages are present in various tissues, including liver, spleen, lung and bone marrow, and are thought to drive pathology. The Gaucher cells are known to massively produce and secrete the enzyme chitotriosidase and cytokine CCL1830 into the circulation. These proteins are present in highly elevated concentrations in plasma and their levels have been shown to correlate with the major manifestations of disease such as splenomegaly, hepatomegaly and hematologic abnormalities.40,41 Plasma glucosylsphingosine, chitotriosidase, and CCL18 diminish comparably in the majority of patients during enzyme therapy. This suggests that the visceral Gaucher cells are the main source of glucosylsphingosine. The specificity of elevated plasma glucosylsphingosine for Gaucher disease has not been extensively examined yet. No abnormalities were noted in plasma obtained from Fabry disease patients or individuals suffering from sarcoidosis, both conditions in which chitotriosidase is modestly elevated. All our findings so far support the idea that plasma glucosylsphingosine is an appealing specific candidate biomarker for type 1 Gaucher disease.
The precise biochemical pathway(s) contributing to formation of glucosylsphingosine in Gaucher patients are unknown. Glucosylceramide synthase is believed to catalyze not only the biosynthesis of glucosylceramide from ceramide and UDP-glucose but also that of glucosylsphingosine.42 Of interest, we observed a prominent generation of glucosylsphingosine in human blood monocyte-derived macrophages when incubated with a specific glucocerebrosidase inhibitor. In the first 2 days after glucocerebrosidase inactivation, the absolute amount of accumulated glucosylsphingosine was only 25% (donor A) and 15% (donor B) compared with that of the accumulating glucosylceramide. In the subsequent 2 days, glucosylceramide increased almost linearly, while the accumulation of glucosylsphingosine accelerated to 70% (donor A) and 40% (donor B). Although glucocerebrosidase is able to degrade glucosylsphingosine, the kcat is a 100-fold lower than for glucosylceramide,43,44 making it less likely that the absence of this function is a major contributor to the increase in glucosylsphingosine levels. We hypothesize that after glucocerebrosidase inactivation, glucosylceramide (and possibly some glucosylsphingosine) indeed accumulate because of impaired degradation by glucocerebrosidase. Most of the glucosylsphingosine, however, seems to result from deacylation of the accumulating glucosylceramide. Such a pathway has earlier been proposed by Yamaguchi and colleagues.45 Summarizing, our data suggest that glucosylsphingosine is largely a direct derivative of the primary storage product glucosylceramide produced by the Gaucher cell.
To obtain further insight in the metabolism of glucosylsphingosine, we studied patients suffering from a saposin C deficiency.46 We speculated that the hydrolysis of the water-soluble glucosylsphingosine by glucocerebrosidase may not require saposin.47 However, glucosylsphingosine (258 and 290nM) and glucosylceramide (13 and 17μM) concentrations in plasma specimens of 2 saposin C deficient patients were comparable with those in type 1 Gaucher patients. As such, this finding does not address the possibility that deacylation of accumulating glucosylceramide is a major pathway for formation of excessive glucosylsphingosine in Gaucher patients. However, it is consistent with our idea that excessive glucosylsphingosine is not a direct result from impaired breakdown. Using cultured fibroblasts, Yamaguchi and colleagues showed that accumulated glucosylceramide can be actively deacylated to glucosylsphingosine, likely involving the lysosomal enzyme acid ceramidase.45 This finding warrants further investigation regarding the role of this enzyme in glucosylsphingosine metabolism in Gaucher disease.
High concentrations of circulating glucosylsphingosine in type 1 Gaucher patients raise the question whether this lysoglycosphingolipid has direct harmful consequences. Numerous reports indicate that glucosylsphingosine (glucopsychosine) is cytotoxic.18-20,22,23 For example, glucosylsphingosine is reported to cause hemolysis of red blood cells at low concentrations48 and inhibit protein kinase C49 , a pivotal kinase in signal transduction and cell behavior. In addition, it has been shown that glucosylsphingosine damages cholinergic neurons.19 The toxic effects of the closely related galactosylsphingosine (psychosine), which is elevated in Krabbe disease (globoid cell leukodystrophy), have been studied in more detail (for a review see Ballabio et al23 ). It activates the TDAG8 receptor, causing inhibition of cytokinesis and the characteristic formation of giant multinuclear globoid cells. Inhibition of protein kinase C by psychosine is thought to disturb normal functioning of oligodendrocytes and Schwann cells. The lysosphingolipid is believed to also interfere with IGF-1 signaling and consequent oligodendrocyte development. In addition, psychosine reduces AMP activated kinase activity, favoring energy consuming over energy generating pathways.23 Finally, psychosine activates phospholipase A2, increasing lysophosphatidylcholine production and release of arachidonic acid. Interestingly, glucosylsphingosine has also been reported to activate phospholipase A2 and to inhibit CTP:phosphocholine cytidylyl-transferase activity, the rate limiting step in phosphatidylcholine synthesis.23 Since phosphatidylcholine is a major membrane lipid, glucosylsphingosine-induced changes in its biosynthesis may be of pathogenic relevance.
Given the potential toxic effects of glucosylsphingosine, we compared plasma levels with clinical symptoms in Gaucher patients. The composite severity scoring index to assess overall disease severity was found to correlate only poorly with plasma glucosylsphingosine concentrations. This is not surprising since past complications make large contributions to this score. In contrast, another clinical parameter, hepatomegaly, correlated well with plasma glucosylsphingosine concentrations. A third, important, clinical symptom of Gaucher disease is skeletal illness. In a recent study it was shown that glucosylsphingosine interferes with osteoblast function.20 When we divided Gaucher patients into those with and without skeletal complications (defined as a history of bone crises, avascular necrosis, or pathologic fractures), no strict correlation with plasma glucosylsphingosine was apparent. However, the bone marrow fat fraction, as measured by quantitative chemical shift imaging of the lumbar spine (QCSI), did correlate with plasma glucosylsphingosine levels, indicating that increasing infiltration with Gaucher cells is reflected by higher glycolipid levels. Our observation that patients with higher, (near) normal levels of the bone formation markers osteocalcin and P1NP show relatively low plasma glucosylsphingosine levels is of interest and consistent with the hypothesis that glucosylsphingosine influences osteoblast proliferation and differentiation.20 A thorough investigation regarding the relationship between plasma glucosylsphingosine concentration and bone mineral density in therapy-naive Gaucher patients should be undertaken.
We have described the marked increase in globotriaosylsphingosine (lysoGb3) in patients suffering from Fabry disease, an X-linked disorder caused by α-galactosidase A deficiency.25 Afterenzyme therapy, the accumulated lysoGb3 levels in Fabry disease react very differently from glucosylsphingosine in Gaucher disease. Plasma glucosylsphingosine in most Gaucher patients tends to show a sustained decrease over years of enzyme therapy. However, a rapid reduction in plasma lysoGb3 is observed within the first 3 months of enzyme therapy, followed by stabilization of levels. Enzyme therapy of male Fabry patients can result in a reduction of lysoGb3 by ∼ 70%. This reduction is only ∼ 25% in the majority of male Fabry patients, who develop antibodies against the therapeutic recombinant α-galactosidase A.50
In conclusion, our present investigation documents a marked elevation in plasma concentration of glucosylsphingosine in symptomatic Gaucher patients. Gaucher cells seem to be a likely major source for this phenomenon. Given the potential toxic effects of glucosylsphingosine, further investigations regarding its role in pathophysiologic processes in Gaucher patients are needed.
This article contains a data supplement.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Acknowledgments
The authors acknowledge the Dutch Gaucher patients and the VKS-GVN for their longstanding support and help. They thank Dr Roscoe Brady for stimulating discussions over many years on the role of sphingosines in lysosomal storage disorders. This study is dedicated to the memory of Professor Joseph Tager, recently deceased, one of the founding fathers of research on lysosomal storage disorders.
Authorship
Contribution: N.D., L.v.D., S.S., K.G., M.J.v.B., M.J.F., H.O., and M.M. performed research; N.D. analyzed the data and performed statistical analysis; N.D., R.G.B., and J.M.A. designed research; C.E.M.H., J.E.M.G., F.W., A.T., and P.K.M. provided plasma samples; and N.D., D.S., and J.M.A. wrote the manuscript.
Conflict-of-interest disclosure: J.M.A. has received an unrestricted joint study grant from Genzyme Corporation and Shire HGT to investigate lysoGb3 in Fabry plasma specimens. Both pharmaceutical companies produce drugs for enzyme replacement therapy of Fabry disease. C.E.M.H. and J.M.A have received reimbursements of expenses and honoraria for lectures on lysosomal storage diseases from Genzyme Corporation, Shire HGT and Actelion. Honoraria have been transferred to the Gaucher Stichting, a foundation that supports research in the field of lysosomal storage disorders. The remaining authors declare no competing financial interests.
Correspondence: J. M. Aerts, Department of Medical Biochemistry, Academic Medical Center, Meibergdreef 15, 1105 AZ Amsterdam, The Netherlands; e-mail: j.m.aerts@amc.uva.nl.