Abstract
Abstract 2484
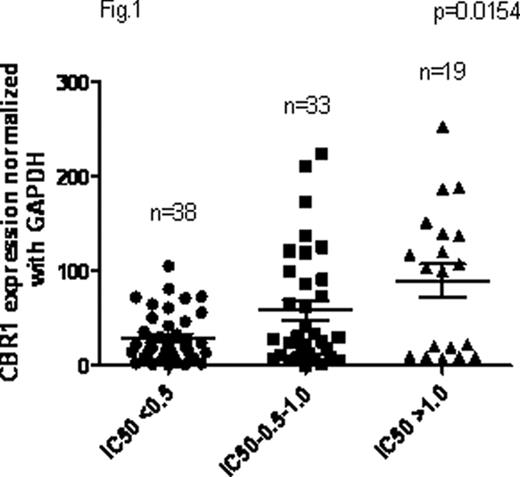
Treatment failure in AML can be attributed to resistance to chemotherapeutic drugs. Induction chemotherapy of AML involves combination of Daunorubicin (Dnr) and Cytarabine. Up-regulation in the expression of efflux transporters such as ABCB1 and ABCG2 has been shown to be one of the causes of Dnr resistance in AML. Apart from efflux transporters, increased expression of the Dnr metabolising enzymes (Carbonyl reductase 1 (CBR1) and CBR3) also can influence the cytotoxic activity of Dnr against leukemic cells. Aim of the present study is to investigate: i) the role of mRNA expression of Dnr metabolising enzymes (CBR1 and CBR3) on the in vitro cytotoxicity of Dnr in primary AML cells and ii) effect of Single nucleotide polymorphisms (SNPs) in CBR1 and CBR3 on the plasma pharmacokinetics of Dnr and Daunorubicinol (DOL) in AML patients.
Ninety patients with AML (excluding AML-M3) at diagnosis before the initiation of therapy were included. Bone marrow (BM) was collected at diagnosis and blast percentage in our cohort of patients ranged from 20–100%. Mononuclear cells (MNCs) were isolated by density gradient centrifugation. Total RNA was extracted from BMMNCs and cDNA was prepared. CBR1 and CBR3 mRNA expression was measured using Taqman based quantitative RT-PCR normalized to GAPDH. In-vitro cytotoxicity of Dnr was determined by MTT cell viability assay. Intracellular levels of Dnr and DOL was estimated by HPLC coupled with Fluorescence detector (FD). SNPs in CBR1 and CBR3 were screened by PCR followed by sequencing. In addition, plasma samples during Dnr infusion was collected at 0, 1, 2, 4, 6 and 24hrs from 24 of the 90 AML patients. Levels of Dnr and DOL in the plasma samples were estimated by HPLC coupled with FD and Area under Curve (AUC) for Dnr and DOL were calculated.
Five SNPs in CBR1 and 3 in CBR3 were identified. CBR1 SNPs, rs20572, rs9024 and rs25678 were in complete linkage disequilibrium (LD). Variant of rs25678 and rs20572/rs9024 had an allelic frequency of 0.244 and 0.20 respectively. Among CBR3 SNPs, variants of two non-synonymous polymorphisms rs8133502 and rs1056892 showed allelic frequency of 0.31 and 0.51 respectively. AUC of Dnr and DOL in plasma samples ranged from 22–2474ng*h/ml and 37–2027 ng*h/ml respectively while clearance of Dnr ranged from 0.04 to 3.34 L/h. Plasma DOL AUC, unlike in vitro intracellular DOL, did not show any significant association with CBR1 and CBR3 expression. In patients with variant rs25678 genotype, Dnr AUC was higher and clearance was lower compared to the wild type genotype, reaching a trend to statistical significance (p=0.0537 and 0.1184 for Dnr AUC and clearance). Influence of Dnr and DOL plasma levels on clinical outcome, if any, remains to be evaluated.
This is the first report showing the influence of CBR1 and CBR3 in in-vitro cytotoxicity of Dnr and role of SNPs in CBR1 and CBR3 in plasma pharmacokinetics of Dnr in AML patients. To conclude, higher expression of CBR1 confers resistance to Dnr in primary AML cells and polymorphisms of this gene may influence the pharmacokinetics of Dnr.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.