Abstract
Abstract 2192
To activate clot formation and maintain hemostasis, platelets adhere and spread onto sites of vascular injury. Although well-characterized biochemically, the role of physical and spatial cues in the microenvironment affect platelet adhesion and spreading remains unclear. No published data systemically characterizes and quantifies, at the single platelet level, how the microenvironmental geometry influences platelet spreading, and what the physical limitations and constraints are. In this study, we applied protein microcontact printing techniques to quantitatively investigate the extent of spatial regulation, if any, during platelet spreading.
This concept of physical and microenvironmental control of platelet function is important to our understanding of platelet physiology and clot formation. Indeed, as fibrin formation takes place on the surface of activated platelets, investigation into the spatial regulation of platelet spreading will provide valuable insight into how clot formation itself is regulated and may have implications in bleeding and thrombotic disorders.
To enable submicron resolution of single platelet adhesion and spreading, microfabricated features were created on silicon chips using deep UV photolithography. Micropatterns of Type I collagen-FITC or fibrinogen-Alexa 488 on glass coverslips were created using microcontact printing.1 Platelets were then incubated on the protein micropattern for 1 to 2 hours and monitored using confocal microscopy.
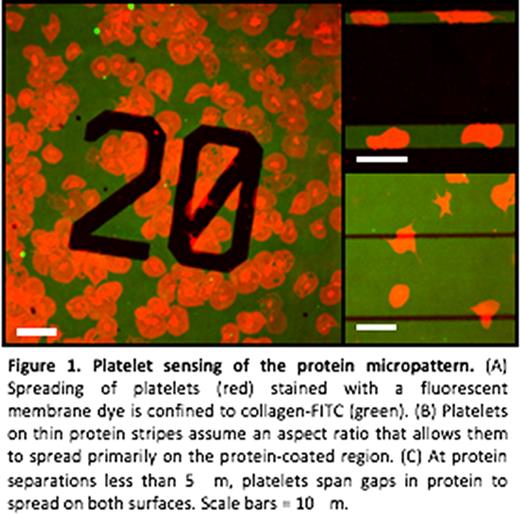
Platelet sensing of the protein micropattern. (A) Spreading of platelets (red) stained with a fluorescent membrane dye is confined to collagen-FITC (green). (B) Platelets on thin protein stripes assume an aspect ratio that allows them to spread primarily on the protein-coated region. (C) At protein separations less than 5 mm, platelets span gaps in protein to spread on both surfaces. Scale bars = 10 mm.
Platelet sensing of the protein micropattern. (A) Spreading of platelets (red) stained with a fluorescent membrane dye is confined to collagen-FITC (green). (B) Platelets on thin protein stripes assume an aspect ratio that allows them to spread primarily on the protein-coated region. (C) At protein separations less than 5 mm, platelets span gaps in protein to spread on both surfaces. Scale bars = 10 mm.
We observed that the fidelity of platelet spreading decreases with feature sizes below 5 μm, likely due to the mass effect of the platelet itself. However, as platelets extend filopodia, they “bridge” and spread over non-protein patterned areas of up to 5 μm in distance. Taken together, our data quantifies the extent of spatial regulation during platelet spreading and has important implications in our understanding of clot formation. Biochemically, hemostasis is tightly controlled via multiple feedback mechanisms. Our observations suggest that this platelet adhesion and spreading is also highly spatially controlled, thereby potentially providing another mechanism by which hemostatic plug formation occurs only at sites of vascular injury. The capability of platelets to span <5 μm distances may imply that spatial guidance is less important for micron-scale, subclinical sites of vascular injury. Ongoing efforts focus on 1) investigating on how flow affects these phenomena and 2) how the microenvironmental geometry affects biological processes within the platelet such as actin and tubulin rearrangement, calcium signaling, and phosphatidyl serine exposure.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.