Abstract
Abstract 3093
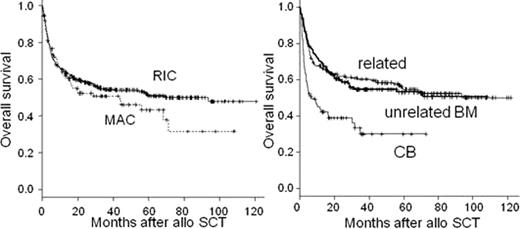
Allogeneic hematopoietic stem cell transplantation (allo SCT) is potentially curative treatment for relapsed follicular lymphoma (FL) that remains non-curative disease even with modern immunochemotherapy. Number of potential candidate of allo SCT for FL has been increasing with the development of reduced intensity conditioning (RIC) regimens and increased donor availability due to use of hematopoietic stem cell from unrelated donor including cord blood (CB). However, short-term and long-term transplantation-related complications are still major obstacles in applying this treatment. Recently, EBMT and CIBMTR reported a prognostic score of allo SCT for FL (Ann Oncol 2011;22 :Suppl 4, iv94). However, this score awaits validation. To elucidate prognostic factors for OS after allo SCT for FL, we conducted a retrospective study using the national registry data of the Japan Society of Hematopoietic Cell Transplantation (JSHCT). In total, 472 cases of allo SCT for FL performed from 2000 to 2008 were identified. 220 (46.6%) were male and the median age at allo SCT was 50 yo (range: 27–75). Forty six (9.7%) patients were 60 yo or older. Eighty two (17.3%) patients had previous history of autologous transplantation (ASCT). Stem cell source was BM or PB from related donor in 215 (45.5%), unrelated donor BM in 180 (38.1%), and unrelated donor umbilical cord blood (CB) in 77 (16.3%). Conditioning regimen was myeloablative (MAC) in 20.7% and reduced intensity (RIC) in 79.3%, respectively. Patients undergoing MAC were younger than those with RIC (45 vs 50 yo, P<0.01). T-cell depletion with ATG or ALG was performed in 7.5%. ECOG performance status (PS) at allo SCT was ≥ 2 in 10.7%. 71.5% had chemosensitive disease at allo SCT and disease status was CR in 38.9%. With a median follow up of 47.3 mo (range: 0.9–122) among survivors, overall survival rate at 4years after allo SCT (4y OS) was 52.6%. Patients who had CB transplantation had worse OS than those transplanted from related donor or unrelated BM (30.0%, 58.5%, 54.6%, P =1.35e-6, logrank). Additionally, in univariate analysis, PS ≥2, chemoresistant disease at allo SCT, older age, male sex were adverse prognostic factors for OS, while previous history of ASCT, time from diagnosis to allo SCT (<3y vs ≥3y), disease status at allo SCT (CR vs non CR), conditioning regimen (MAC vs RIC), and year of allo SCT (2000–2 vs 2003–5 vs 2006–8) were not. 4y OS of patients undergoing MAC and RIC were 46.2% and 54.0% (P =0.28), respectively. In multivariate analysis with proportional hazard modeling, PS ≥2 (HR 3.2, P =0.00015), chemorefractory disease (HR 2.7, P =0.039), and use of CB (HR 3.8, P =0.039) were independent adverse predictors of OS. Although risk factors that are incorporated in the proposed EBMT/CIBMTR risk score other than PS were not predictive of OS in the present analysis, we applied this score to the population of the present study. In the entire population, 4y OS were 61.0% and 38.5% (P =9.5e-08) in patients with the score <3 (n=294) and ≥3 (n=77), respectively. This score was predictive of OS in patients who underwent transplantation from related donor (65.4% vs 36.7%, P =3.77e-08) and from unrelated BM (59.0% vs 41.7%, P =0.0217). In conclusion, this retrospective study of JSHCT registry data showed that allo SCT for FL is a reasonable option for patients with relapsed FL when suitable donor is available. Poor PS, chemorefractory disease, and CB as donor source were adverse prognostic factors for OS.
Disclosures:
No relevant conflicts of interest to declare.
Author notes
*
Asterisk with author names denotes non-ASH members.
© 2011 by The American Society of Hematology
2011