Abstract
Abstract 4053
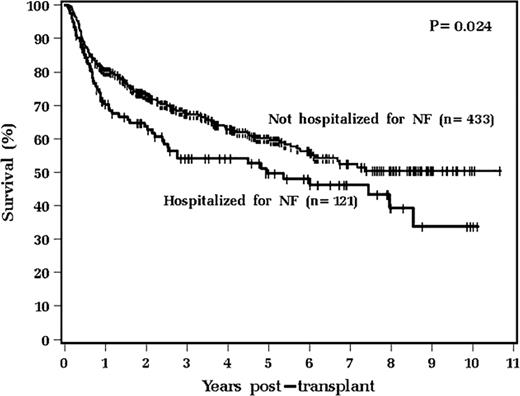
High-dose chemotherapy followed by autologous stem cell transplant can improve long-term outcome of patients with relapsed non-Hodgkin and Hodgkin lymphoma. Stem cell mobilization with chemotherapy in addition to G-CSF improves stem cell collection, however it is also associated with increased risk of neutropenic fever. We analyze whether hospitalization for neutropenic fever (NF) affects outcomes after transplantation.
From 1/1998 to 12/2008, 599 patients underwent chemotherapy priming with etoposide + G-CSF (27 patients also received rituximab). Forty five (8%) did not proceed to transplant. Of the 554 (92%) patients who were transplanted, the median age was 51 years, and 348 (63%) were male. The diagnoses were 422 non-Hodgkin lymphoma (63%) and 132 Hodgkin lymphoma (24%). A majority of these patients (92%) had received 3 or less prior chemotherapy regimens. Only 6% had been exposed to fludarabine therapy. Most patients had chemosensitive disease (88% were in CR or PR) at time of transplant. For preparative regimen: 517 (93%) received busulfan/etoposide/cyclophosphamide, 32 (5.8%) received melphalan, 5 (0.9%) received other chemotherapy.
In conclusion, admission for neutropenic fever during stem cell mobilization is associated with significantly increased number of apheresis days required for adequate stem cell collection, lower CD34+ cell collection, higher 30-day re-admission rates, and poorer survival.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.